Radiological assessment
1. Preliminary remarks
Radiological assessment of the injured hip includes plain x-rays, image intensification (including 3-D reconstruction), computerized tomography (CT) and, in some cases, magnetic resonance imaging (MRI).
The purpose of radiological assessment is to:
- Identify the location, nature and extent of injury
- Classify the injury pattern
- Assess the degree of displacement
- Assess stability
- Identify any additional injuries
- Identify pre-existing contributory pathology (eg, cysts)
- Exclude chronic pathology (eg, SCFE, Perthes’ disease, and OCD)
2. Plain x-rays
Introduction
According to the level of pain and the compliance of the child (and the parents), satisfactory radiological examination can be difficult and requires patience, time and an experienced and specialized radiographer.
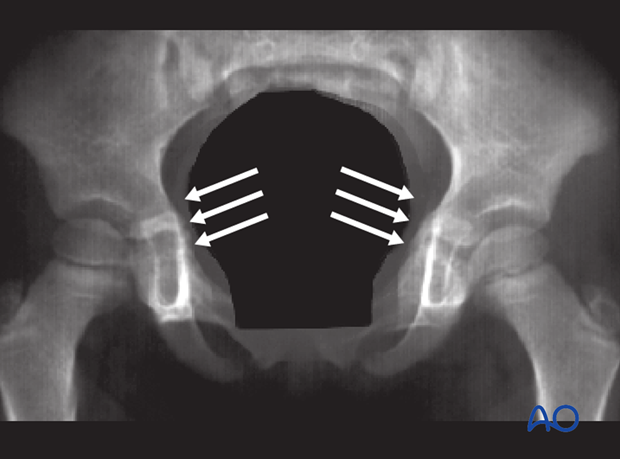
Good quality x-ray images in two planes (antero-posterior (AP) and lateral) must be obtained in all patients with suspected hip trauma.
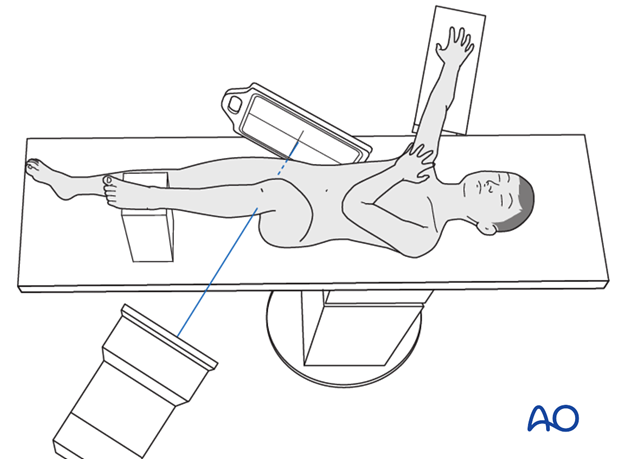
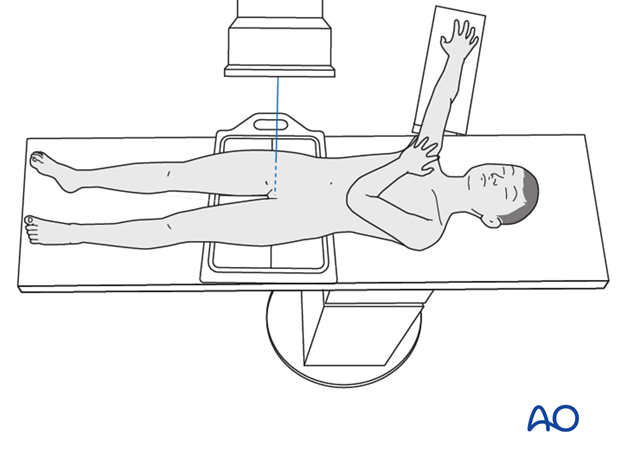
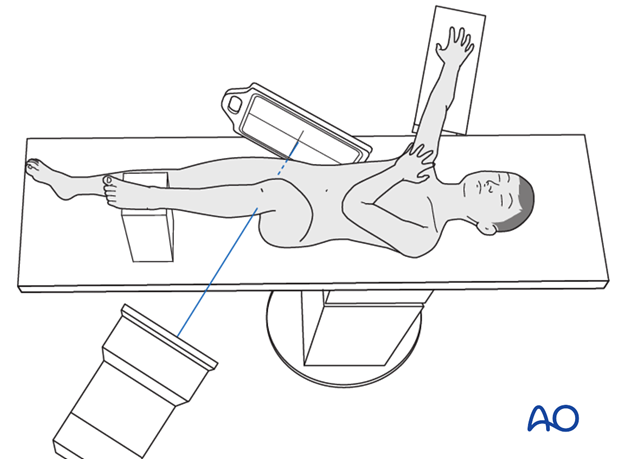
Note: In trauma situations, it is not always possible to turn the patient, and hence a cross-table lateral view can be used (as illustrated).
