Nonoperative treatment - Splinting
1. General considerations
Indications
Most tibial shaft fractures require initial management with a long leg cast.
A short leg splint (or below-knee cast or brace) may provide sufficient support for stable diaphyseal tibial, eg, toddler’s fracture, and fibular injuries.
Tibial fractures managed with a splint require close radiological follow-up.
A splint can also be used following surgical fixation in the early postoperative period.
Complications
- Pressure sores
- Skin irritation
- Compartment syndrome
- Thermal burns (avoid using hot water)
2. Preparation
Read the additional material on preoperative preparation.
Material
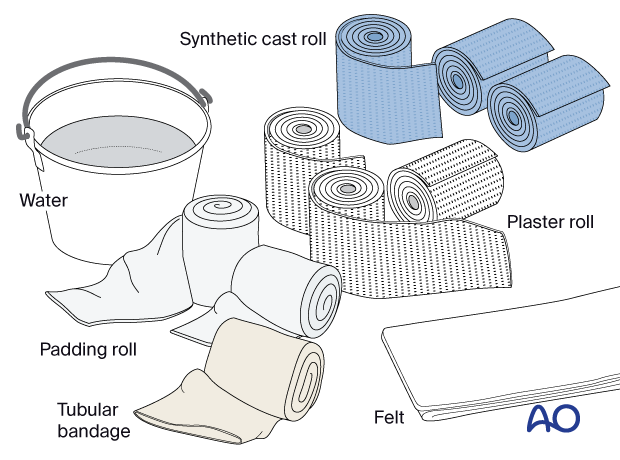
- Tubular bandage (stockinette) of appropriate size
- Cast padding
- Felt
- Casting material: synthetic, plaster of Paris, or a combination of both
- Water
The water temperature should ideally be between 22° and 25° C.
3. Splinting
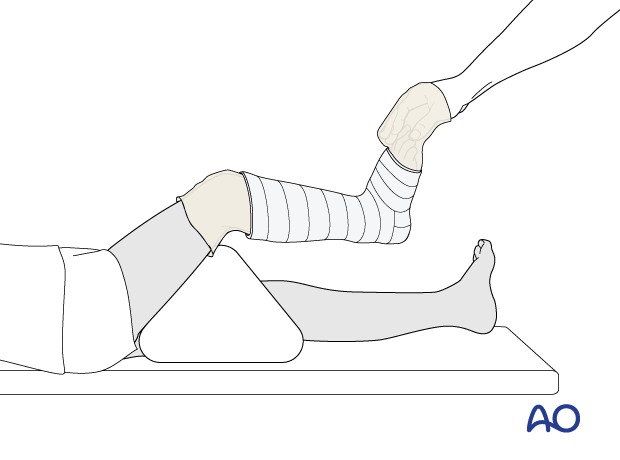
Patient and leg positioning
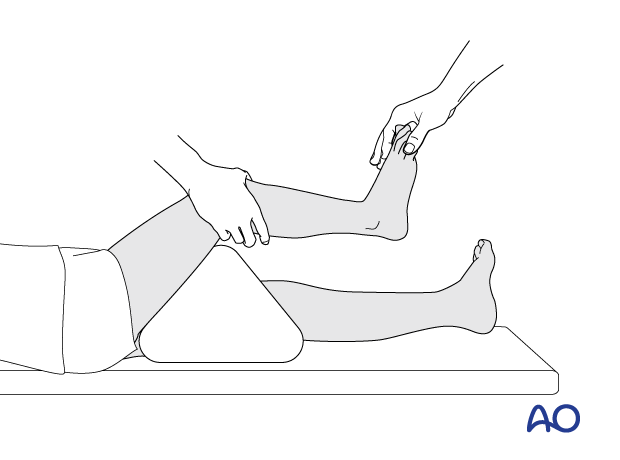
Place the patient in a supine position with a bolster under the knee to keep it flexed.
An assistant also supports the leg to maintain knee flexion.
