Immobilization with splint, brace, or cast
1. General considerations
After initial, immobilization, humeral shaft fractures may be treated nonoperatively with:
- U-slab splint (temporary treatment)
- Sarmiento Brace
- Hanging cast
Application of a splint or brace is performed without sedation in older children and in compliant younger children.
Fracture reduction requires sedation or general anesthesia.
The environment should be one in which the child and the parents/carers are comfortable.
Important considerations include:
- A child-sensitive approach
- Careful explanation of the procedure, in language that is understood by the child and the parents/carers
- Availability of all equipment and material
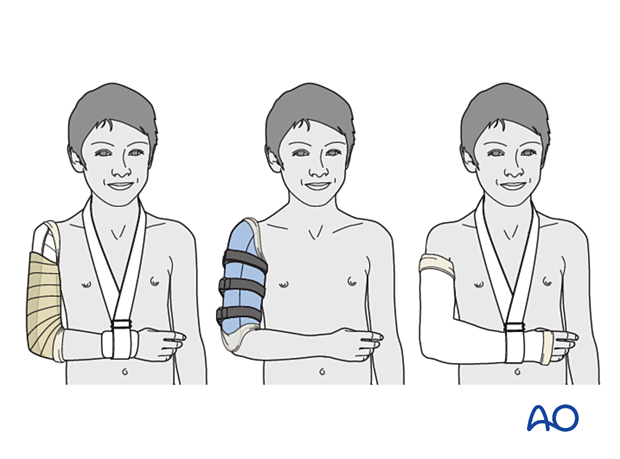
2. U-shaped/coaptation splint
Introduction
Immobilization in a coaptation splint (also known as sugar tong splint) stabilizes the fracture and supports the limb, whilst accommodating swelling in the immediate postinjury period.
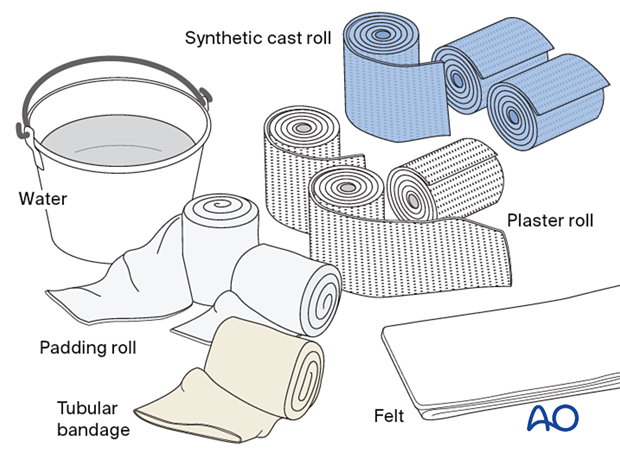
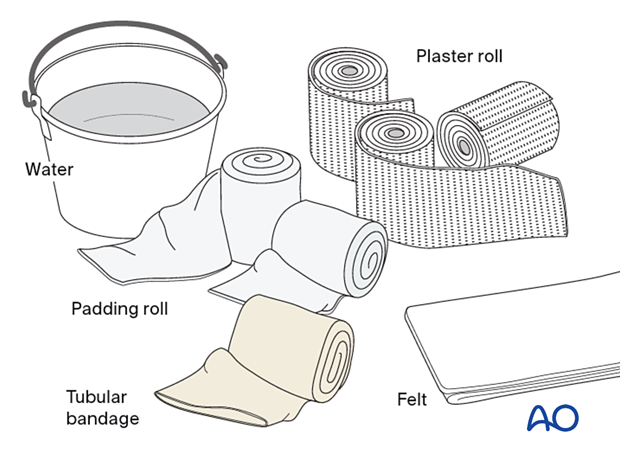
Material
- Tubular bandage (stockinette) of appropriate size
- Cast padding
- Felt
- Casting material: synthetic or plaster of Paris
- Water
The water temperature should ideally be between 22° and 25° C.