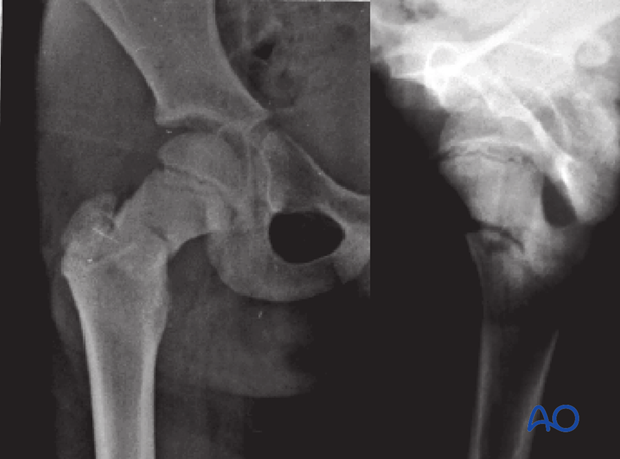
Case example 1
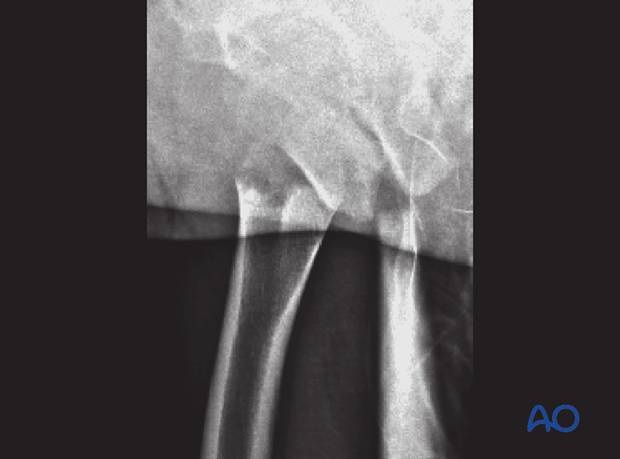
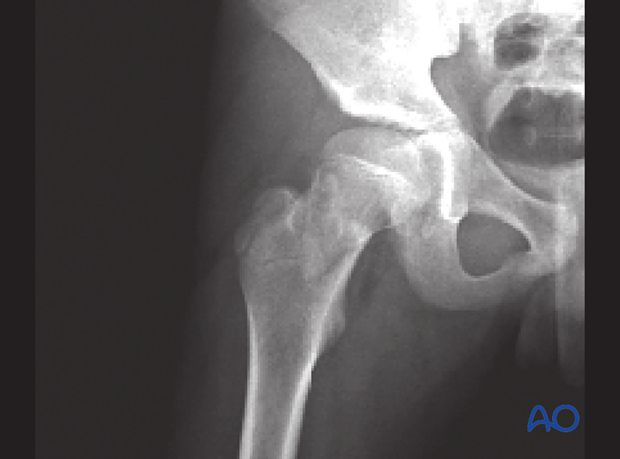
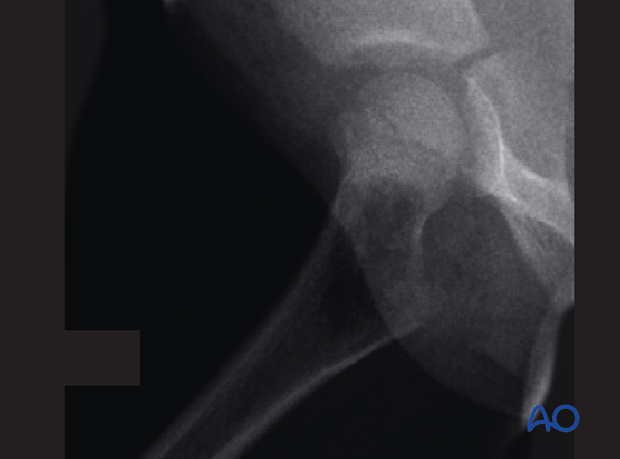
A femoral neck fracture in a 7-year-old child.
