Arthroscopically assisted screw fixation
1. General considerations
Introduction
Displaced avulsion fractures of the tibial spine require internal fixation to reconstruct the attachment of the anterior cruciate ligament (ACL).
Reduction may be arthroscopically assisted, provided appropriate equipment and skills are available.
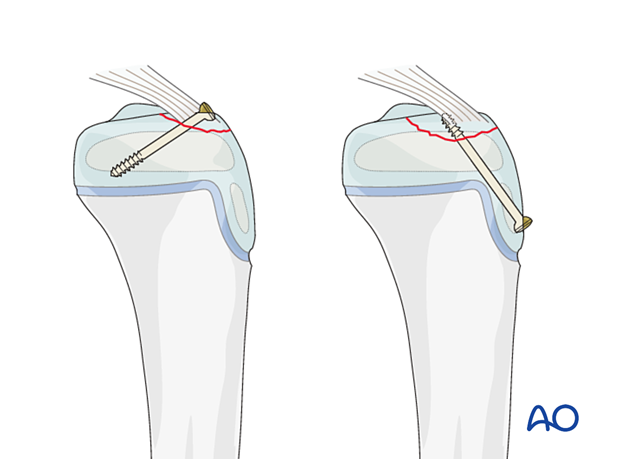
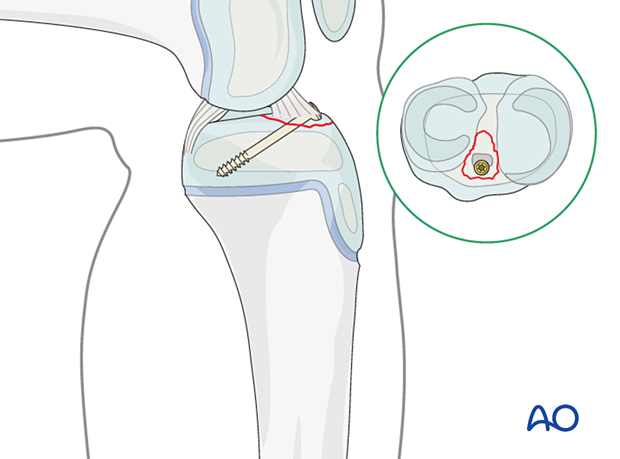
Antegrade screw fixation
A large tibial spine fragment may be stabilized using a screw.
This screw should not cross the physis.
Small or comminuted fragments should be stabilized with a suture.
Crossing the physis should be avoided but this may result in decreased stability.
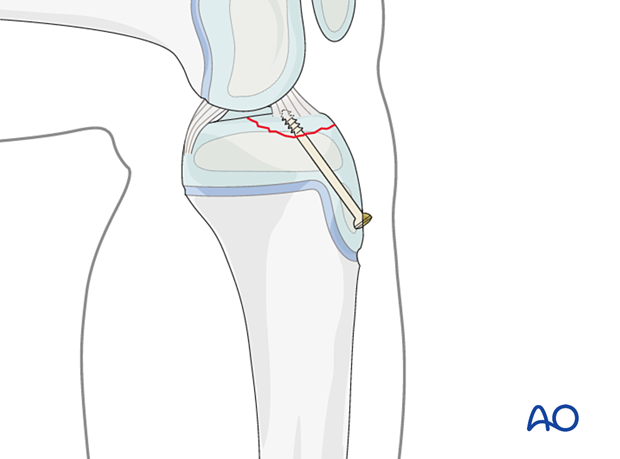
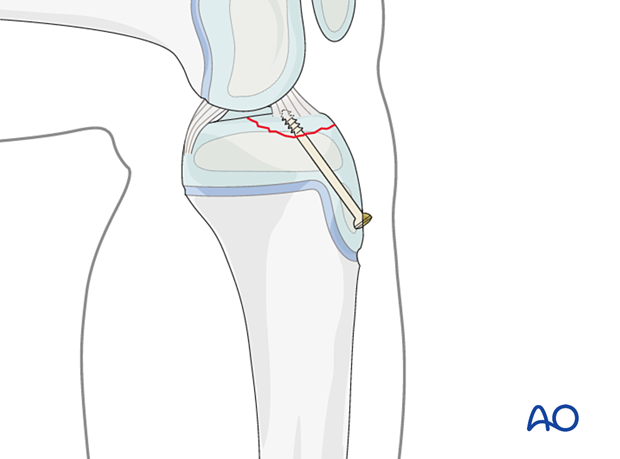
Retrograde screw fixation
The screw(s) may be inserted along the line of action of the ACL and this has the advantage of easier implant removal.
The thread of a retrograde partially cannulated screw may limit compression across the fracture and the correct ACL tension may, therefore, not be restored.
