Complications and technical failures
1. Introduction
Tibial shaft fractures are associated with significant but predictable complications.
Treatment related complications can be minimized by anticipating them and paying attention to the general principles of fracture management.
There is limited potential for remodeling and anatomical reduction of fractures should be achieved, particularly in the adolescent patient.
2. Compartment syndrome
Compartment syndrome is most common in the lower leg.
The diagnosis of compartment syndrome should be suspected in a conscious and alert patient, when the following early signs are present:
- Pain, unrelated to the posture of the limb, made worse by passive movement of muscles in the relevant compartment
- Paresthesia
- Progressive loss of light touch sensation
3. Infection
The risk of infection is increased in:
- Open fractures and associated soft-tissue injuries
- Soft-tissue tethering around K-wires, pins, or prominent implants
- Delayed removal of exposed K-wires
4. Cast complications
Pediatric fractures are commonly treated with a cast but this requires close attention to detail.
Preventive measures during application:
- Padding all pressure points (eg, malleoli, patella, fibular head)
- Correct application of cast bandage
- Avoid application of a complete cast in a swollen leg
- Exposure of all toes to allow assessment of distal circulation
Preventive measures after cast application:
- Elevation of the leg
- Instructions to care givers:
- Check toe perfusion
- Check for excessive swelling
- Avoid insertion of objects between cast and skin
- Avoid wetting the cast and padding
Preventive measures during cast removal:
- Using sharp saw blades to avoid injury
5. Delayed union and nonunion
Tibial shaft fractures are associated with significant but predictable complications.
Nonunion is rare in pediatric tibial shaft fractures and requires investigation for a pathological cause.
Delayed union may occur as a consequence of:
- Instability
- Persistent fracture gap
- Open reduction
- Inappropriate choice or use of implant
- Severe soft-tissue damage
- Infection
- Devascularization
- Delayed weight bearing
- Bone loss
- Vitamin D deficiency

6. Refracture
Causes:
- Early implant removal
- Malunion
- Premature return to sport
7. Malunion
Causes:
- Intact fibula
- Inadequate reduction
- Inappropriate choice or use of implant
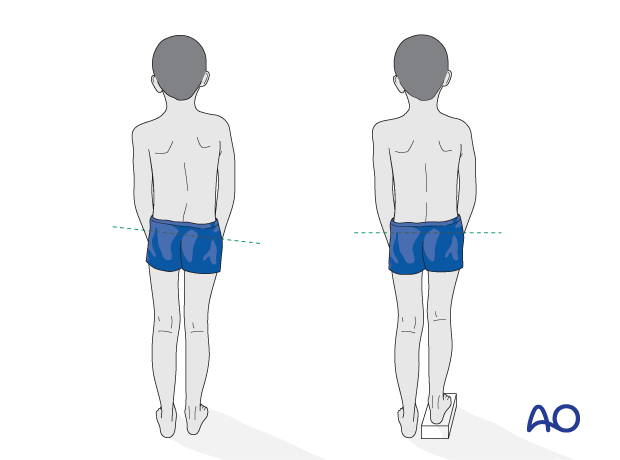
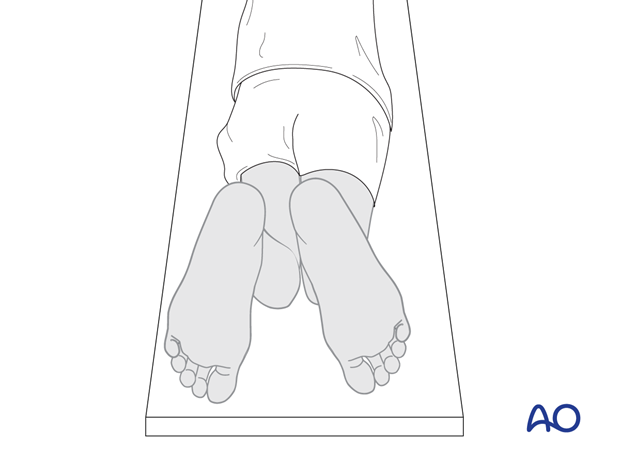
In this illustration, malunion of the tibial shaft can be seen with external rotation of the right foot.
Cases
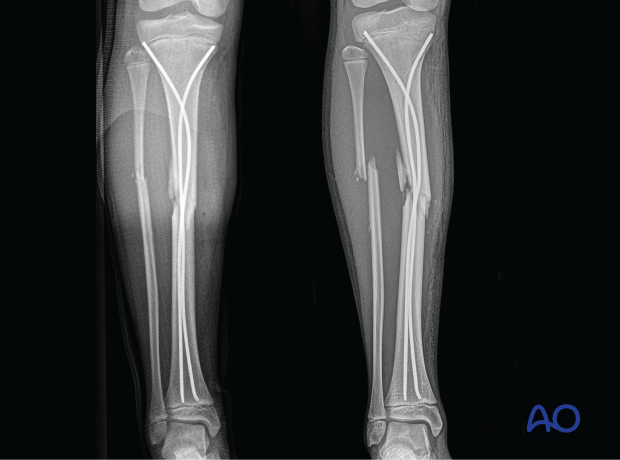
These x-rays show a both-bone fracture in an adolescent treated with elastic nailing.
Technical errors include:
- Incorrect nail diameter
- Inadequate contact between nail and cortex in an unstable fracture pattern
- Corkscrew phenomenon
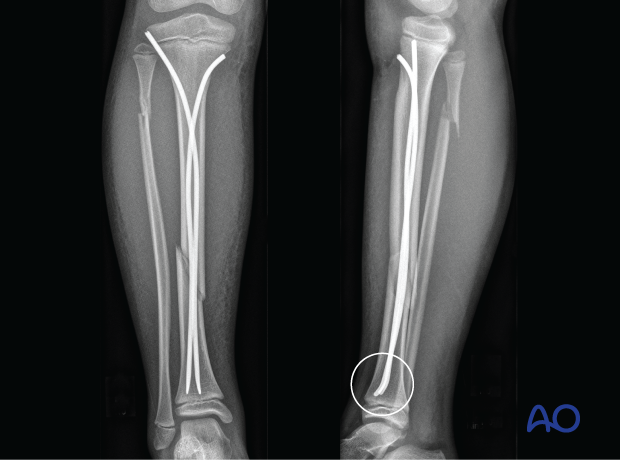
These x-rays show an oblique tibial shaft fracture treated with elastic nailing.
A loss of physiological apex anterior alignment of the tibia because of incorrect nail orientation can be seen.
The nail tips should be directed dorsally.
8. Implant pain/prominence
Causes:
- Large plates with inadequate soft-tissue cover
- Long screws
- Prominent nail ends
9. Joint stiffness
Causes:
- Prolonged immobilization due to:
- Pain
- Instability - Extensive soft-tissue injury
10. Peri-implant fracture
Causes:
- Stress riser from plate or short nail
- Pathological bone (eg, disuse osteopenia, osteogenesis imperfecta)
11. Growth stimulation
Growth stimulation may occur and continue until after fracture healing and until remodeling is complete.
This may lead to leg-length discrepancy.
Leg lengths should be evaluated at intervals up to 2 years after injury.