On the left is an AP x-ray and on the right a somewhat lateral or oblique x-ray. This view gives no clear information about the fracture.

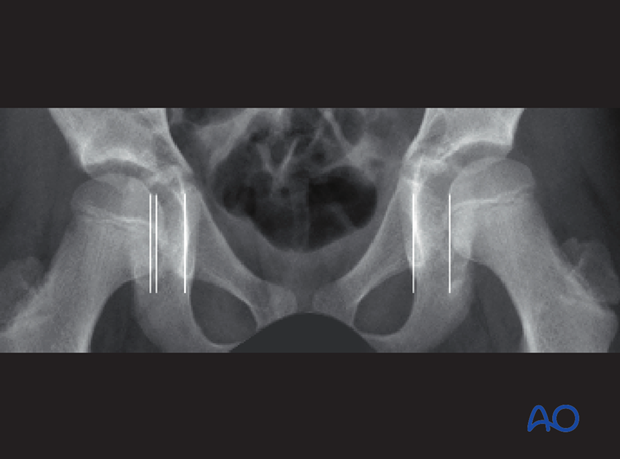
These two x-rays from the same patient are examples of a true AP (left) and lateral, cross table view (right).
These properly centered views provide a much clearer view of the fracture.
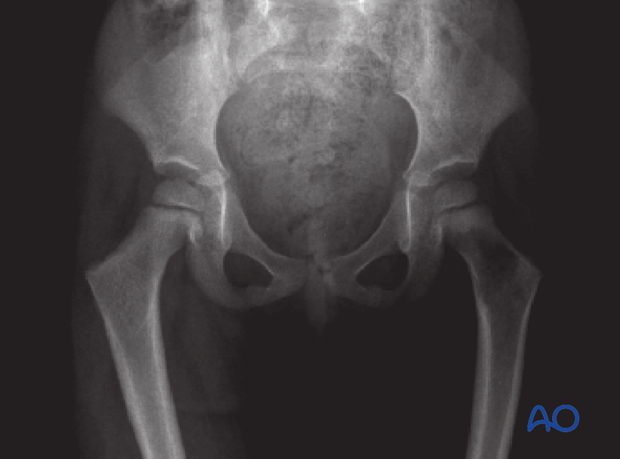
Case example 2
This AP view of a basicervical hip fracture does not show the true displacement in the frontal plane.
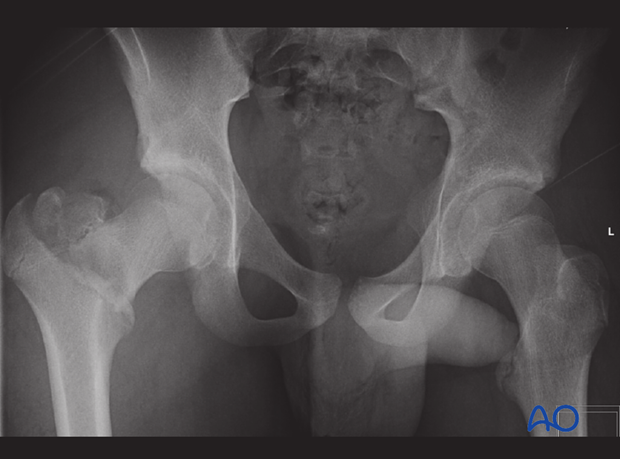
A cross table x-ray of the same injury shows the actual degree of angulation and displacement of the fracture.
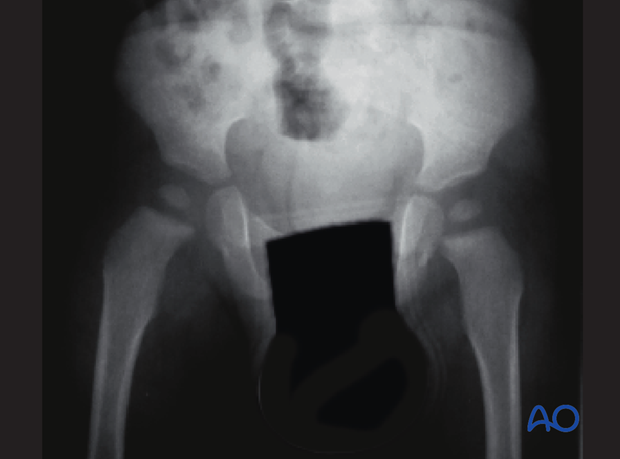
Plain AP x-ray
The first step in the radiological examination is a plain antero-posterior (AP) x-ray of the pelvis, or hemi-pelvis, including the proximal femur, according to the history and the location of pain.