Splint application
Apply a stockinette up to the shoulder, slightly longer than the planned splint.
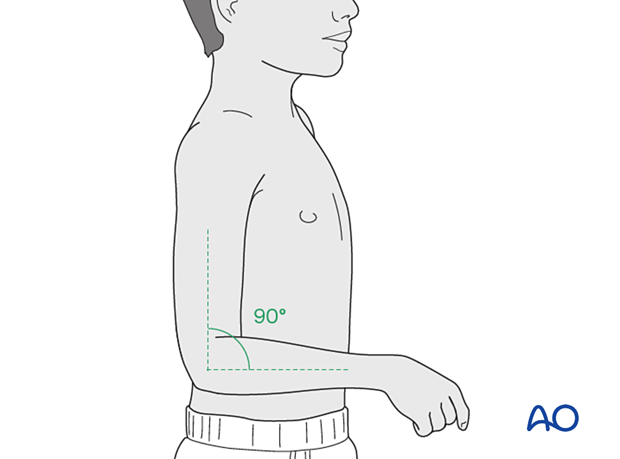
Ideally, the patient should be sitting, leaning slightly towards the injured side, with the elbow in 90° flexion.
While maintaining traction, wrap cast padding around the upper arm from axilla to elbow. Make sure that the epicondyles of the humerus and antecubital area are well padded.

Determine the length of the splint using the uninjured side, measuring between the medial aspect of the arm at the axilla, around the elbow and up to the acromioclavicular joint (except for very distal fractures).
Prepare a splint with 6–8 layers of plaster material in a width equal to diameter of the arm.
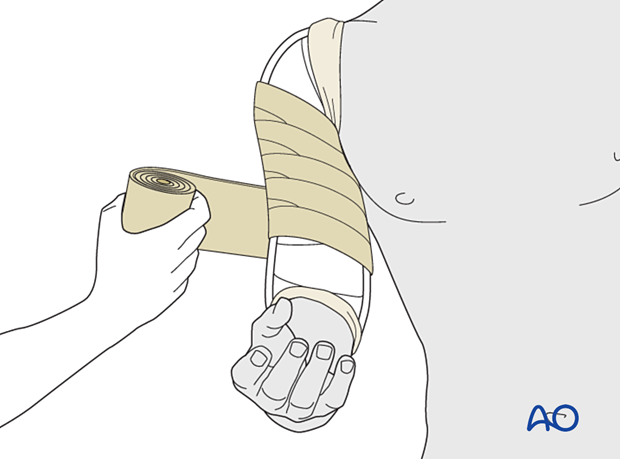
While maintaining traction, apply a splint of fiberglass, or plaster, in a U-shape, with padding under the axilla. Wrap it from the medial aspect of the arm near the axilla around the elbow and up to the acromioclavicular joint (except for very distal fractures).
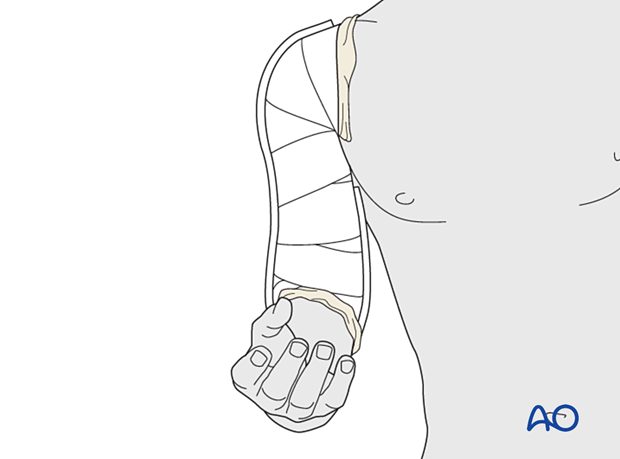
Secure it in place with an elastic bandage, that should not be too tight to allow for swelling.
