Suture fixation
1. General considerations
Displaced avulsion fractures of the tibial spine require internal fixation to reconstruct the attachment of the anterior cruciate ligament (ACL).
Tibial spine fragment may be stabilized with suture fixation through bone tunnels.
Reduction may be arthroscopically assisted, provided appropriate equipment and skills are available.
Advantages:
- Direct evaluation of the fragment and reduction
- Possible fixation of comminuted and small fragments
- Anatomical restoration of the ACL tension
- No implant removal necessary
2. Patient preparation
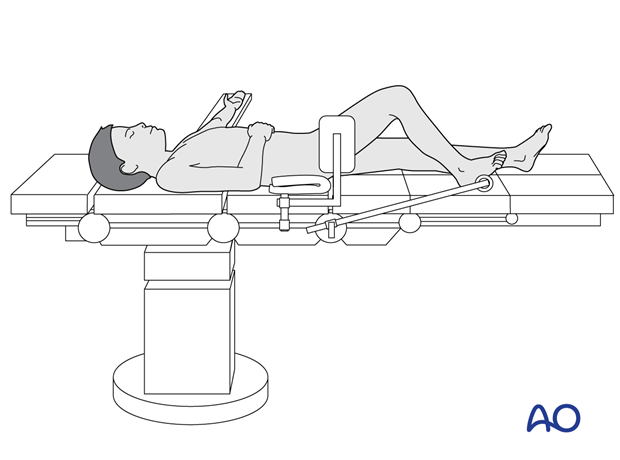
This procedure is normally performed with the patient in a supine position for arthroscopy.
For an arthrotomy, a supine position should be used.
3. Approaches
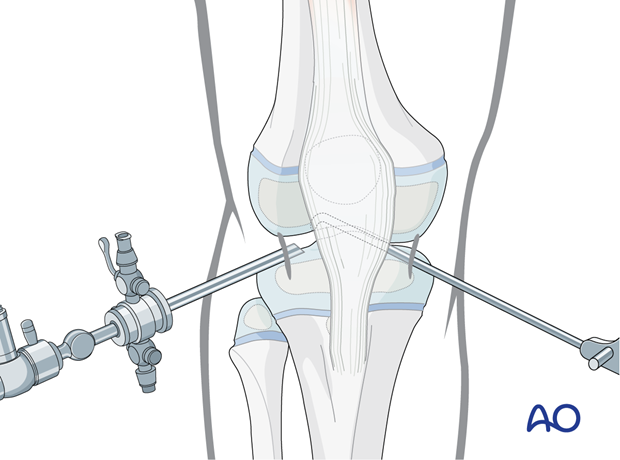
Arthroscopically assisted approach
The anteromedial-anterolateral arthroscopy assisted approach may be used but advanced experience in arthroscopic surgery is essential.
Moving the camera to the lateral entry portal may provide better visualization of the zone of injury.
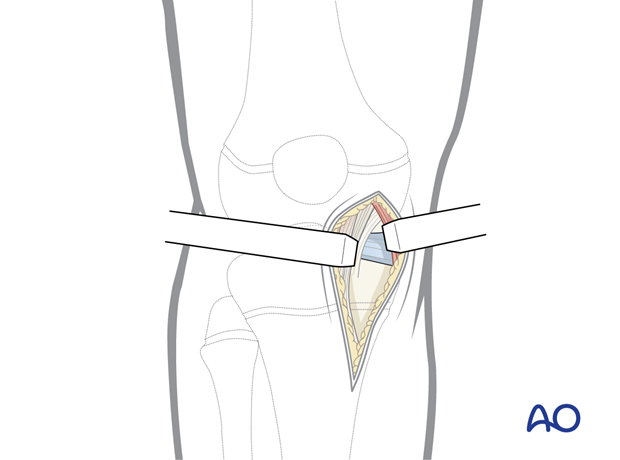
Arthrotomy
A limited medial or lateral arthrotomy can be used. The incision may be enlarged as necessary for direct visualization.
4. Reduction
Reduction with arthroscopy
Initially, reduce the spine fragment with a hook inserted through the working portal.
Definitive reduction will be achieved with the tensioning of the suture band.
Open reduction
Reduce the spine fragment with a hook or ball spike pusher inserted in the arthrotomy.
Confirm the reduction under direct vision or with an image intensifier.