Whenever possible, a cross-table x-ray technique is recommended to avoid pain associated with moving the patient.
The following radiological features should be assessed:
- Symmetry of the pelvis
- Morphology and structure of the pelvic bone
- Morphology and structure of the proximal femur
- Relationship between femoral head and acetabulum
- Indirect signs (muscle swelling, capsular distension etc.)
- Distortion of the intramuscular fat layers
In the AP view, the following features can be seen:
- Symmetry of the pelvis, indicating a well-centered image and no displaced bony injury of the pelvis
- Symmetrical joint space between femoral head and the acetabulum, excluding any sizeable joint effusion, or fragment entrapped in the joint
Note: Ultrasonography should be used to detect minor joint effusion

- Asymmetrical joint space, indicating interposed soft tissue, entrapped cartilage fragments, hemarthrosis or joint effusion
Note: This is an indication for an MRI examination.
- Callus formation at the tri-radiate cartilage, indicating a nondisplaced injury of the physis
The same patient developed dysplasia of the hip due to premature closure of the tri-radiate cartilage.

- Fracture of the base of the femoral neck
- Simple, unicameral bone cyst.
Note: Reduced bony density in the femoral neck.
- Simple, unicameral bone cyst
Note: Asymmetrical radiolucency, widening and an osteolytic zone can be seen in the right femoral neck-shaft junction.
- Reduced transparency of the soft tissues, indicating swelling around the right hip.This can be seen as higher relative density of the bone compared to the soft tissue
3. CT imaging
Introduction
The dose of ionizing radiation from a CT scan of the pelvis is significantly higher than from a standard x-ray and contributes to life-time risk. Furthermore, in an acute trauma case, with a restless/anxious child, it may be very difficult to obtain good quality images without general anesthesia.
It is therefore essential to consider very carefully whether a CT scan is essential and would be likely to yield important information that cannot be obtained from plain x-rays, or MRI, and which will alter the management of the injury.
If one cannot wait for an MRI in an acute situation, CT scans may be indicated.
When requesting a CT scan, it is important to explain carefully to the radiologist where to focus and what question needs to be answered.
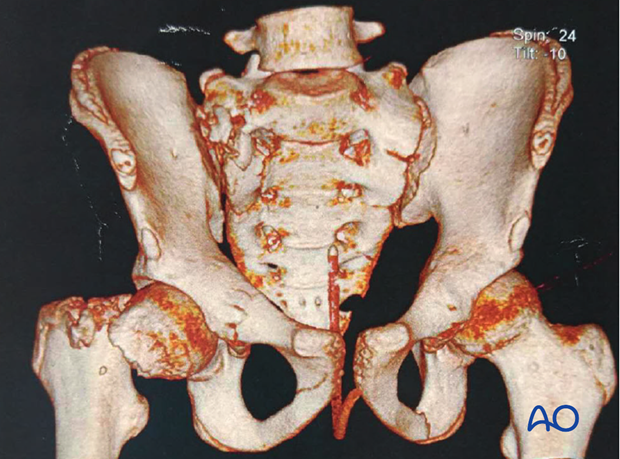
CT allows visualization of all fracture lines and is also the best technique for quantifying displacement of the fracture (distance and direction).
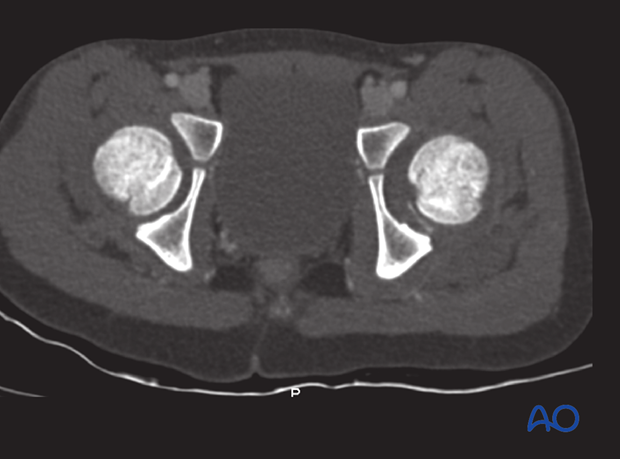
CT also offers the possibility of 2-D–MPR (multi-planar-reformation) for better analysis of the fracture lines. This allows better preoperative planning.