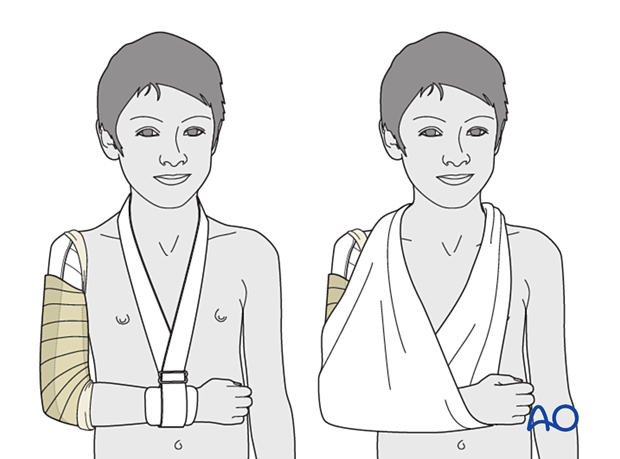
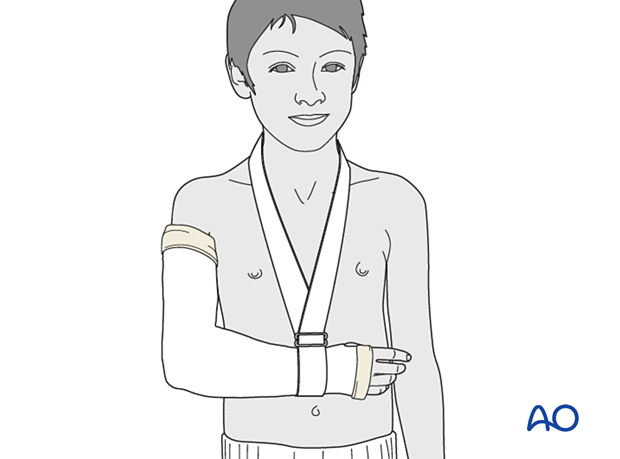
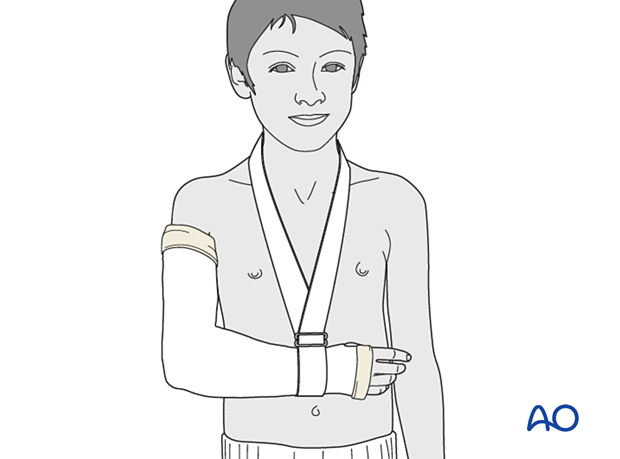
The injured arm and cast are supported with a collar and cuff or a sling.
