Immature patients, abnormal neuroaxis, body habitus
1. Immature patients
Patients who are skeletally immature presenting for treatment of their AIS deformity merit special consideration. The degree of skeletal immaturity can be determined from their preoperative AP radiograph from observation of the triradiate cartilage (TRC) and from the Risser sign.
Details on patient examination
Patients with an open TRC are highly immature and thus have much growth remaining. Patients with a closed TRC along with a Risser zero are more mature but still undergoing skeletal maturation. Both of these groups are prone to progressive scoliosis deformity both within (crankshaft phenomemon) and outside their fused levels (adding on phenomenon) of the spine.
The following three considerations below should be taken into account.
Avoid short fusions in these patients
Selection of the Lowest Instrumented Vertebra (LIV) in these patients usually mandates fusion to the neutral and stable vertebra. This will prevent adding on phenomenon which occurs below a shorter fusion in immature patients. Adding on phenomenon usually requires revision surgery to extend the fusion level more distal in the spine following growth.
Consider ASF to remove anterior growth potential
A preliminary ASF procedure will remove the anterior growth potential of these immature patients thus making the posterior instrumentation and fusion more definitive. This will also eliminate the crankshaft phenomenon that often produces progressive three dimensional scoliotic deformity in immature patients treated with a PSF alone.
Consider segmental bilateral pedicle screw fixation to overcome the progressive anterior growth forces
Another technique to avoid the crankshaft phenomenon is to perform bilateral segmental pedicle screw fixation over the appropriate fusion levels of the spine in these immature patients.
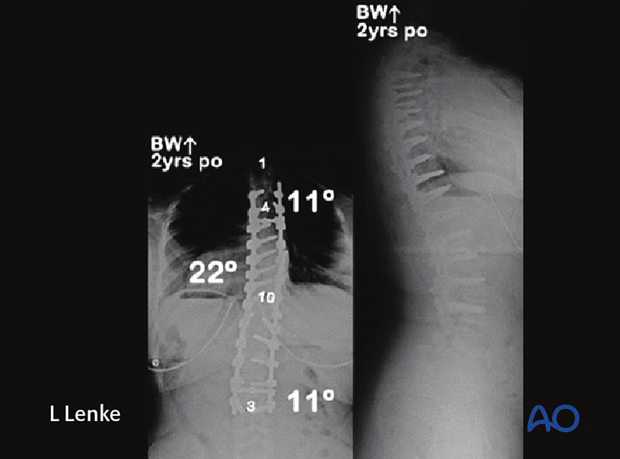
This is an 11 years, 3 months old female with a severe double major AIS deformity. Although her TRC's are closed, she is Risser zero and premenarcheal and thus highly immature and at risk for crankshaft phenomenon.
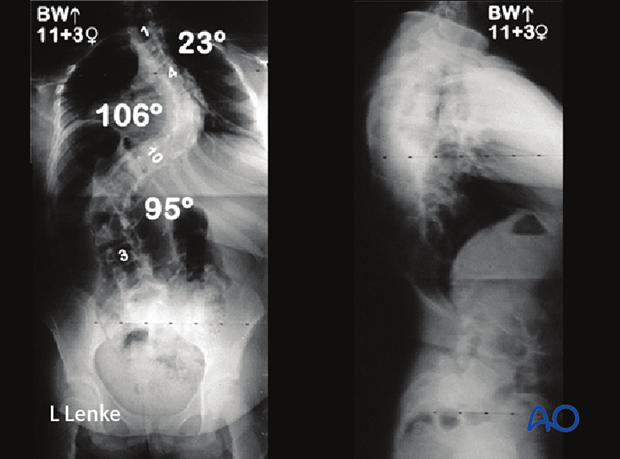
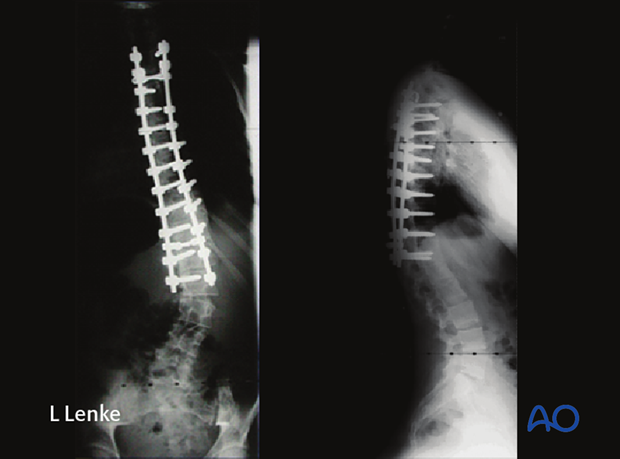
She underwent a PSF from T3-L3 with segmental bilateral pedicle screw fixation and Posterior Column Osteotomies (PCO's) for correction of her curves to 22° and 11° respectively. At two years postoperative she is now skeletally mature without any signs of crankshaft phenomenon.
