Posterior approach to the scapular body
1. Introduction
This approach can be used in periprosthetic fractures where the glenoid component remains stable, and there is a displaced scapular body fracture.
Exposure of the body and articular segment of the scapula is based on the extensile Judet approach.
The modified Judet approach avoids detachment of the deltoid muscle and gains almost the same exposure.
This approach permits exposure of the following:
- Lateral column (or margin)
- Articular segment
- Medial border and body

If exposure of the lateral column and articular segment without exposure of the medial border and body is indicated, a direct lateral column (Brodsky) approach can be performed.
Both exposures are based on an interneural, intervascular concept.
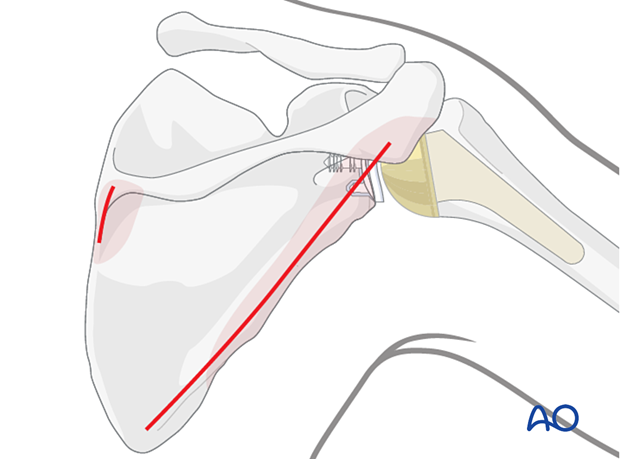
The Brodsky approach may be combined with a limited incision over the medial end of the scapular spine to control a medial border exit fracture line.
Little, if any, muscular detachment is needed for extensile exposure of relevant regions.
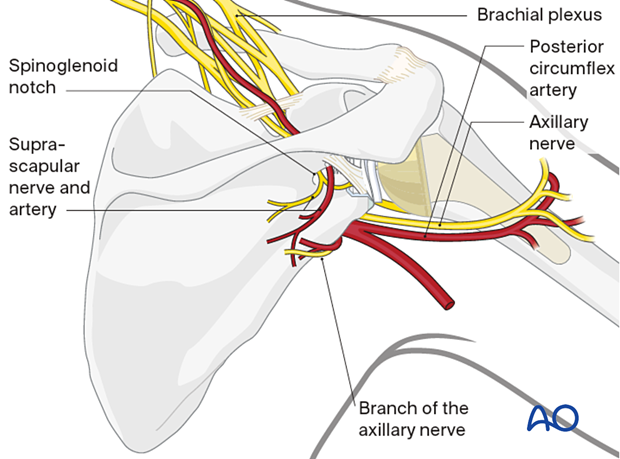
2. Anatomy
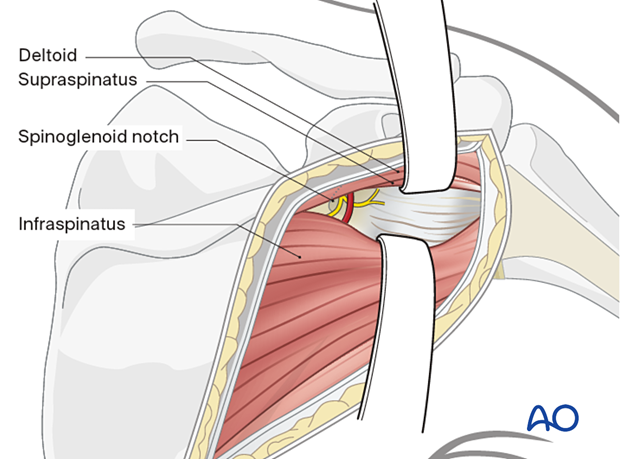
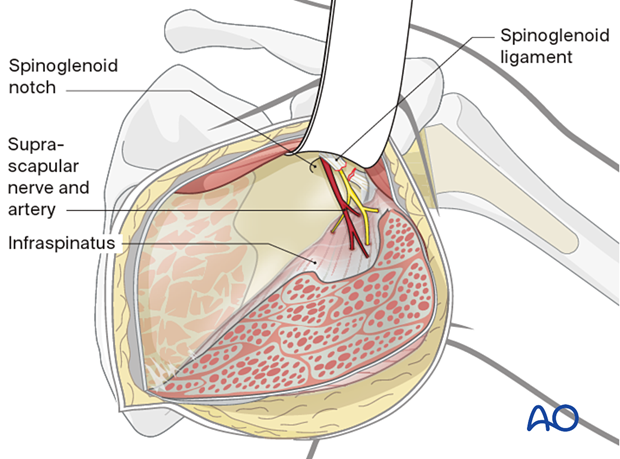
During the posterior approach, care must be taken not to injure the suprascapular nerve at the spinoglenoid notch on its way to supply the infraspinatus muscle.