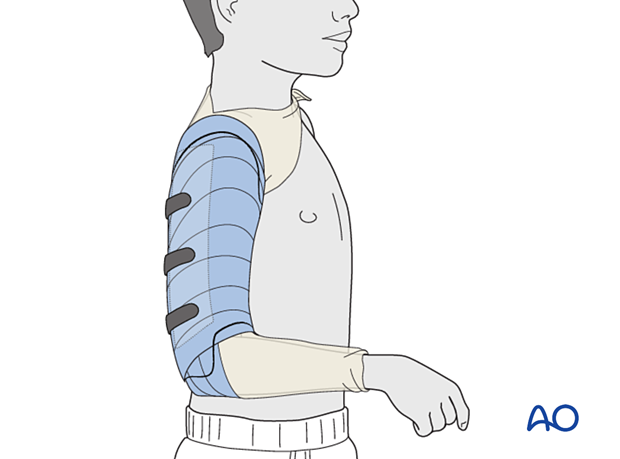
3. Brace application
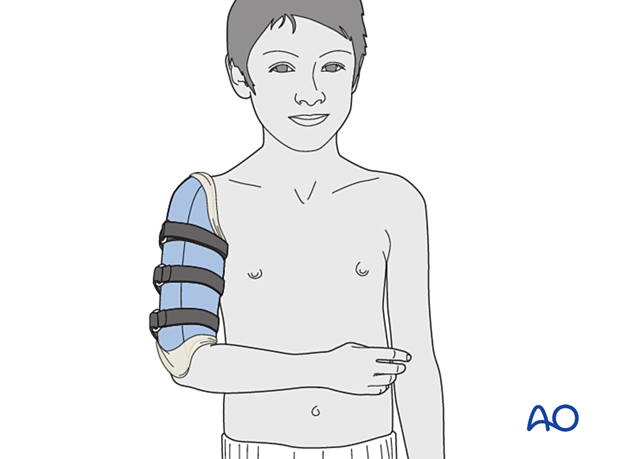
Braces allow for shoulder and elbow movement during rehabilitation.
Braces are available for older children. For younger children, a brace may be custom made with cast material.
The arm may initially be stabilized with a bandage.
AO video
Sarmiento humeral brace using synthetic casting materialIndications:
- Diaphyseal fractures of the humerus
- Not recommended for primary fracture care
Goal:
- Stabilization of the humeral shaft
Material
- Tubular bandage (stockinette) of appropriate large and small sizes
- Casting material (synthetic) – soft and hard
- Water
- Velcro strips
- Elastic bandage
The water temperature should ideally be between 22° and 25° C.

Seat the patient comfortably on a stool.
The affected limb hangs over the table, with 90° elbow flexion.
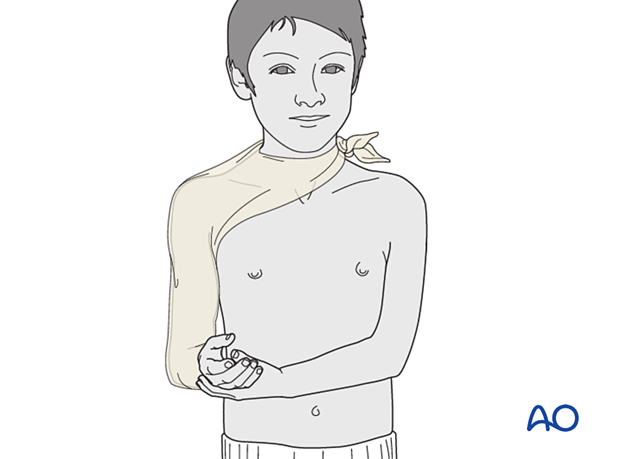
Cut two slits in one end of the large tube bandage, one long and one short. These slits allow application around the neck.
Apply the large tube bandage and tie around the neck.
Tighten the tube bandage to remove any wrinkles.
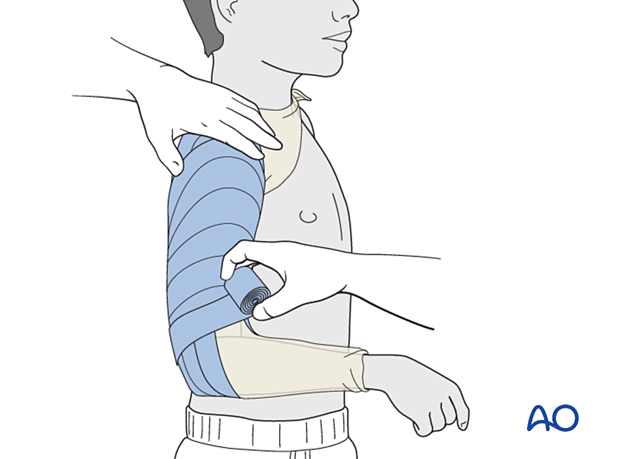
An assistant is needed to hold the shoulder and elbow in position for the rest of the procedure.
