Hip spica
1. Introduction
Material
- Tubular bandage sized both for leg and for body
- Cast padding
- Felt
- Casting material: synthetic material, if available, is preferable to plaster of Paris, for sanitary reasons

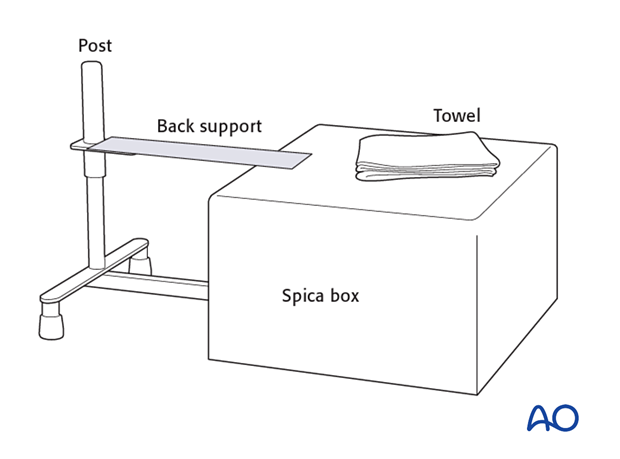
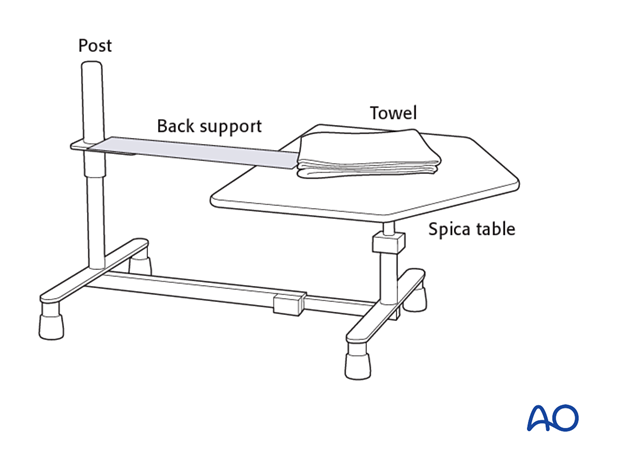
Equipment
- Hip spica box or table
- Folded towel as abdominal spacer
Dressing
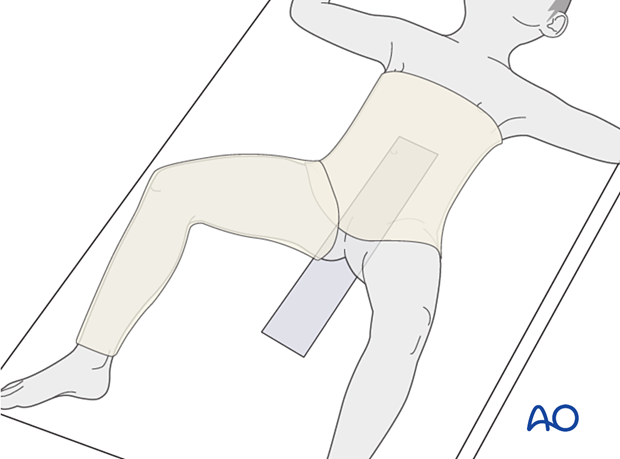
A generous length of tubular bandage is cut to dress the injured leg and a larger diameter tube for the torso. Sewing the two parts of the tubular bandage together prevents separation of the bandages as the child is moved.
The back support for the spica box is placed inside the torso tubular bandage, directly against the skin of the child's back.