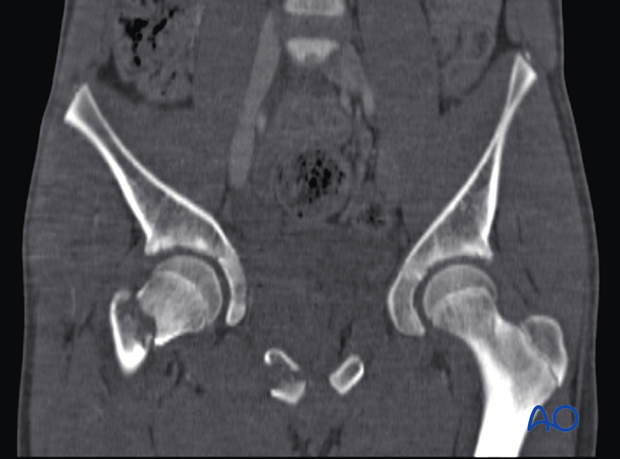
Note: 3-D reconstructions only demonstrate the surface of the bone and do not provide accurate information on the configuration of the fracture. These images can be useful as an explanation of the pathology for the patient/parents.
4. MRI
Introduction
MRI is not part of the primary imaging in acute trauma.
Examination time for MRI is much longer than for CT and the biggest challenge is for the child to stay still for the required time.
MRI is more likely to be indicated some days after an acute trauma for further detailed analysis of the injury, especially to the soft tissues.
In an acute setting, general anesthesia, solely for an MRI examination, should be avoided.
MRI is less informative than CT scans for bony structures.
The following features can be observed on an MRI:
- Bone edema, indicating bony injury without fracture, or cancellous microfractures
- Swelling, indicating soft tissue insult
- Accumulation of fluids
- Hematoma
- Ligaments
- Cartilage
- Incomplete fracture lines (fatigue fractures)
- Vascular structures (only with IV contrast)
- Tumors and cysts
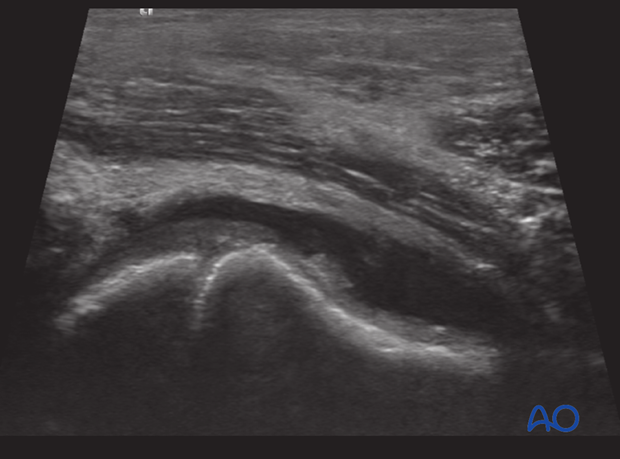
5. Ultrasonography
Ultrasonography is a useful, noninvasive and painless examination for children. It can be repeated without any side effects, or complications.
Ultrasonography can also be used as a dynamic examination (by moving an extremity, or joint).
Ultrasonography has a high sensitivity for fluids (swelling and soft tissues in general).
The accuracy of ultrasonography is closely related to the experience of the ultrasonographer.
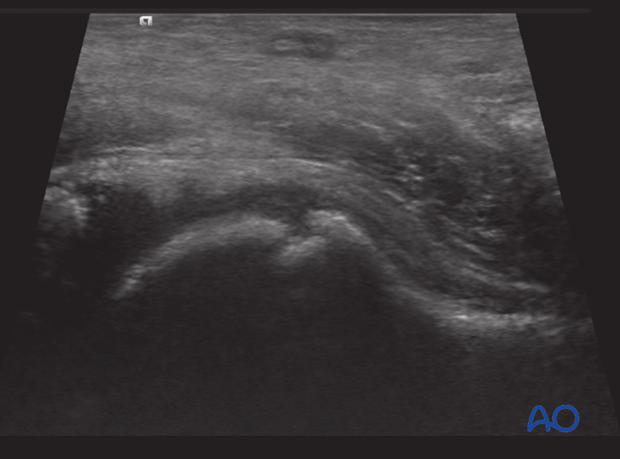
Ultrasonography can demonstrate:
- Haemarthrosis or joint effusion
- Ligamentous integrity
- Incomplete fracture lines