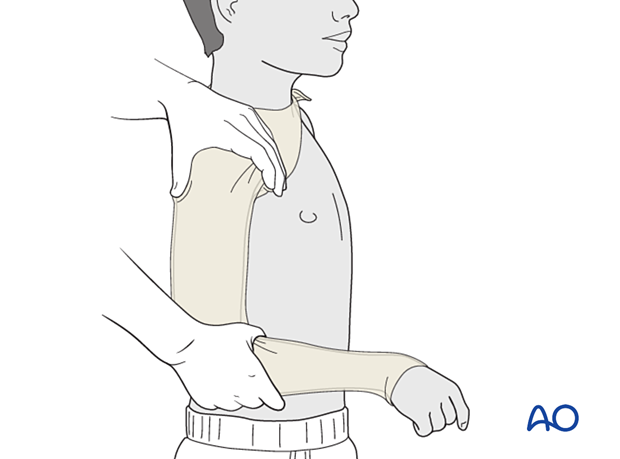
Apply the first layer of soft synthetic casting tape; the assistant holds the tape at the shoulder.
Wrap the soft synthetic casting tape twice from the elbow to shoulder.
Wrap the soft synthetic casting tape over the olecranon to hold the elbow at 90° flexion.
Wrap the rest of the upper arm using the half-overlapping technique.
Ensure there are no creases in the tube bandage on the inside of the elbow.
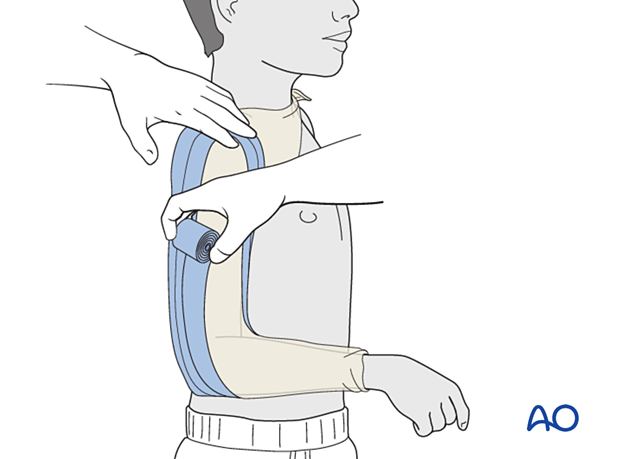
Make a rigid splint using the hard synthetic cast, apply it to the lateral aspect of the arm, and trim to the length of the humerus.
Add another layer of soft synthetic casting to hold the splint in place.
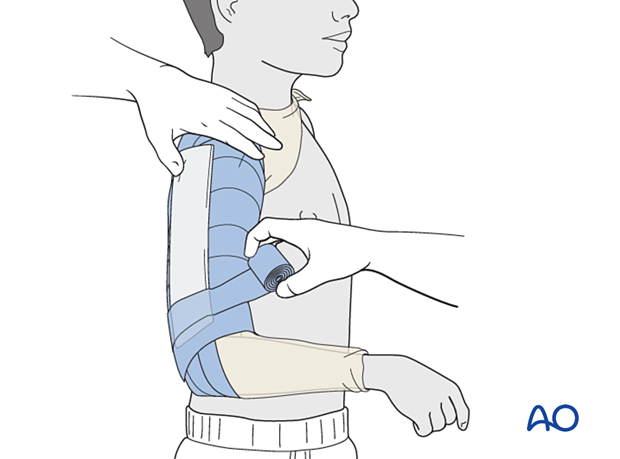
Submerge the elastic bandage in water; using a wet bandage accelerates the setting.
Apply the elastic bandage over the casting tape for two minutes and remove it before the cast has set.