5. Fixation
Drilling holes
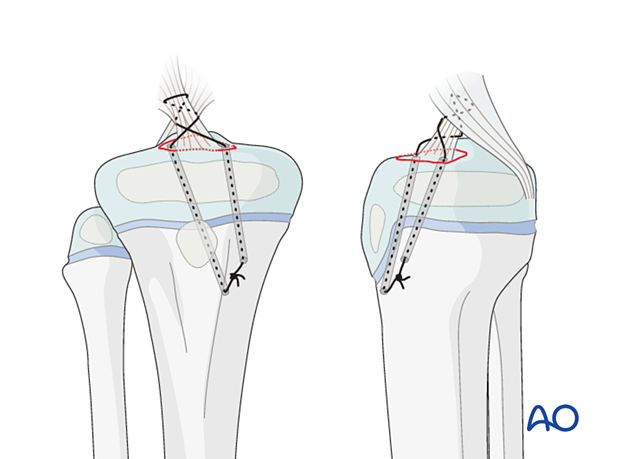
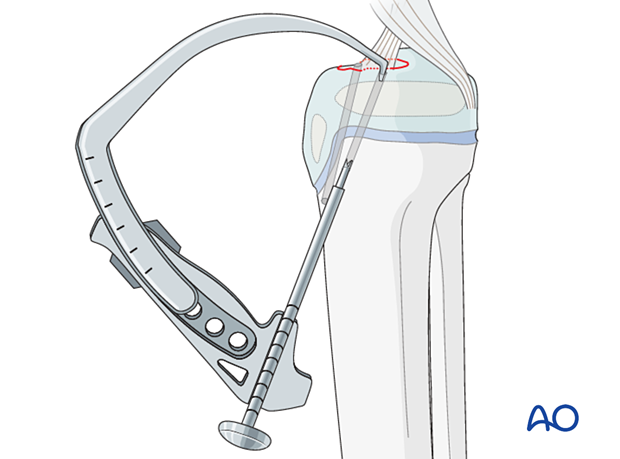
Drill two holes from the proximal medial tibia into the tibial spine fragment using a cannulated drill over a K-wire.
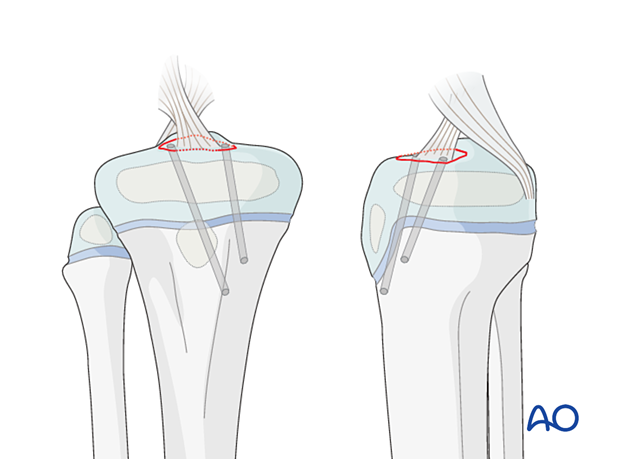
Ideally, the drill holes exit medial and lateral to the base of the ACL.
The use of an ACL drill guide system assists with accurate positioning of the drill holes and fracture reduction.
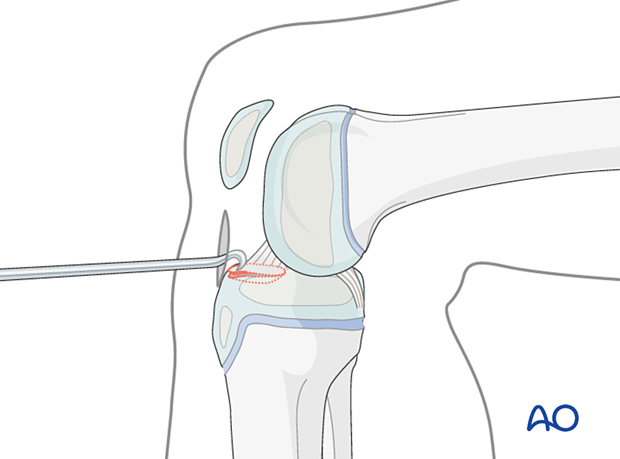
Suture application
Place a fiber wire or PDS (size 0) through one of the drill holes in a retrograde direction.
A suture passer should be used if available.