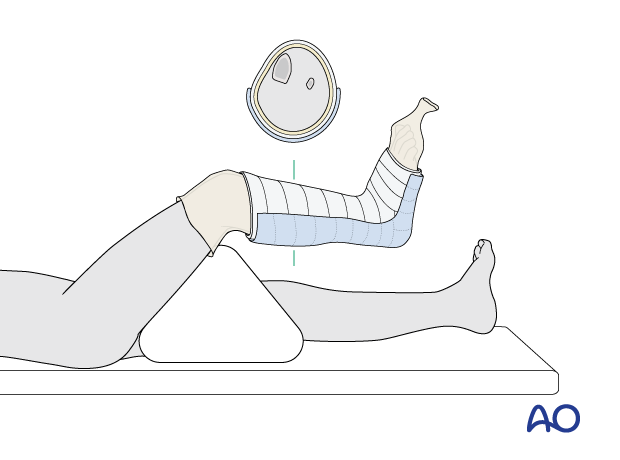
Dressing
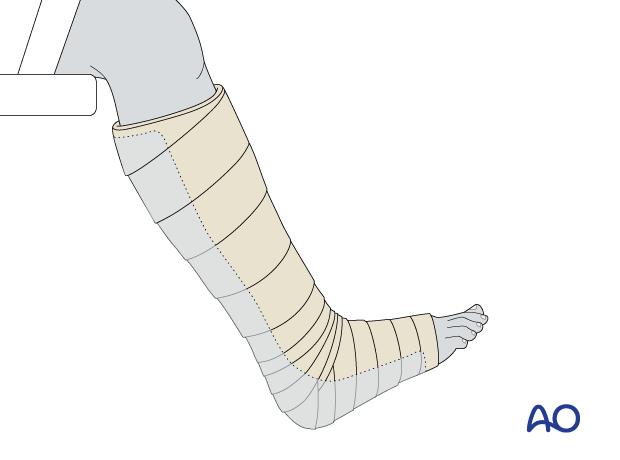
The cast extends from just below the knee to the base of the toes.
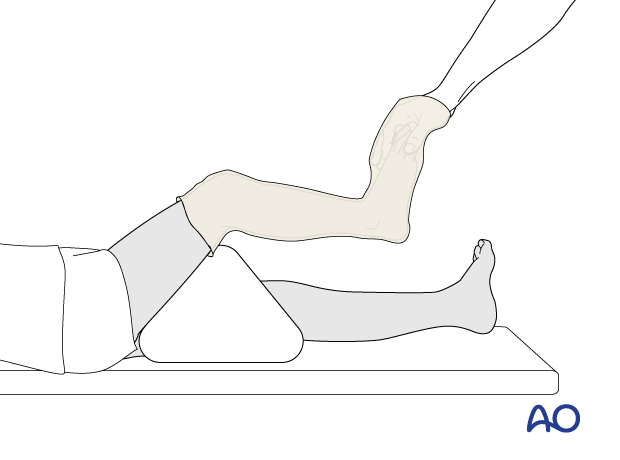
Apply a tubular bandage and cut it slightly longer than the length of the final cast.
The assistant holds the toes, not the stockinette, with the ankle in a neutral position.
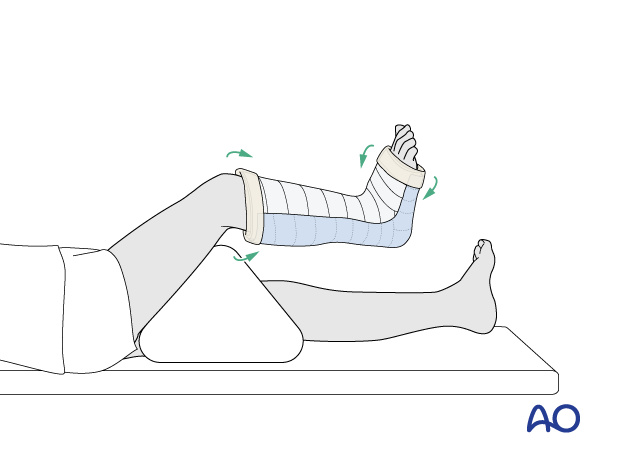
Padding
Add thick felt or additional padding at the free edges of the cast and prominent areas (eg, tibial crest, malleoli, and heel) to prevent pressure sores.
Apply cast padding without creases, overlapping each layer by 50%.
It should be appreciated that, when more padding is applied, there will be less support at the injury site.