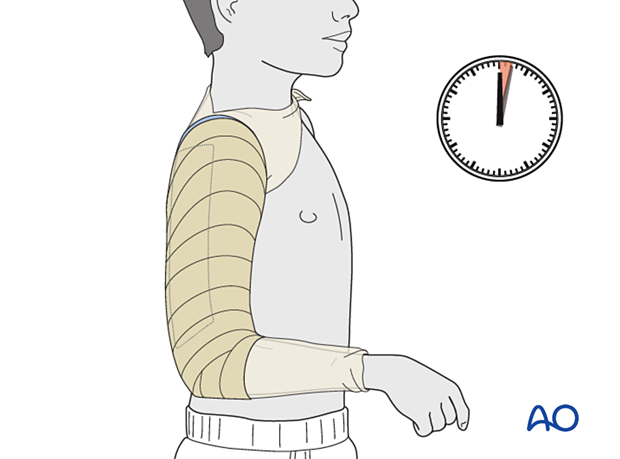
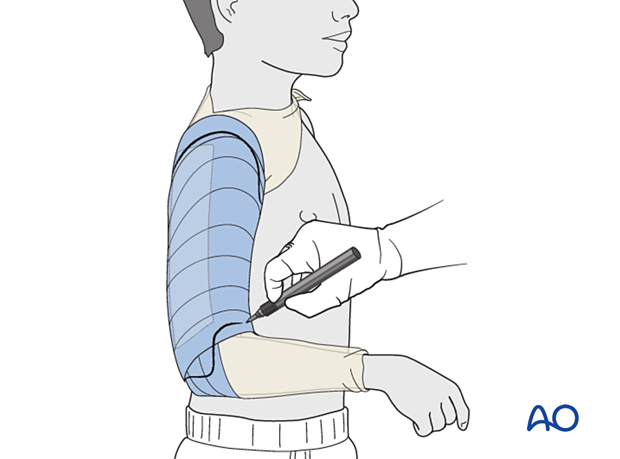
Mark the brace where it needs to be trimmed.
Ensure there is enough space at the axilla and shoulder.
Mark the epicondyles and the fold of the elbow.
Ensure the olecranon fossa is free.
Keep in mind:
- Skin irritation under the axilla
- Circulation
Apply three strips of adhesive Velcro (with loops).
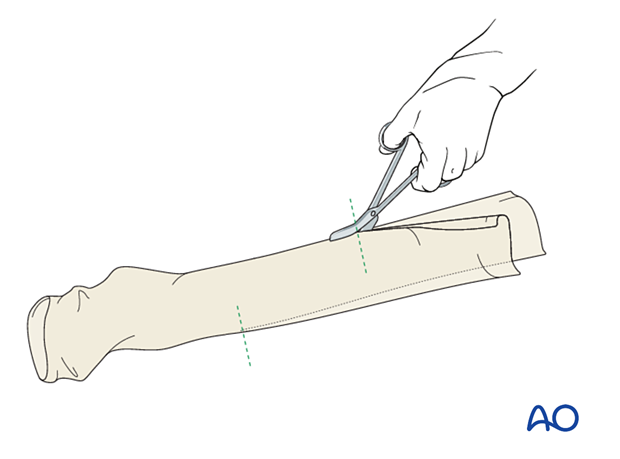
Splitting the soft synthetic casting tape
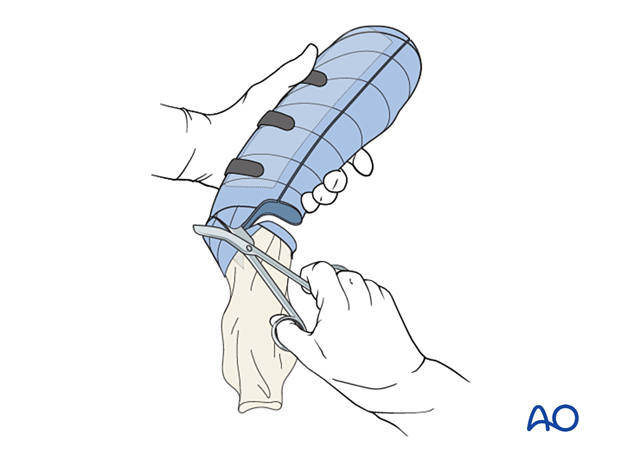
Cut through the cast beginning proximally at the lateral aspect of the arm.
