External fixation for temporary stabilization
1. General considerations
Principles of modular external fixation
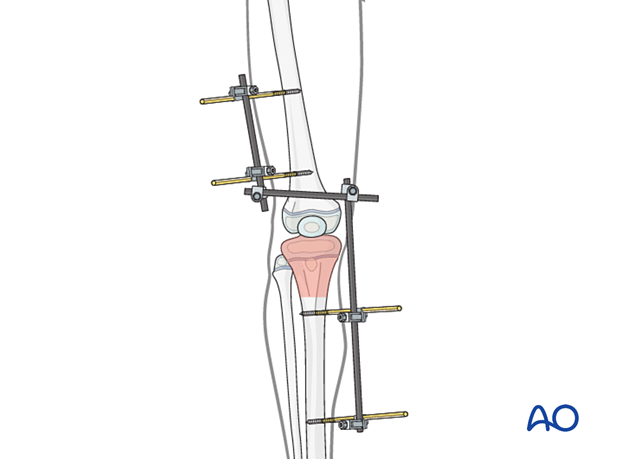
An external fixator in proximal tibial fractures spans the knee and is used mainly for temporary stabilization. It is applied to the femur and the tibia, and the fracture zone is not disturbed.
The versatility of a modular external fixator is an advantage in the management of children’s fractures and can accommodate age-specific variations in fracture biology and anatomy.
Provisional reduction is initially achieved with distraction.
Details of external fixation are described in the basic technique for application of modular external fixator in children.
Specific considerations for proximal tibial fractures are given below.
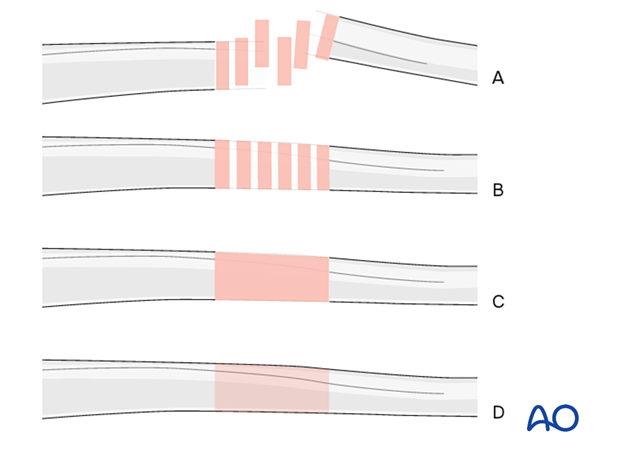
Throughout this section generic fracture patterns are illustrated as:
- Unreduced
- Reduced
- Reduced and provisionally stabilized
- Definitively stabilized
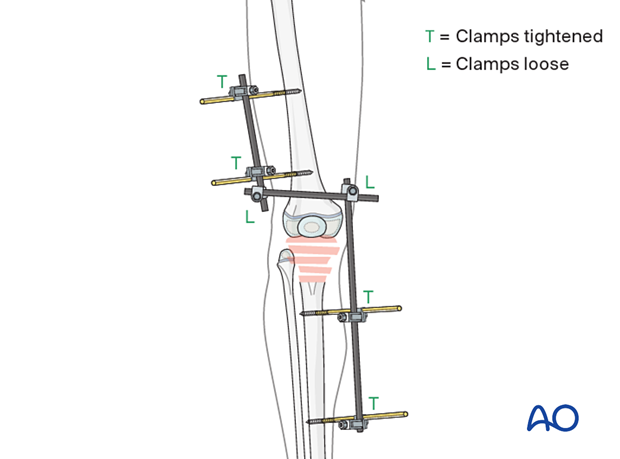
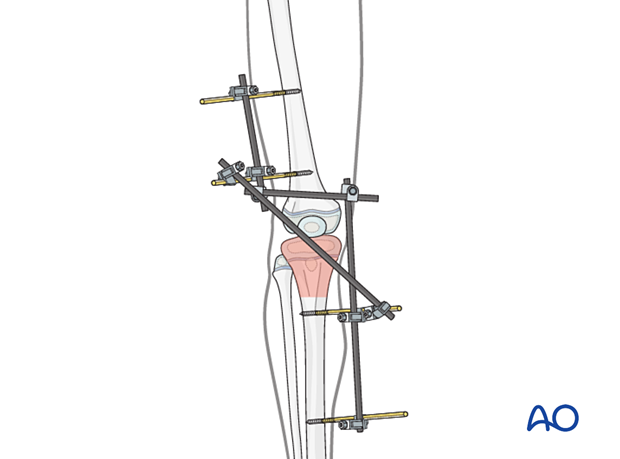
External fixator construct for temporary fixation
If the external fixator is used for temporary stabilization, the construct should provide a large enough window for definitive osteosynthesis. The tibial rod may be inclined laterally to leave enough space for medial osteosynthesis, or medially for lateral fixation.
Pin size in tibial fractures
External fixation is suitable for all ages, but the pin diameter must be appropriate to the size of the bone.