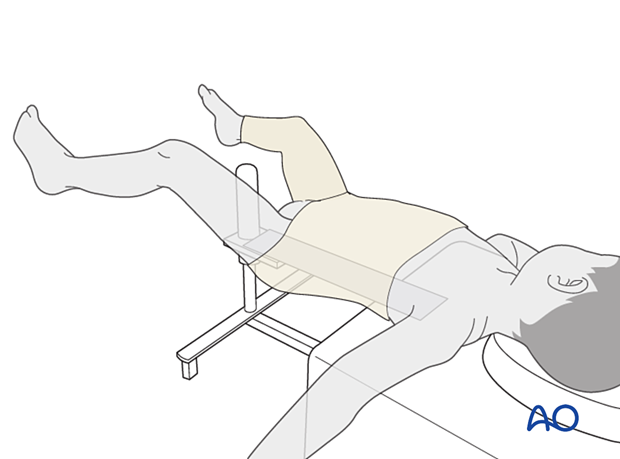
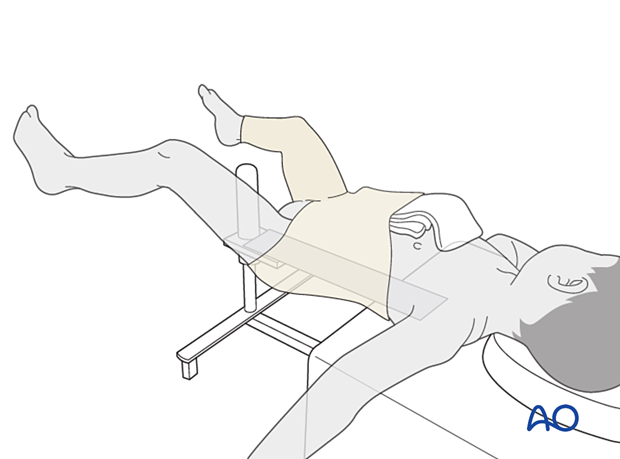
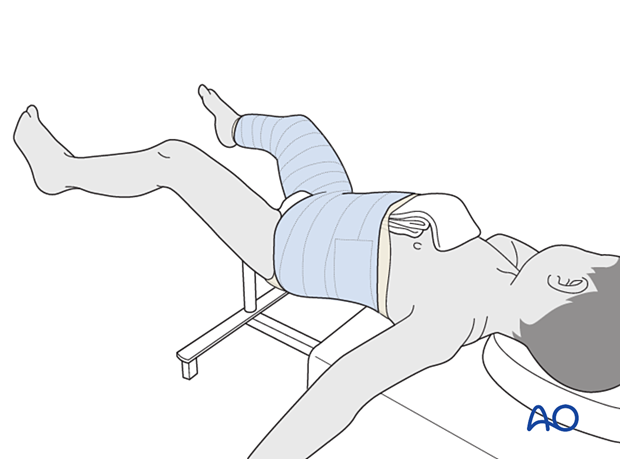
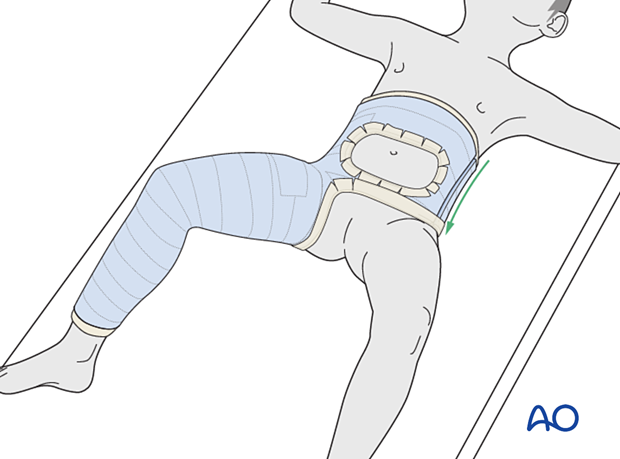
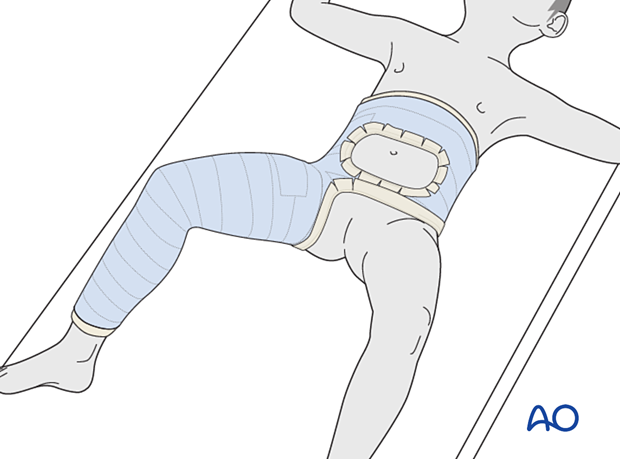
Placement on hip spica box
The anesthetized child is transferred onto the hip spica box. It should be ensured that enough people are available to help positioning and stability.
The child’s sacrum should rest on the back support with its perineum against the padded post. The shoulders should be supported by the spica box leaving almost the entire torso free for casting.
The back support can be secured to the apparatus with tape.
Pitfall: Avoid inadvertent extubation during transfer and casting. Discuss airway management with the anesthetist beforehand.