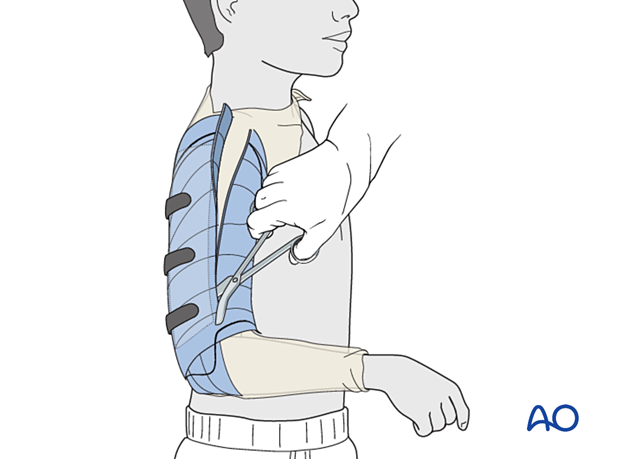
Open the brace and remove it.
Trim the brace to the desired shape.
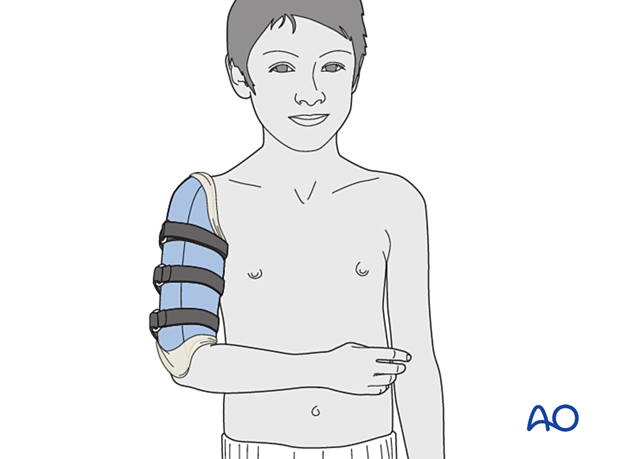
Prepare a new tube bandage and place over the arm before applying the brace.
Attach the Velcro strips (with hooks); compress the brace slightly and provisionally close with the strips.
Apply tension to the tube bandage, loosen the Velcro strips, place the brace in the final position and refasten the strips.
Ensure free flexion and extension of the elbow. Ensure free movement of the olecranon fossa.
Fold the tube bandage over the brace to provide protection.
Check that the brace is not too tight, check edges are not pinching the skin, and confirm that the radial pulse is palpable.
4. Cast application
Introduction
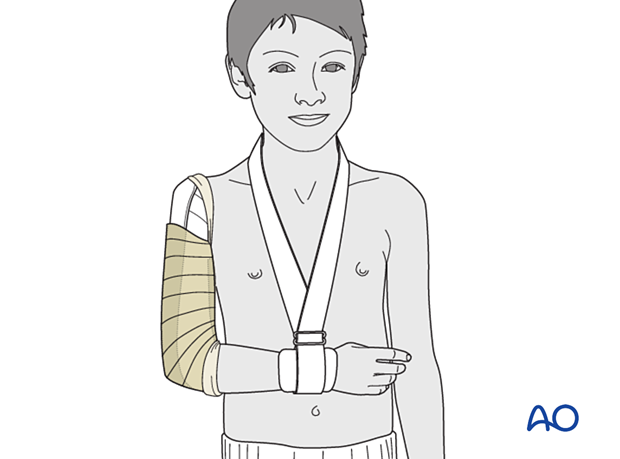
The aim of a hanging cast, in combination with a collar and cuff, is to immobilize the fracture and encourage reduction with traction.