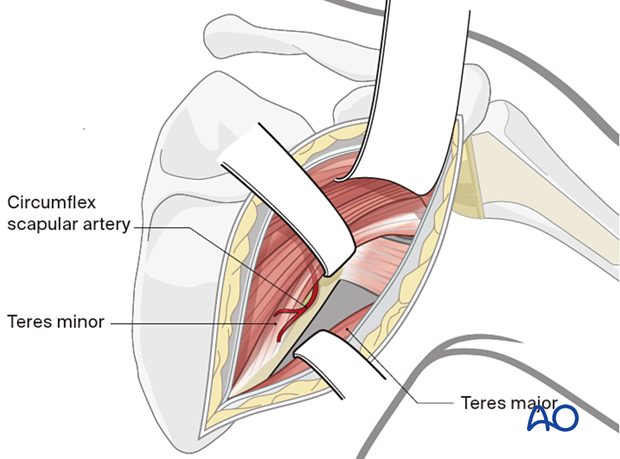
The teres minor is supplied by a posterior branch of the axillary nerve given off as the nerve emerges from the quadrilateral space with the posterior circumflex artery and vein.
3. Positioning
The lateral decubitus position is preferred to allow mobility of the scapula.
Support the injured limb on an arm support with the arm abducted between 45° and 90° relative to the scapula.
4. Marking of anatomical landmarks
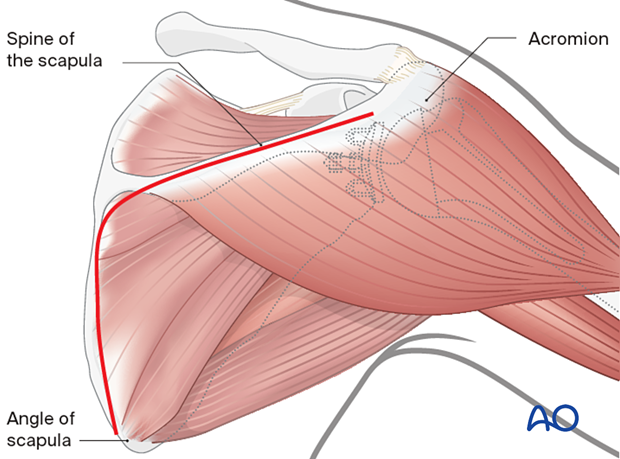
The following anatomical landmarks should be identified and marked:
- The posterior corner of the acromion
- The posterior aspect of the acromioclavicular joint
- The medial end of the scapular spine
- The inferior pole of the scapula
5. Skin incision
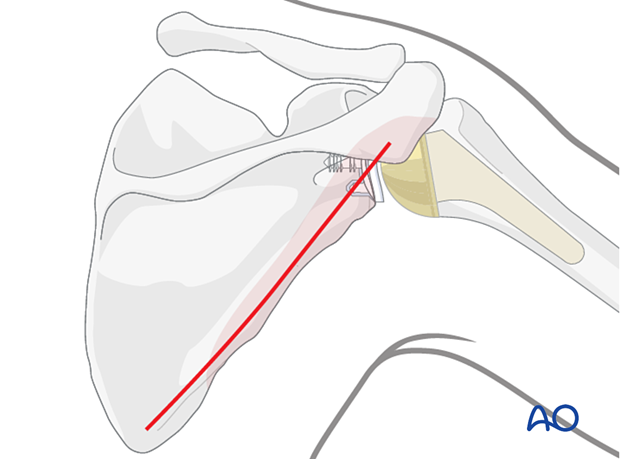