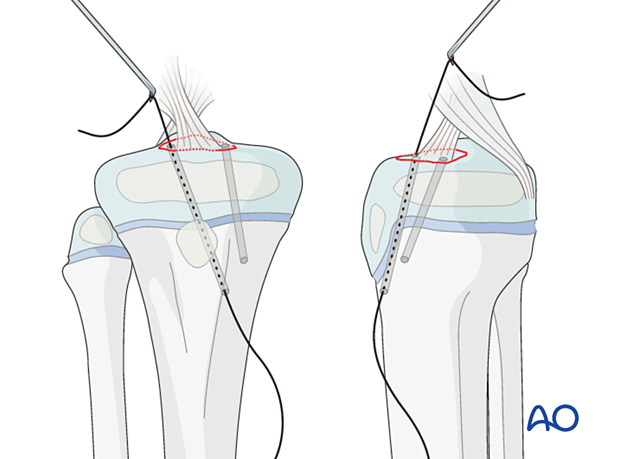
Pass the suture through the ACL several times.
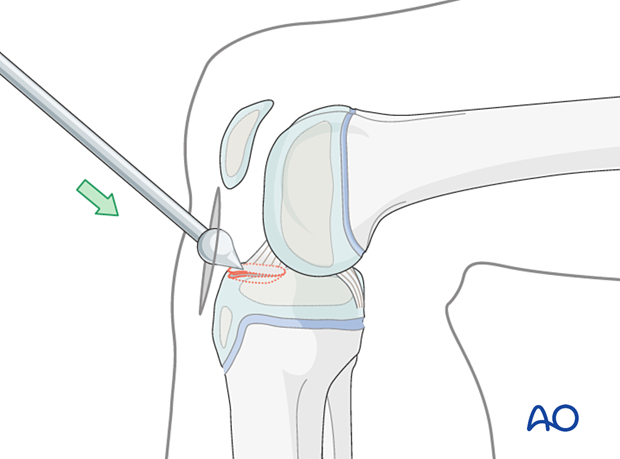
Insert a lasso in a retrograde direction to capture the suture end and pass it through the second hole.
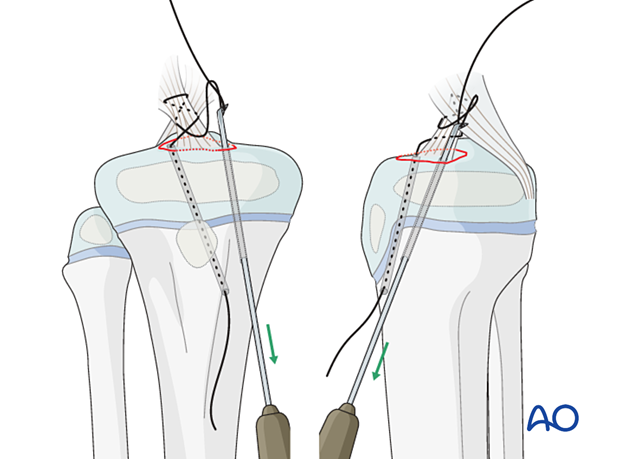
Pull the sutures to tighten the ligament …
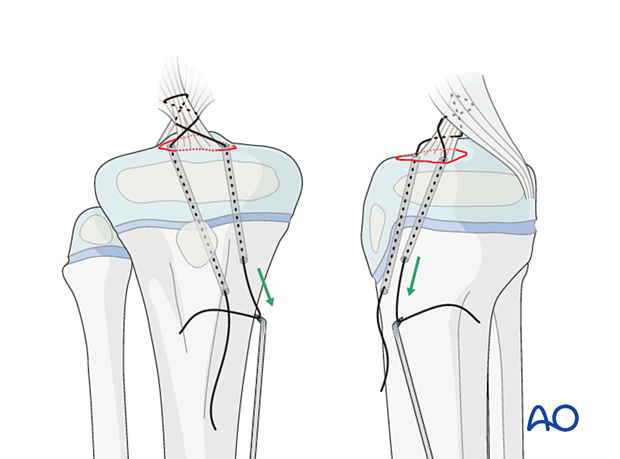
… and tie a knot.
A suture button may be used if the size of the bone bridge between the drill holes is too small.
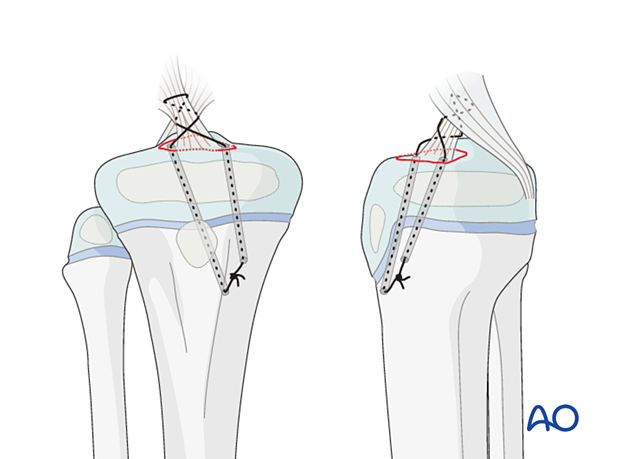
6. Final assessment
Confirm reduction of the fragment and tension of the ACL under arthroscopy/direct vision and with an image intensifier.