Pins with a thread diameter of 4.0–6.0 mm are suitable for the femur. Pins with a thread diameter of 3.0–4.0 mm are suitable for the tibia and should typically be between ¼ and ⅓ of the external bone diameter.
2. Patient preparation
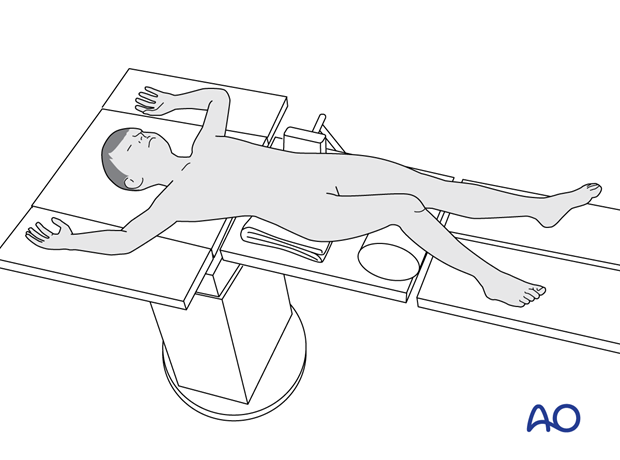
Place the patient in a supine position without traction on a radiolucent fracture table, with a bolster under the ipsilateral flank.
3. Approaches for safe pin placement
For pin placement use the safe zones and be familiar with the anatomy of the thigh and lower leg.
4. Pin insertion
Pin placement in the femur
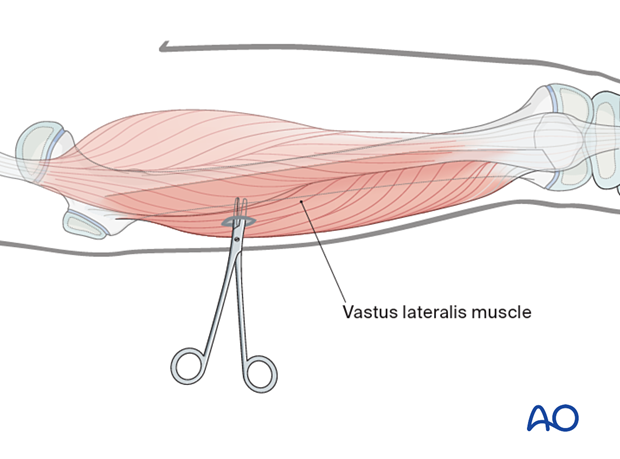
The safe zone for the femur is lateral.
Blunt dissection of the soft tissues and the use of small retractors will minimize muscular damage.
Using a straight clamp, prepare a channel for the insertion of the pin.
Pin placement in the tibia
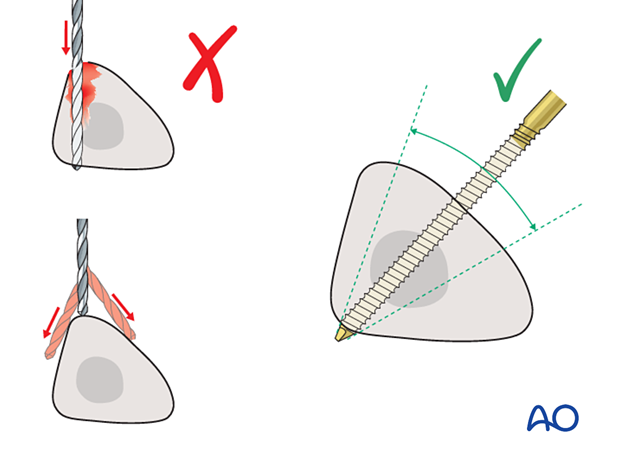
The anteromedial tibial surface is recommended for pin placement.
Pins must not interfere with definitive fixation.
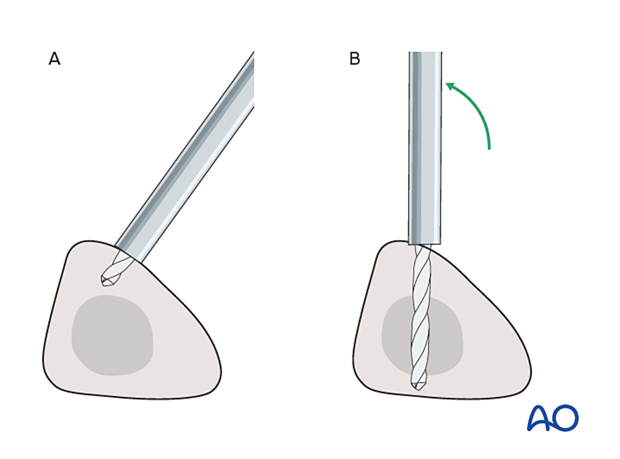
Drilling may be associated with excessive heat generation.
There is also a risk that the drill bit may slip medially or laterally, damaging the soft tissues.
A trajectory of 20°–60° relative to the sagittal plane for the proximal fragment and 30°–90° for the distal fragment is recommended.
