Splint immobilization
1. Principles
General considerations
Proximal forearm fractures require immobilization with a splint to control forearm rotation and therefore decrease the risk of displacement.
Pediatric considerations
Simple application of a splint is performed without sedation in older children and in compliant younger children.
The environment should be one in which the child and the parents/carers are comfortable.
Important considerations include:
- A child-sensitive approach
- A child-friendly clinical area
- Careful explanation of the procedure, in language that is understood by the child and the parents/carers
- Availability of all equipment and material
When a procedure including manipulation is required, general anesthesia or conscious sedation is usually necessary.
2. Preparation for splint application
Equipment
- Examination couch
- Tubular bandage (40-80 mm wide, depending on the size of the child)
- 2-4 rolls of padding (40-150 mm wide, depending on the size of the child)
- 2-8 plaster of Paris (POP) or synthetic fiberglass bandages (40-150 mm wide, depending on the size of the child)
- Bucket with cold water
- Protective aprons for the team members and the child
Patient preparation
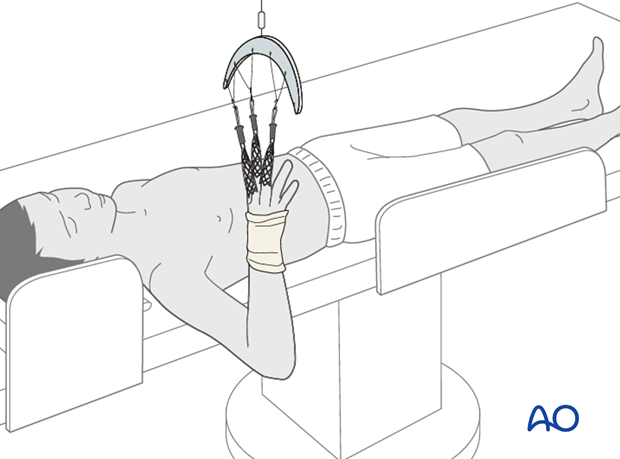
This procedure is normally performed with the patient in a supine position.
Pearl: Holding the arm using finger traps as illustrated allows easy manipulation, reduction, imaging, and mobilization for a surgeon working without an assistant.
To avoid damage to the skin of the fingers ensure that the pressure is evenly distributed, and that prolonged or excessive force is avoided.
3. Splint application
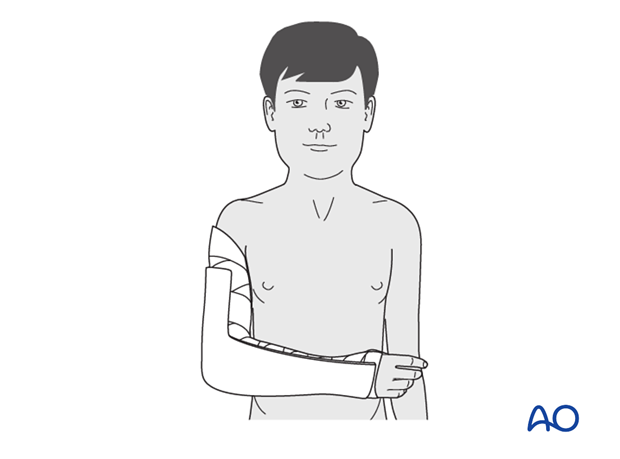
Application of cast padding
Hold the elbow in 90° flexion and the forearm in neutral rotation.
Wrap cast padding around the upper arm, elbow, forearm and hand, as far as the transverse flexor crease of the palm (the MP joints are left free). According to surgeon’s preference a tubular bandage may be applied to the arm beneath the padding.
Make sure that the epicondyles of the humerus and the antecubital area are well padded.

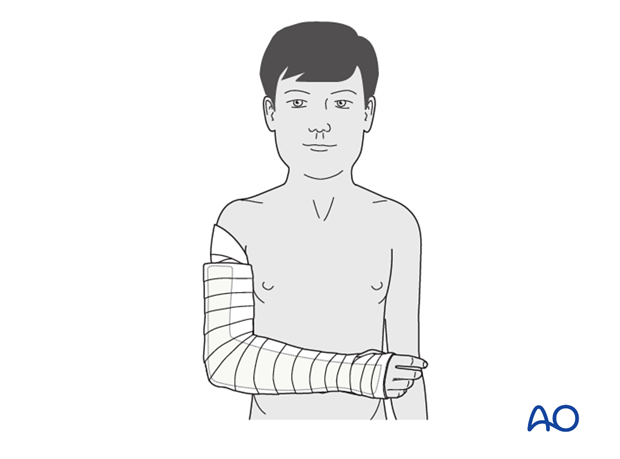
Application of splint
Apply a splint of fiberglass, or plaster, on the posterior aspect of the arm and forearm. It should be wide enough to cover more than half the circumference of the arm and forearm.
Secure the splint with a noncompressive bandage.
Ensure that this is not tight, to accommodate subsequent swelling.