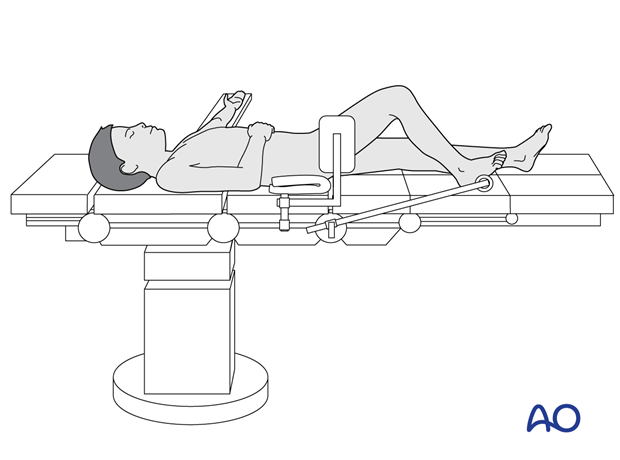
2. Patient preparation
This procedure is usually performed with the patient in a supine position for arthroscopy.
3. Approach
The anteromedial-anterolateral arthroscopy assisted approach may be used but advanced experience in arthroscopic surgery is essential.
Moving the camera to the lateral entry portal may provide better visualization of the zone of injury.
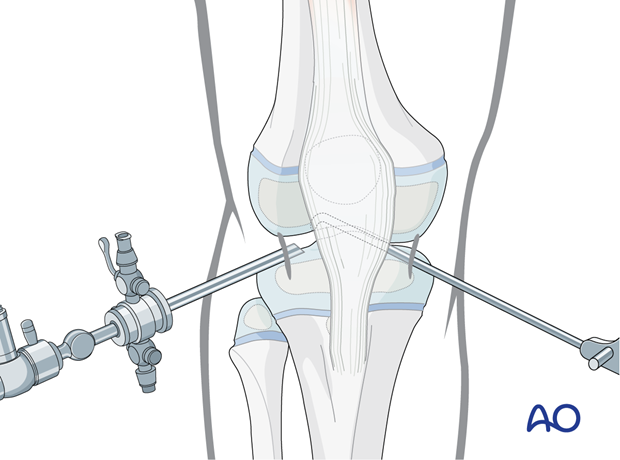
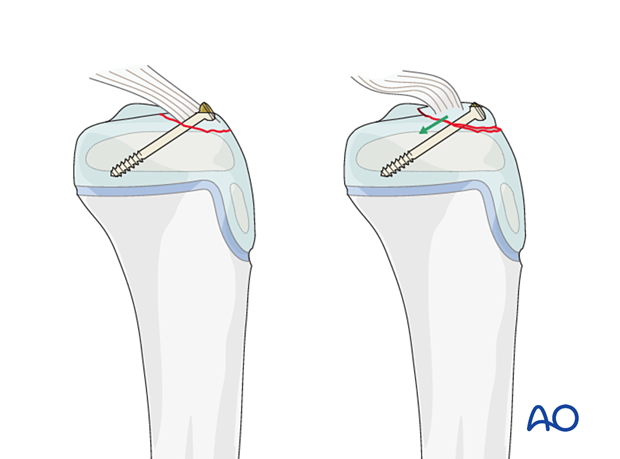
4. Reduction
Reduce the spine fragment with a hook inserted through the working portal.
Confirm the reduction arthroscopically or with an image intensifier.
5. Fixation
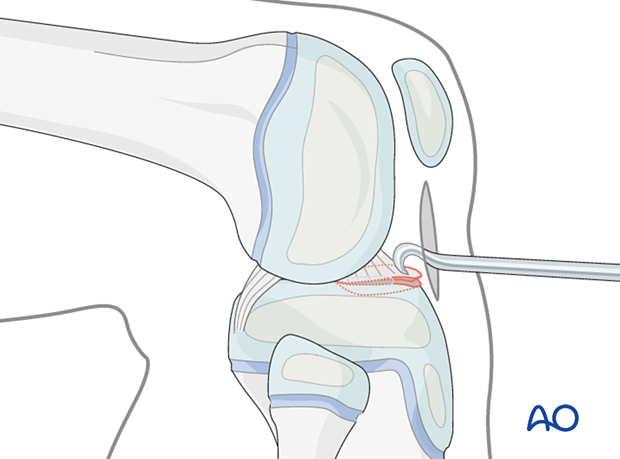
Antegrade lag-screw fixation
Flex the knee to 80°.
Insert a screw ensuring that it does not cross the physis, or compromise the articular cartilage or ligament insertion sites.
Cannulated small fragment screws are the implant of choice.
To avoid dorsal displacement, maintain the fracture reduction with a hook during screw insertion.