If plate osteosynthesis is planned as a later, definitive procedure, the pins may be placed more anteriorly.
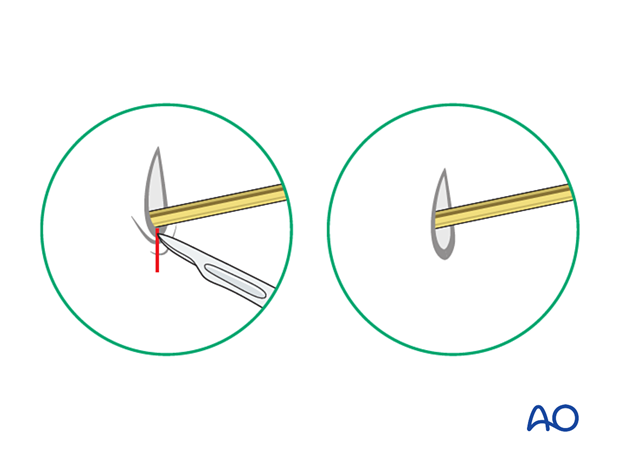
The drill bit is initially placed with the tip just medial to the anterior crest, and with the drill bit perpendicular to the anteromedial surface (A).
As the drill bit starts to penetrate the surface, the drill is gradually moved until the drill bit is in the desired plane (B).
This should prevent the tip from sliding down the medial or lateral surface.
5. Fixator construction
Fixator assembly
Attach the appropriately sized rods to the proximal and distal pins and tighten the rod-to-pin clamps.
Loosely apply a connecting rod to the two partial frames.
6. Reduction and fixation
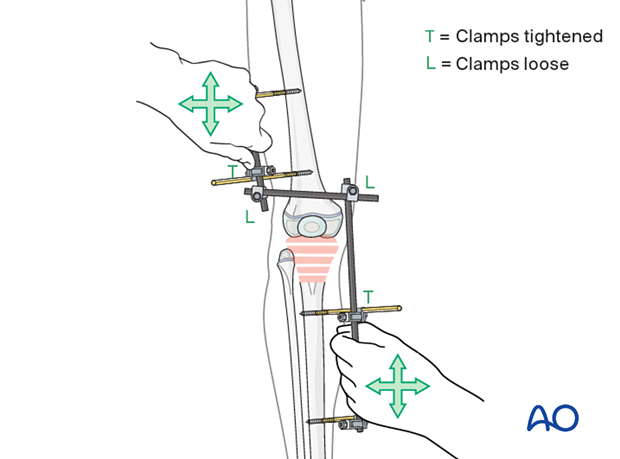
Reduction manipulating the partial frames
Reduce the fracture with traction and manipulation of the distal segment. Stabilization is more important than alignment.
Tighten the rod-to-rod clamps with the knee in a slight flexion.
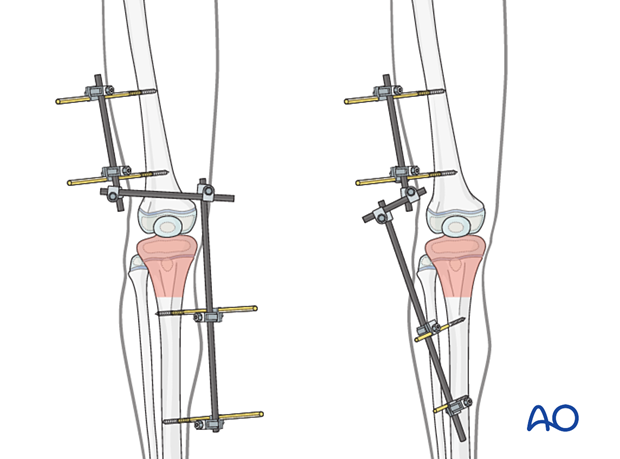
Additional rod
An additional rod may be applied to the construct to increase stiffness.
Pin sites
Check the skin at all pin sites and incise if tethered.
Dress the pin sites to prevent skin motion.
7. Final assessment
Check pin placement and fracture alignment under image intensification.
Use clinical examination to check lower extremity alignment.
8. Aftercare
Pin-site care
Pin-care protocolThere is no universally agreed protocol for pin-site care.
The following points are recommended:
- Pin-site care should continue until removal of the external fixator.
- The pin sites should be kept clean.
- Crusts or exudates should be removed.
- The pins may be cleaned with water, saline, disinfectant solution or alcohol. The frequency of cleaning varies from daily to weekly.
- Ointments or antibiotic solutions are not recommended for routine pin-site care.
- Pin sites do not need to be protected whilst showering or bathing with clean water but should be dried immediately.
Initial management is with oral anti-staphylococcal antibiotics.
In case of pin loosening or unresponsive pin site infection, the following steps should be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for microbiological culture to guide appropriate antibiotic treatment.
Internal fixation following an infected external fixator pin has a high risk of infection and should be avoided unless no reasonable alternative is available.
Follow-up
The patient should be seen 5–7 days after surgery for a wound check.