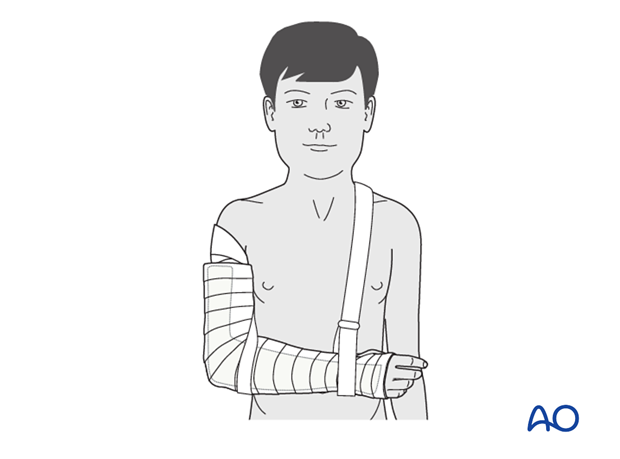
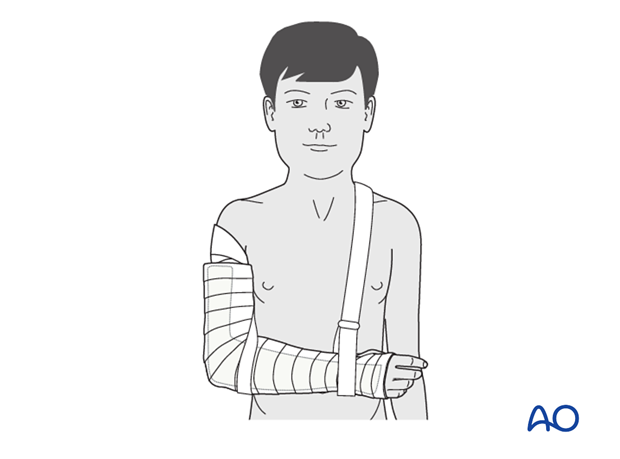
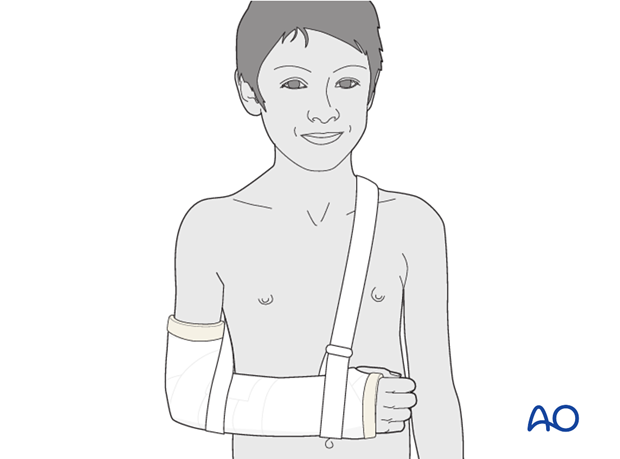
Sling
The injured arm and splint are supported with a sling around the shoulder.
4. Aftercare following immobilization
Duration of immobilization
Metaphyseal and epiphyseal fractures of the proximal radius and ulna usually require 2-4 weeks of immobilization for adequate healing.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
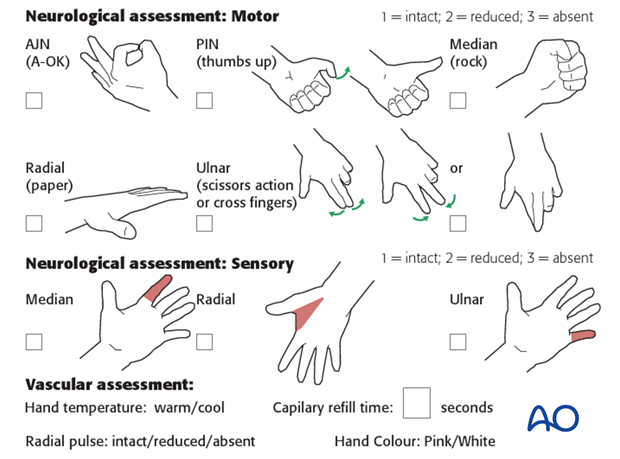
Neurovascular examination
The child should be examined after casting, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome in a child in a cast or splint:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
When the child is discharged from the hospital, the parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
Follow-up
AP and lateral x-rays may be taken to assess fracture position at intervals decided by the fracture configuration and age of patient.
Loss of reduction can be treated by conversion to internal fixation.
See also the additional material on complications.
Removal of cast or splint
Fractures treated by immobilization should have the cast or splint removed 2-4 weeks after the injury.
Clinical assessment and x-rays without cast are used to judge adequate healing.
Recovery of motion
As symptoms recover, the child should be encouraged to remove the sling and begin active movements of the elbow and forearm rotation. See also the additional material on elbow stiffness.
The majority of motion is recovered rapidly and within two months of cast or splint removal.
The older child may take a little longer.
Once the child is comfortable, with a nearly complete range of motion, (s)he may incrementally resume noncontact sports.
Resumption of unrestricted physical activity is a matter for judgment by the treating surgeon.