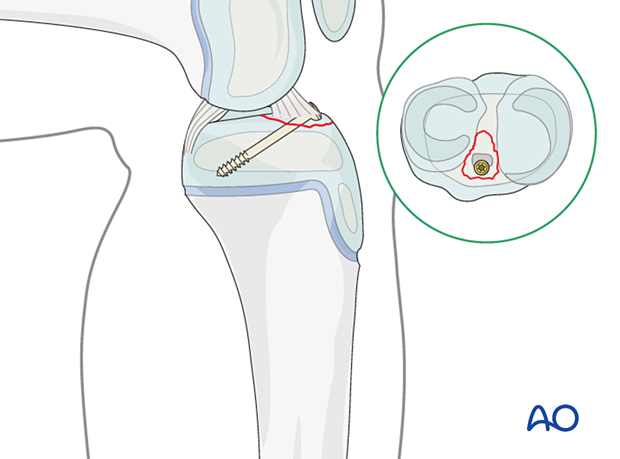
Alternative: retrograde lag-screw fixation
Fixation of a solid avulsion fragment can be performed with a small cancellous screw.
The entry point should be proximal to avoid injury to the physis.
6. Final assessment
Confirm reduction of the fragment with arthroscopy and an image intensifier and tension of the ACL with clinical examination.
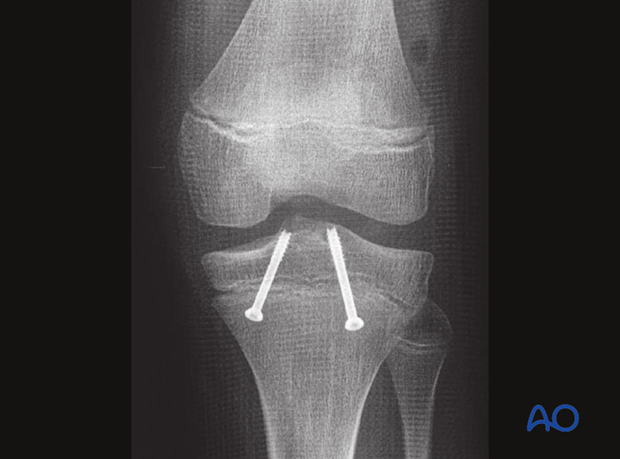
This lateral view x-ray shows the case of a tibial spine avulsion stabilized with two retrograde lag screws.

AP view x-ray of the same case
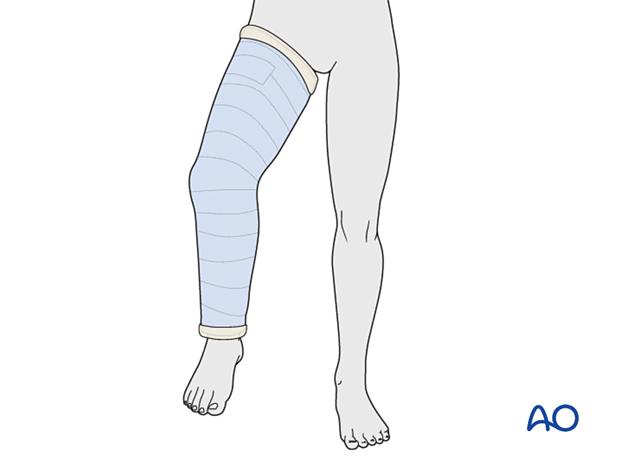
7. Immobilization
Depending on the stability of fixation, a cylinder cast with the knee flexed to 20°–30° may be applied for 4–6 weeks.
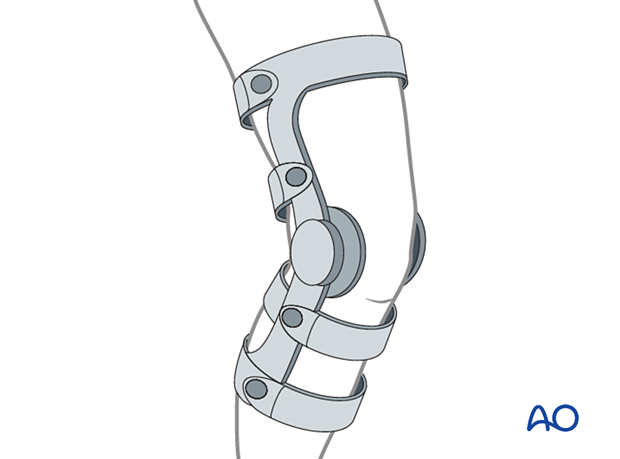
Alternatively, a hinged knee brace may be used with a gradually increasing range of motion over 6 weeks, with the patient instructed to remain touch-weight bearing.
8. Aftercare
Immediate postoperative care
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up
The first clinical and radiological follow-up is usually undertaken at 6 weeks.
Long-term follow up with clinical assessment of ligament stability is mandatory because of possible residual ACL insufficiency.
Growth disturbance is rare as the fracture usually does not involve the physis. Growth arrest of the tibial apophysis may result in recurvation malalignment. This should also be checked in a long-term follow-up (ca 2 years after trauma).
Implant removal
Implants are usually removed after 3–6 months.