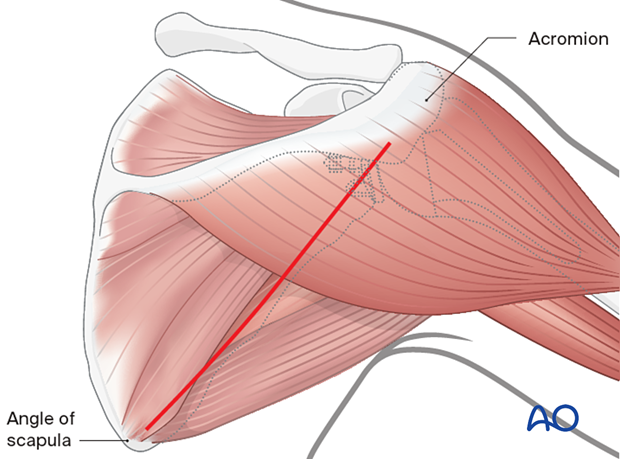
Lateral column approach (Brodsky approach to the scapula)
The incision begins medial to the posterior corner of the acromion and continues distally to the inferior pole of the scapula, parallel to the lateral border of the scapula.
The skin is elevated at the epifascial level just enough to expose the inferior border of the deltoid muscle.
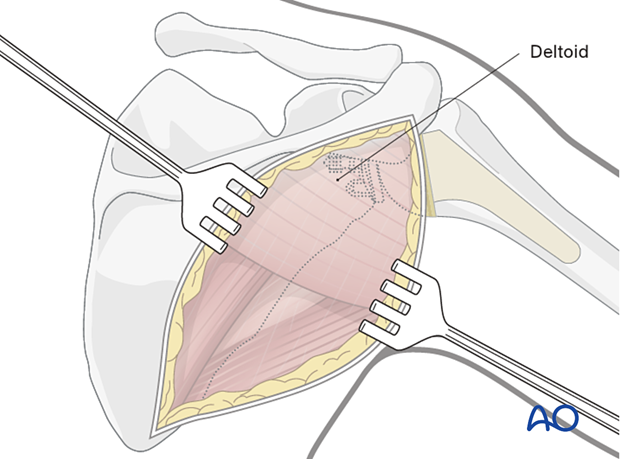
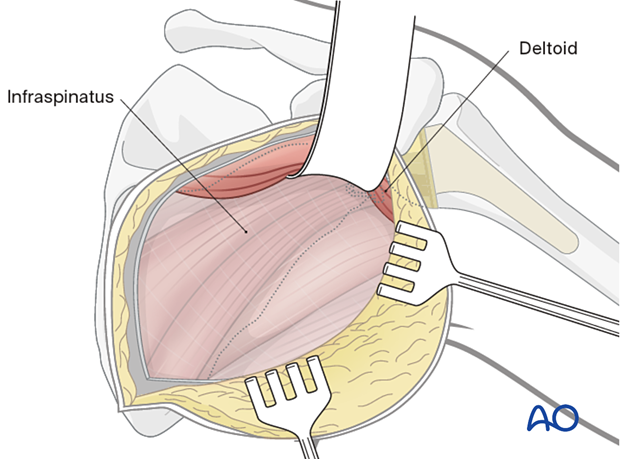
The deltoid muscle is retracted superiorly after incising the fascia over the inferior border of the muscle, taking care to avoid traction on the axillary nerve and posterior circumflex humeral artery laterally. This retraction exposes the infraspinatus fascia, which is incised in the line of the muscular fibers.