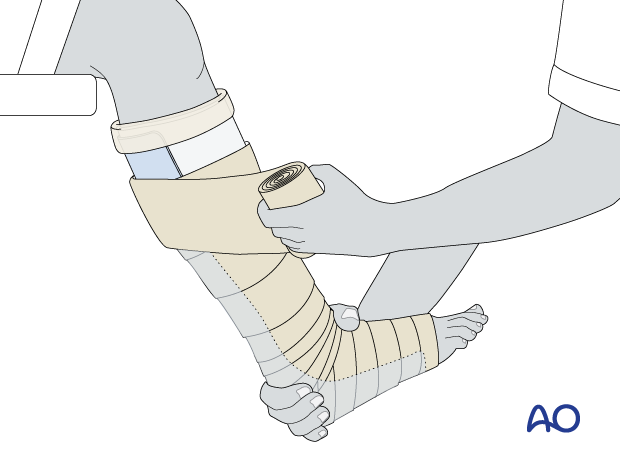
Application of the back slab
The assistant holds the ankle.
Apply a slab of 3–6 layers of cast material.
Avoid sharp edges at the ends of the cast.
Fold the tubular bandage and padding over the edges.
Apply an elastic bandage to hold the splint in place.
Ensure that all toes are visible for vascular assessment.
4. Final assessment
After cast application, check the fracture configuration with x-rays in both planes.
Confirm normal toe color and capillary refill at the end of cast application.
5. Aftercare
Instructions to parents/carers
Parents/carers should understand the following precautions and instructions:
- Check daily for swelling, discoloration, and impaired toe circulation (any of which should be reported urgently)
- Immediately report signs suggesting skin irritation ulceration, and cast soiling
- Make sure the cast padding remains dry and avoid inserting anything between the cast and skin
Immediate postinjury care
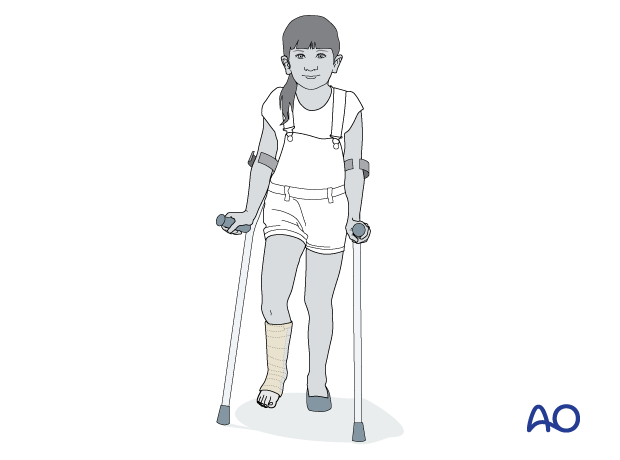
Weight-bearing is encouraged when comfort allows.
Pain control
Routine pain medication is prescribed for 3–5 days after injury if required.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Follow-up
The first clinical and radiological follow-up is usually undertaken 1–2 weeks after injury to confirm fracture position.
A radiograph to evaluate bone healing should be taken after about 4 weeks. When clinical and radiological signs indicate that the fracture no longer needs external support, the cast can be removed.
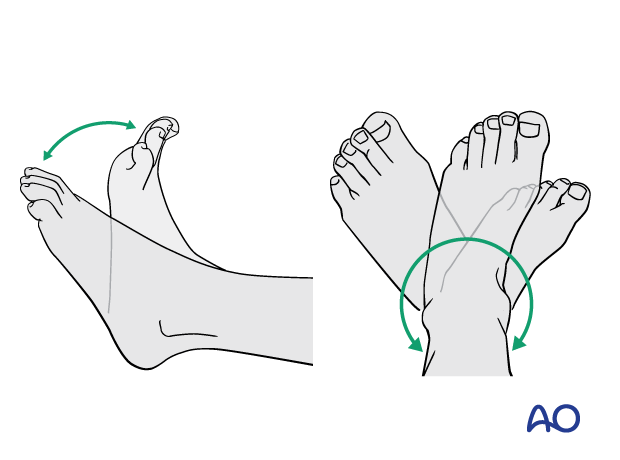
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be necessary in some cases but is not mandatory.
Activities that involve running and jumping are not recommended until full recovery of local symptoms.
Follow-up for growth disturbance
Leg length should be evaluated up to 2 years following injury due to the effect of growth stimulation.