The proximal end of the cast often ends at or slightly proximal to the level of the fracture and does not support the fracture.
AO Video
Long arm cast - Plaster of ParisIndications:
- Fracture of the radius
- Fracture of the ulna
- Fracture of the elbow
- Epicondylitis
Material
- Tubular bandage (stockinette) of appropriate size
- Cast padding
- Felt
- Casting material: plaster of Paris
- Water
The water temperature should ideally be between 22° and 25° C.
Application of cast
Hold the elbow in 90° flexion and the forearm in neutral rotation.
A tubular bandage may also be applied to the arm beneath the padding.
Wrap cast padding around the upper arm, elbow, and forearm, as far as the wrist crease.
Make sure that the epicondyles of the humerus and the antecubital area are well padded.
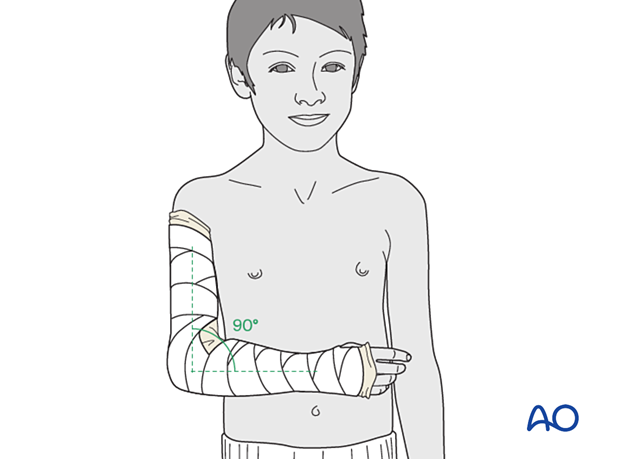
Apply a full plaster cast around the arm and forearm.
Fold the proximal and distal ends of the tubular bandage over the cast and cover the cast with an additional single layer of plaster.
Ensure that the edges of the cast are well-padded and smooth, to avoid abrasion during the period of plaster immobilization.
Consider splitting the cast to accommodate swelling in the initial period following injury
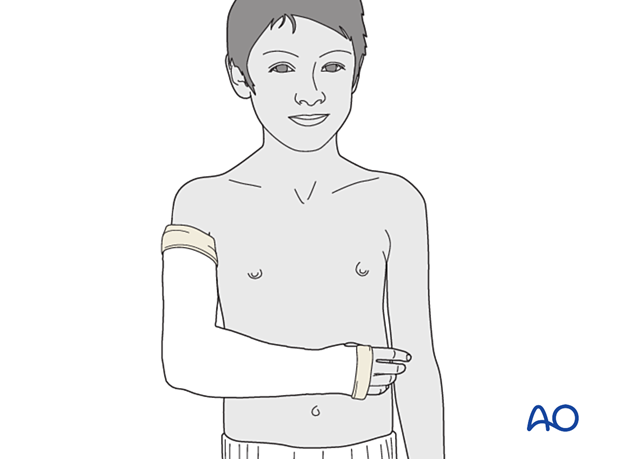
Support with a collar and cuff
The injured arm and cast are supported with a collar and cuff.
5. Aftercare following immobilization
Duration of immobilization
Humeral shaft fractures require 3–6 weeks of immobilization for adequate healing, depending on the age of the patient and fracture morphology.
Immobilization may be discontinued as symptoms improve.
Follow-up
AP and lateral x-rays should be taken to assess fracture position at intervals decided by the fracture configuration and age of patient.
Recovery of motion
Recovery of movement is usually rapid and rarely requires physiotherapy.
Resumption of unrestricted physical activity is a matter of judgment by the treating surgeon.
Remodeling
Remodeling is less predictable in older children and residual angulation may result in visible deformity.