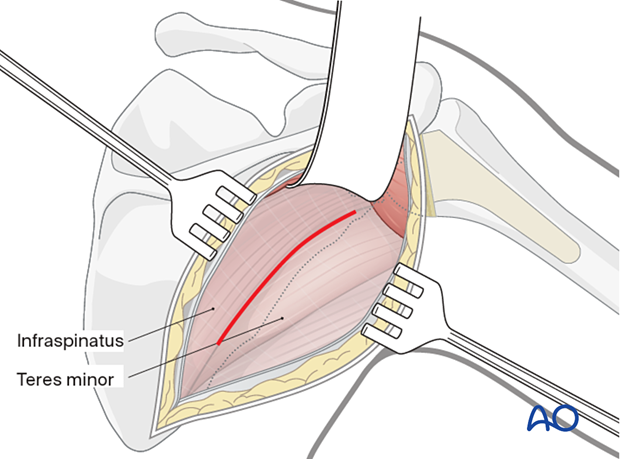
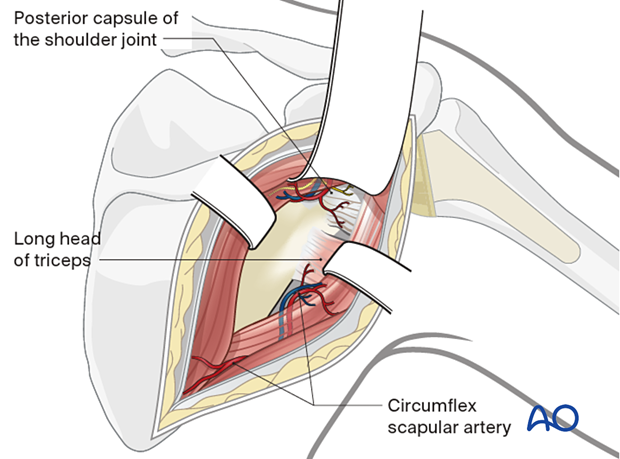
The interval between the infraspinatus and the teres minor is identified. The interval is developed to expose the long head of the triceps laterally. By following this muscle upwards to its attachment to the infraglenoid tubercle, the inferior and posterior capsule of the joint and the inferolateral border of the scapula are exposed.
Exposure of the superior part of the articular segment and glenoid rim can be performed through the interval between the supraspinatus and infraspinatus. Care must be taken to avoid injury of the nerves to the infraspinatus at the spinoglenoid notch.
The interval between the teres minor and teres major is identified by exposure of the circumflex scapular vessels. This interval permits exposure of the remainder of the lateral column.
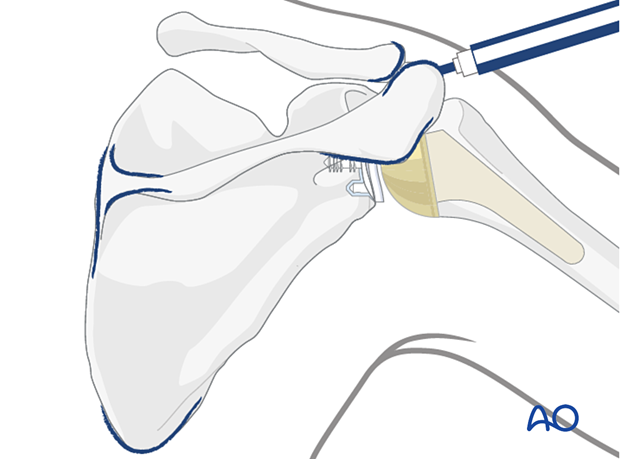
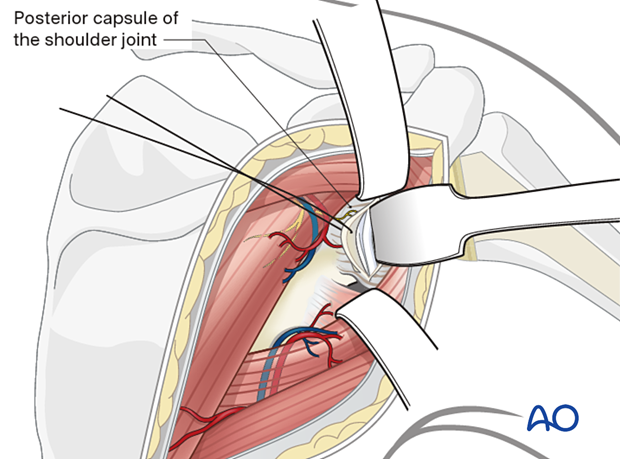
A transverse posterior glenohumeral arthrotomy exposes the glenoid fossa when checking for intra-articular fracture reduction and inadvertent penetration of the joint surfaces by fixation screws.