7. Immobilization
Depending on the stability of fixation, a cylinder cast with the knee flexed to 20°–30° may be applied for 4–6 weeks.
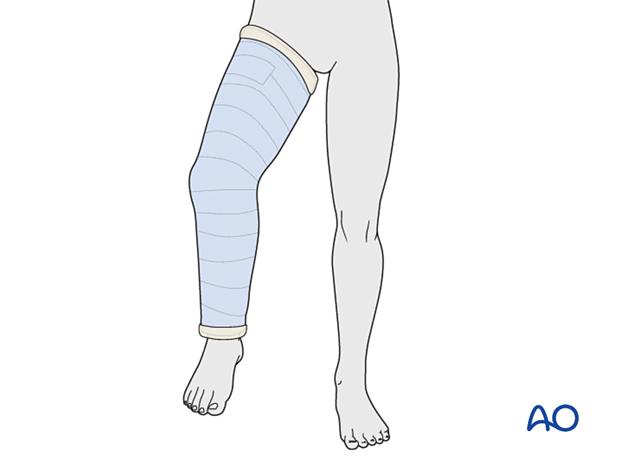
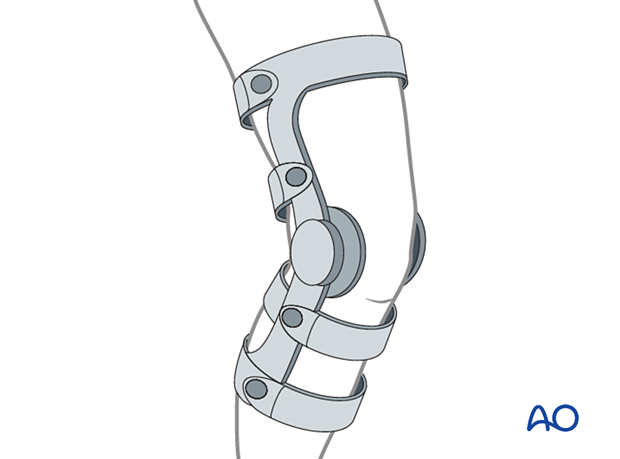
Alternatively, a hinged knee brace may be used with a gradually increasing range of motion over 6 weeks, with the patient instructed to remain touch-weight bearing.
8. Aftercare
Immediate postoperative care
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up
The first clinical and radiological follow-up is usually undertaken at 6 weeks.
Long-term follow up with clinical assessment of ligament stability is mandatory because of possible residual ACL insufficiency.
