Posteromedial approach to the proximal tibia
1. Principles
A skin incision posterior and medial to prior midline arthroplasty incisions can be safely achieved.
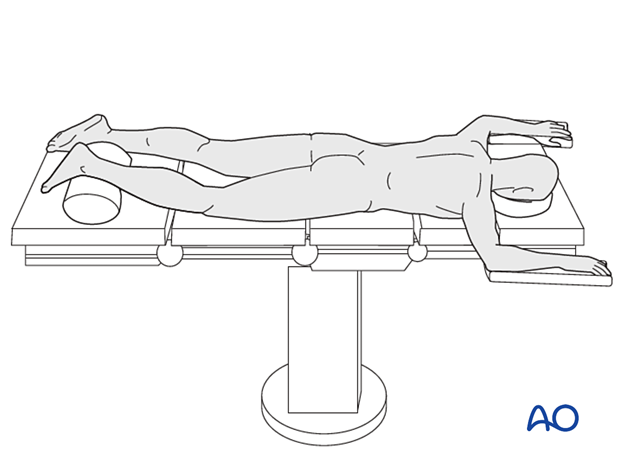
2. Patient position
The patient is positioned prone with the hip fully extended and the knee flexed approximately 15°. A tourniquet may be used. Application before positioning and draping may facilitate sufficient access for the incision.
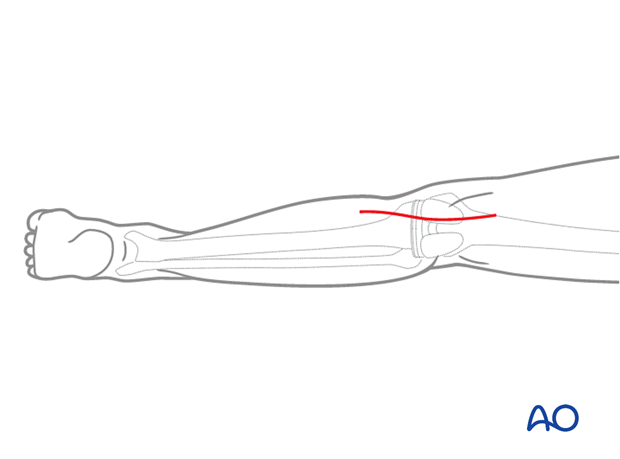
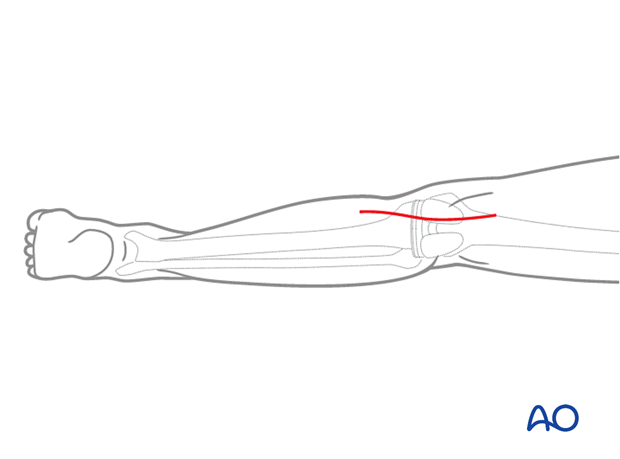
3. Skin incision
A 10-15 cm long skin incision is made along the posterior border of the hamstring tendon extending distally along with the medial gastrocnemius and soleus musculature.
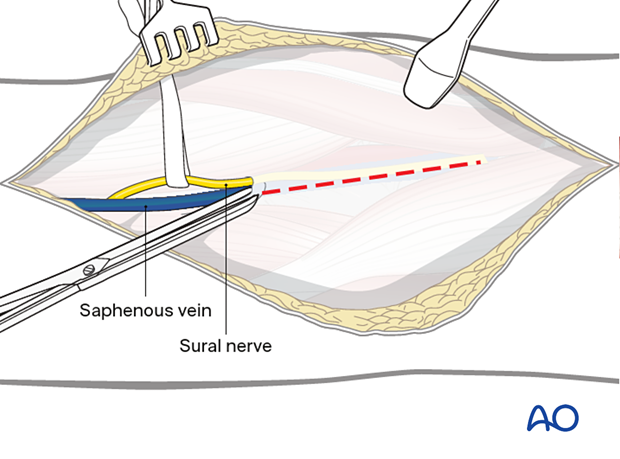
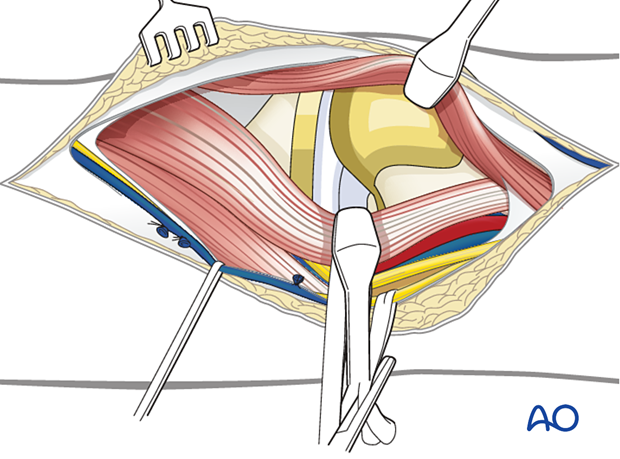
4. Fascial incision
Open the crural fascia. Identify and save the short saphenous vein and the medial sural cutaneous nerve.
The fascial incision is made in line with the skin incision. It is critical to remain on the medial aspect of the gastrocnemius to avoid injury to the popliteal neurovascular bundle.
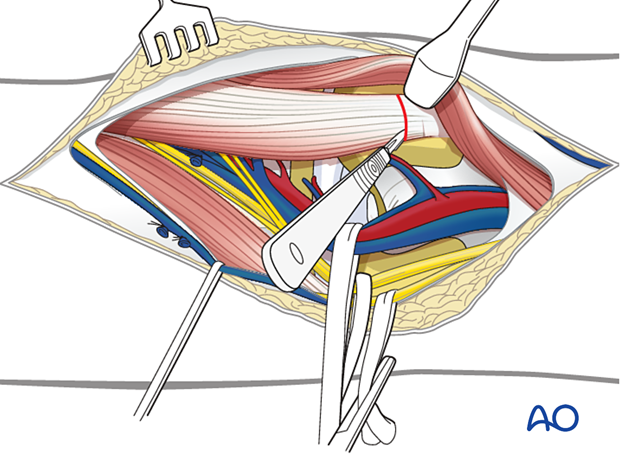
5. Deep dissection
The pes anserine tendons are reflected anteromedially allowing for dissection directly down to the posteromedial border of the bone.
A periosteal elevator can then be used to elevate the gastrocnemius and underline popliteus muscle, and a blunt retractor can be placed around the lateral tibia. Care must be taken to carefully reflect the popliteal artery and vein proximal to the trifurcation of the vessels.
Alternatively, the medial gastrocnemius tendon can be released from the medial femoral condyle, allowing for greater exposure. This does however place the neurovascular bundle at greater risk.
6. Closure
The medial gastrocnemius can be repaired primarily utilizing a non-resorbable stitch or a suture anchor. The fascia can be closed using a running absorbable stitch and the skin can be closed according to the surgeon's preference.