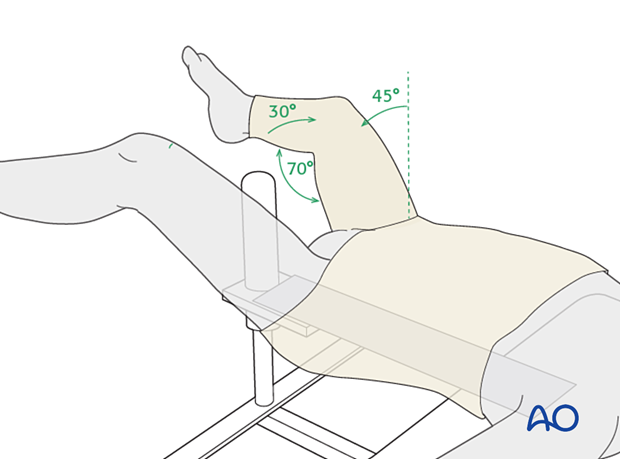
Leg position
For a younger child, the most convenient position for a protective spica cast is about 45° of hip flexion, 30° of hip abduction, and 70° of knee flexion. This allows for comfort whilst lying and also sitting.
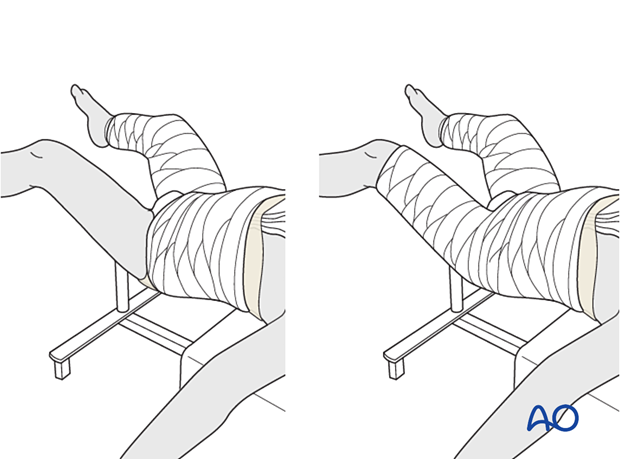
Single-leg vs two-leg spica
A single-leg spica is adequate for most circumstances; some surgeons prefer to apply a short leg on the uninjured side as this can help to make the cast more stable.
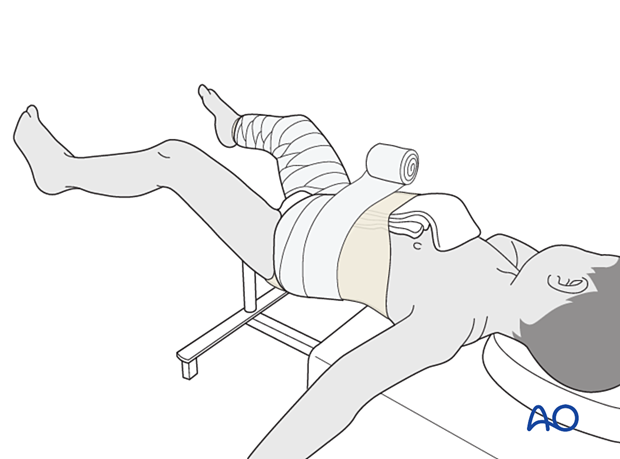
2. Casting
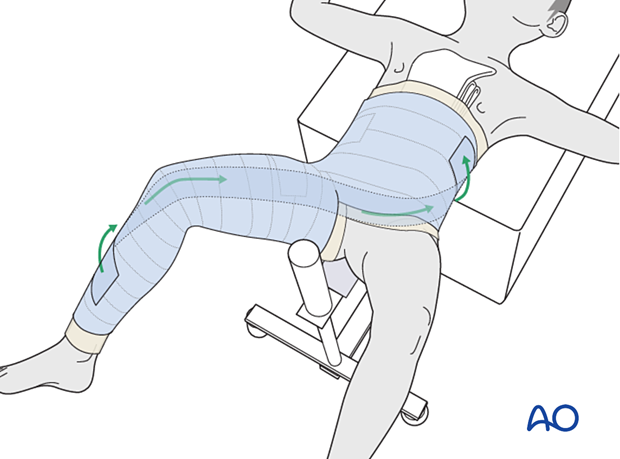
A folded towel is placed over the central abdomen, inside the tubular bandage, to create space in the cast for breathing. The tail of the towel is brought towards the neck for ease of removal.