Growth disturbance is rare as the fracture usually does not involve the physis. Growth arrest of the tibial apophysis may result in recurvation malalignment. This should also be checked in a long-term follow-up (ca 2 years after trauma).
9. Case
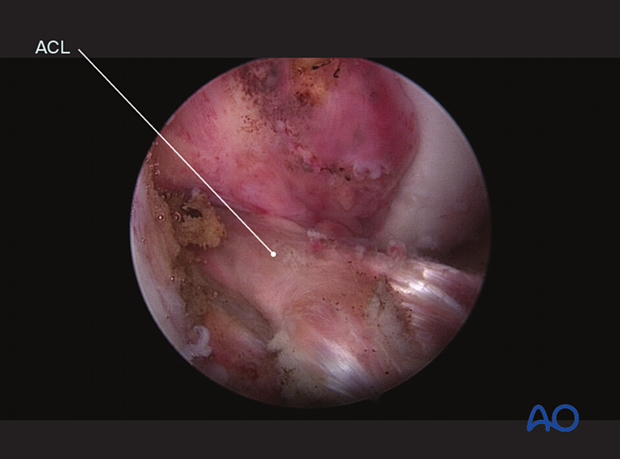
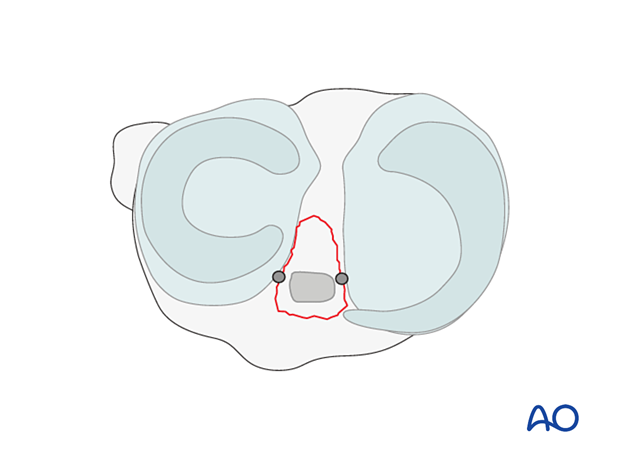
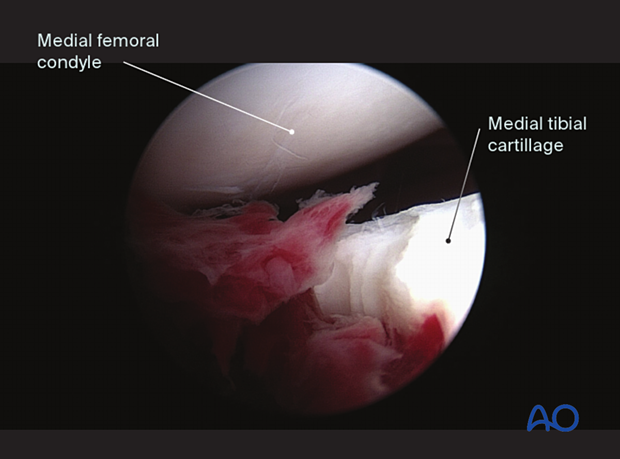
Arthroscopic views of a tibial spine avulsion
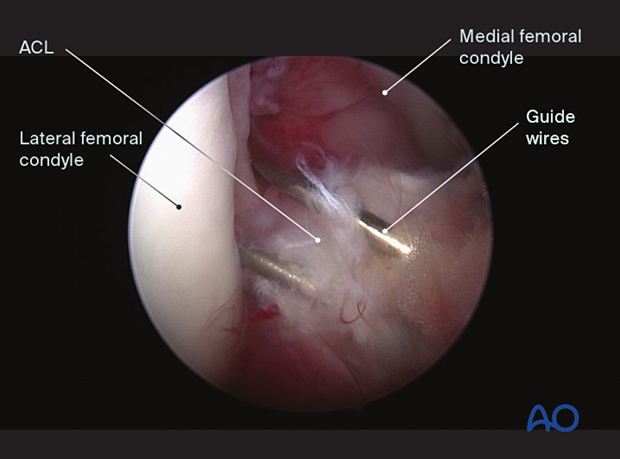
Guide wires for the cannulated drill placed with the ACL drill guide system
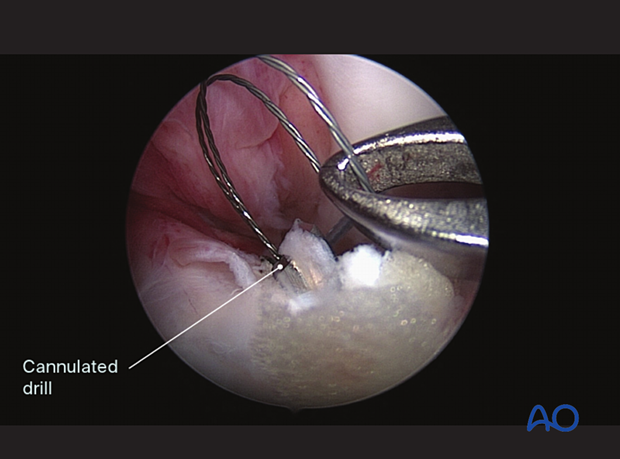
Suture lassos inserted through the cannulated drill into the joint for passing the suture (fiber wire)
Fiber wire inserted through the base of the ACL
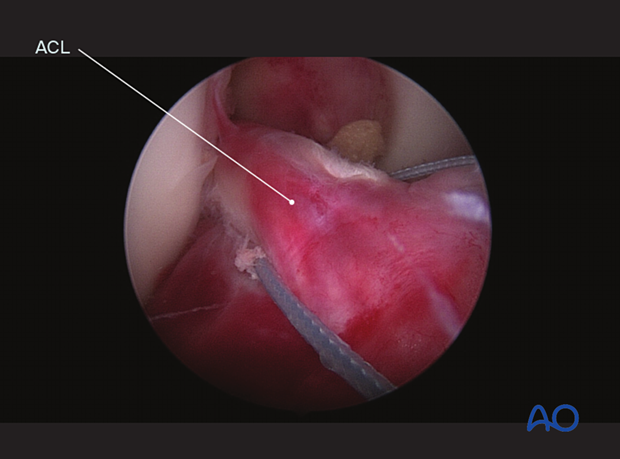
Reduced tibial spine fragment and ACL under tension