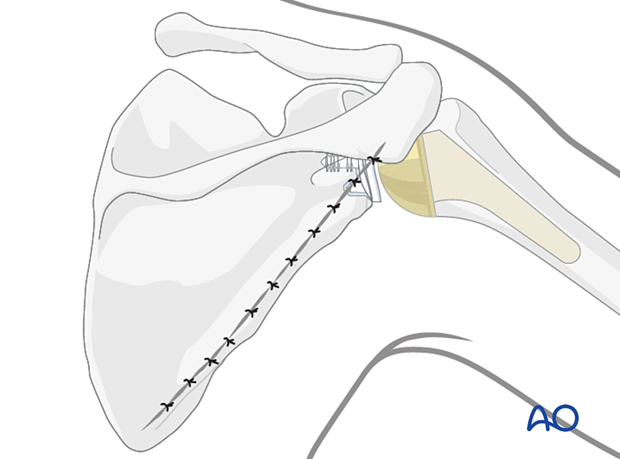
Modified Judet incision
Begin the incision at the posterior corner of the acromion. Continue the incision along the spine of the scapula to its medial border and then distally to the inferior pole of the scapula.
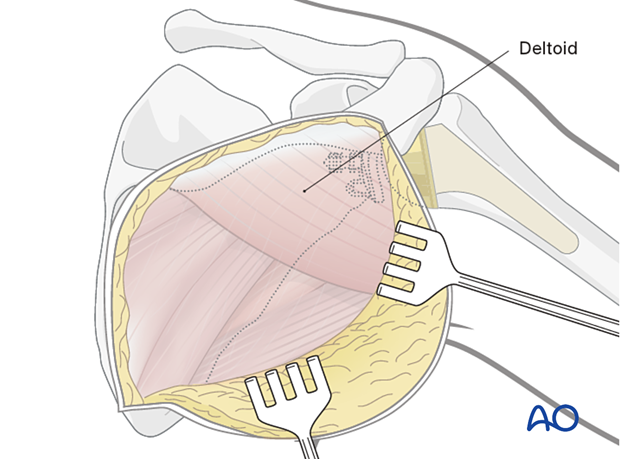
In this approach elevate the posterior border of the deltoid without detachment from the spinal scapula to expose the infraspinatus.
The deltoid muscle may or may not be detached from the spine of the scapula for greater access to the superior part of the articular segment depending on the fracture pattern.
The infraspinatus muscle is elevated from the infraspinous fossa and retracted laterally to expose the entire posterior aspect of the scapula.
This includes:
- The posterior aspect of the neck of the scapula
- The posterior glenoid rim
- The posterior scapular body
6. Wound closure
After definitive fixation, the wound is irrigated, and the joint capsule is repaired. The fascia over the infraspinatus muscle is repaired. The deltoid muscle is allowed to fall back into place. It is not necessary to repair the deltoid fascia.
The subcutaneous fascia and the skin are closed in layers.