Clinical rib hump deformity
The rib hump deformity deserves increased attention in the immature patient. Consideration for optimal rib hump correction should be made during surgical correction and this may include performing a thoracoplasty (costoplasty) in select cases of severe rib hump deformities.
2. Abnormal neuroaxis
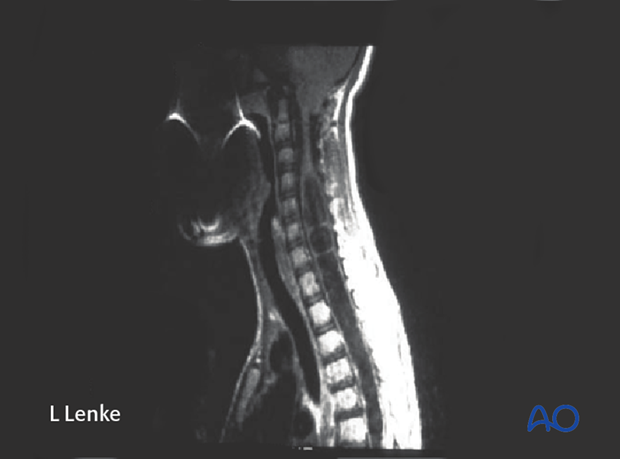
Most patients with AIS will have a normal neuroaxis as seen on a total spine MRI. However patients with atypical curve patterns, abnormal neurological exams or unusual history associated with their scoliosis may have underlying abnormal neuroaxis. Thus, patients with any type of these abnormal preoperative conditions deserve to have a preoperative MRI total spine screening exam. If a neuroaxis abnormality is detected on the MRI scan, consultation with a paediatric neurosurgeon should be considered.
Abnormal AIS curve patterns include most commonly a left thoracic curve or thoracic hyper kyphosis. Both of these are notoriously associated with a high risk of underlying syringomyelia and potential associated Arnold-Chiari malformation.
Patients with AIS should have a completely normal upper and lower motor, sensory, and reflex examination preoperatively. Any abnormalities to the neurological exam warrants a preoperative screening total spine MRI.
Patients with AIS should otherwise have a normal history, free of any spinal pain or rapid progression of curvature. Patients with pain out of proportions to their deformity and/or pain which awakens them at night, or prevents them from pursuing normal activities is atypical and warrants preoperative MRI.
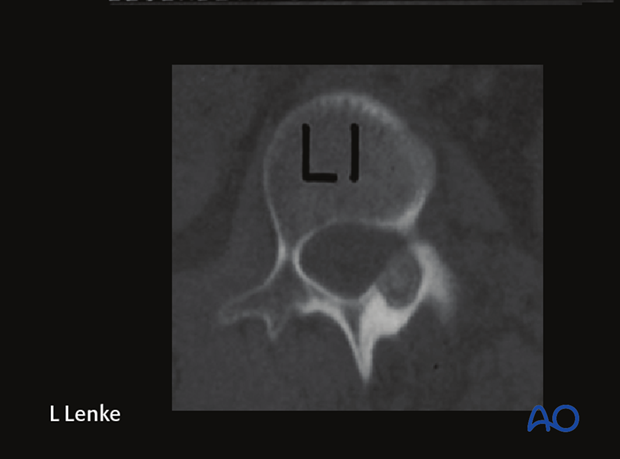
This 13 year, 6 months old female presented with a right thoracolumbar scoliosis along with pain that often awakened her at night. CT-scan imaging of her spine demonstrated a benign osteoid osteoma tumor located in the lamina of her L1 vertebra at the apex of her scoliosis. Thus, her scoliosis was not idiopathic but caused by this benign bone tumor.
3. Body habitus
Patients with AIS come in all shapes and sizes. Overall, the thinner the patient the more clinical deformity they will demonstrate on physical exam. This usually leads to earlier detection of the scoliosis deformity than in those patients with a larger body habitus. In addition, the clinical manifestations of more severe AIS curves are noted to a much greater extent in those patients with a thinner body habitus. Thus, these patients may desire operative correction at a smaller degree of curvature than those patients with a larger body habitus which hides the clinical deformity to a significant degree.
These two nearly identical Lenke 5CN thoracolumbar curves presented for operative correction. The thinner right patient with the 53° curve demonstrates more significant truncal deformation than the left patient with a 52° curve and a larger body habitus.

These two nearly identical Lenke 5CN thoracolumbar curves presented for operative correction. The thinner patient with the 53° curve demonstrates more significant truncal deformation than the patient with a 52° curve and a larger body habitus.