A layer of cast padding is applied, using a larger width for the body and a narrower one for the leg(s).
The cast extends from the nipple line, or just below, to just above the malleolus of the ipsilateral ankle.
Optionally, thick felt can be added over the padding where the chest and leg edges of the cast will be.
A first layer of cast material is applied to leg and body sections, taking care to connect leg to body securely, in a figure of eight (spica technique).
Reinforcing slabs of casting material may be applied between the body segment and the leg segment.
Tubular bandage and padding are folded over the edges before applying the final layer of casting material.
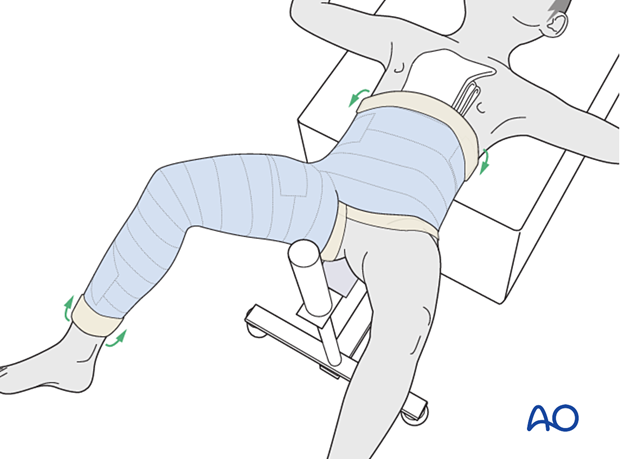
The child is transferred from the spica box and the abdominal towel and the back support are removed from the cast.
The edges of the cast are trimmed, as necessary, to allow flexion of the opposite hip and adequate access to the perineal area.
Optionally, waterproof adhesive tape is added to the perineal edge of the cast.

A hole may be cut in the abdominal portion of the cast to allow for greater comfort with breathing and eating. This is especially important for older children.
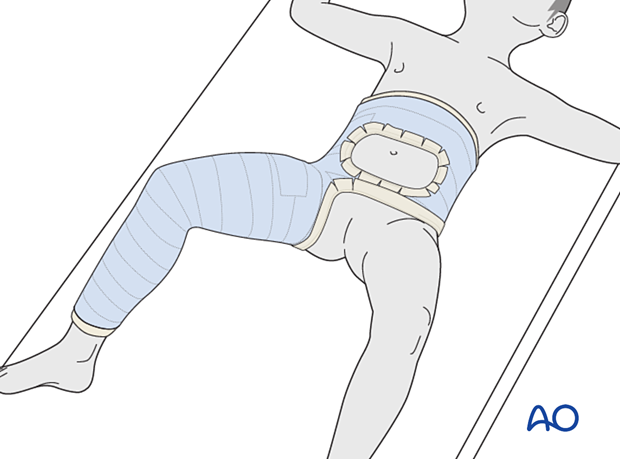
If the child has respiratory distress from a cast that has been applied to tightly, it can be split down the side and spread to allow for expansion or it can be removed and reapplied.
3. Aftercare
Introduction
Hip spica is only likely to be used in the treatment of small children with proximal femoral fractures.
For larger children, internal fixation should be used even for nondisplaced fractures.
Immediate care
After application, the spica should be trimmed to allow adequate space for bodily functions. The edges of the spica should be padded and waterproofed.
Diaper care
Generally, a hip spica should allow space for a small diaper inside the plaster and a large one outside the plaster. The diapers should be positioned to prevent soiling of the spica.
Washing
The spica is not waterproof. Bathing and showering should not be attempted. Hair washing should be done very carefully.
Skin care
No skin products should be put inside the spica. Only skin that can be seen should be moisturized.
Transport
Both the child and the spica must be lifted. A special car seat will be required. The child may be placed in a stroller or buggy.
In this circumstance, the parents/carers are advised to return to the healthcare provider.
Length of time in spica
The length of time in the spica depends on the age of the child and the healing of the fracture. A proximal femoral fracture in a child aged below 4 years should always be healed in 6 weeks.
Growth
The child will continue to grow and the tightness of the spica should be monitored.
Follow-up x-rays
Nondisplaced fractures being treated nonoperatively should have early radiological follow-up. If the spica is being used for protection of fixation, x-rays are required only when planning removal.













