Anatomy of the forearm shaft
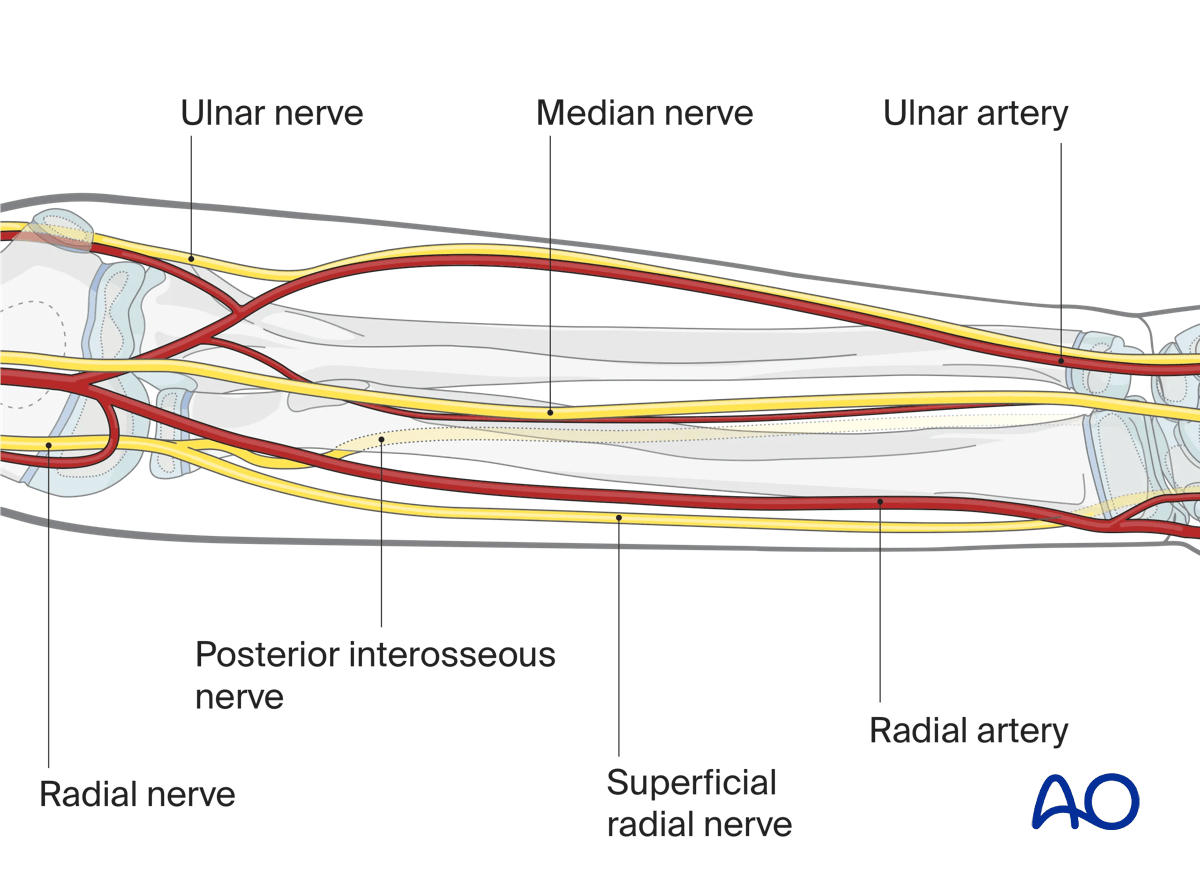
1. Neurovascular structures
The forearm anatomy is complex due to the presence of three major neurovascular bundles.
In particular:
- Radial nerve with its two branches (posterior interosseous nerve and superficial radial nerve)
- Brachial artery
- Radial artery
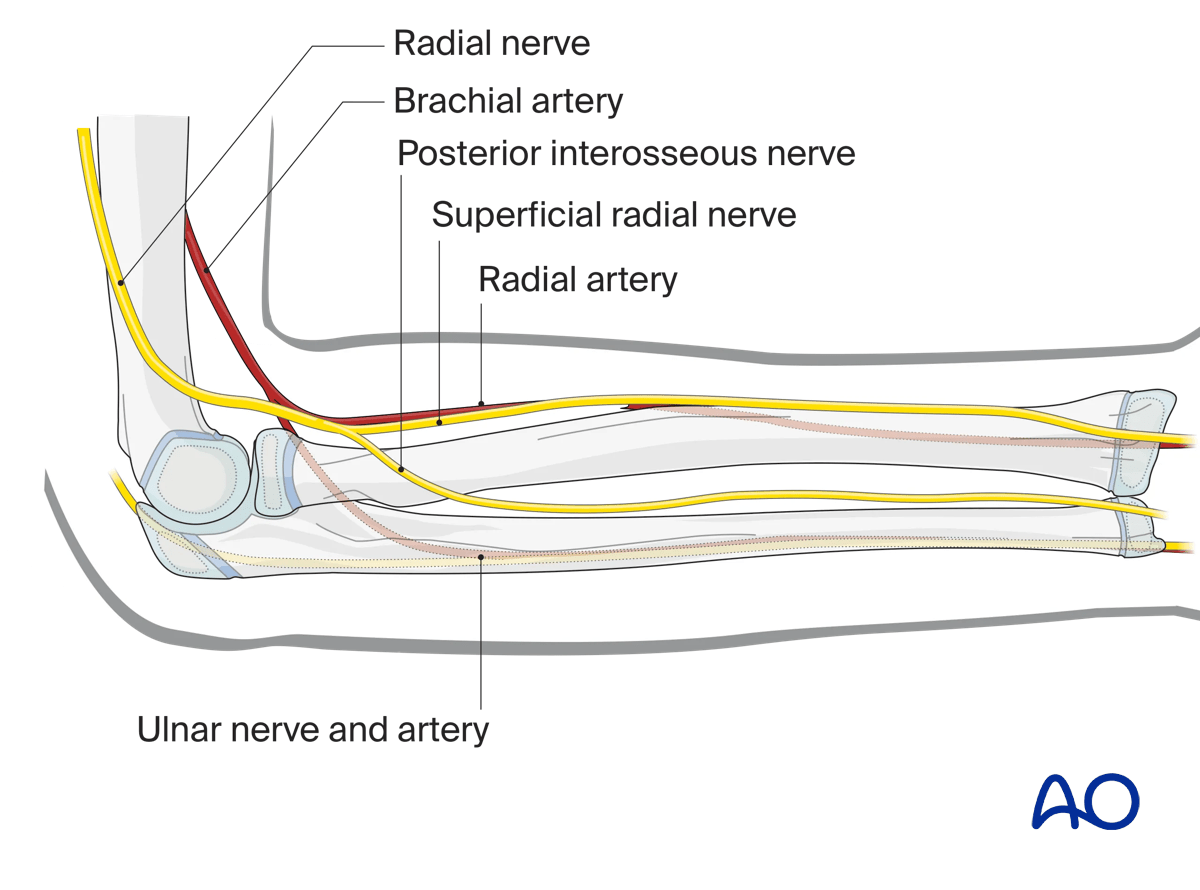
- Median nerve
- Ulnar nerve
- Ulnar artery
Except for the posterior interosseous nerve, all previously mentioned structures run in the flexor compartment.
Note: the cephalic vein runs parallel to the superficial radial nerve in the distal part of the forearm.
Pitfall: The more proximal the approach, the greater the risk of damage to important structures.
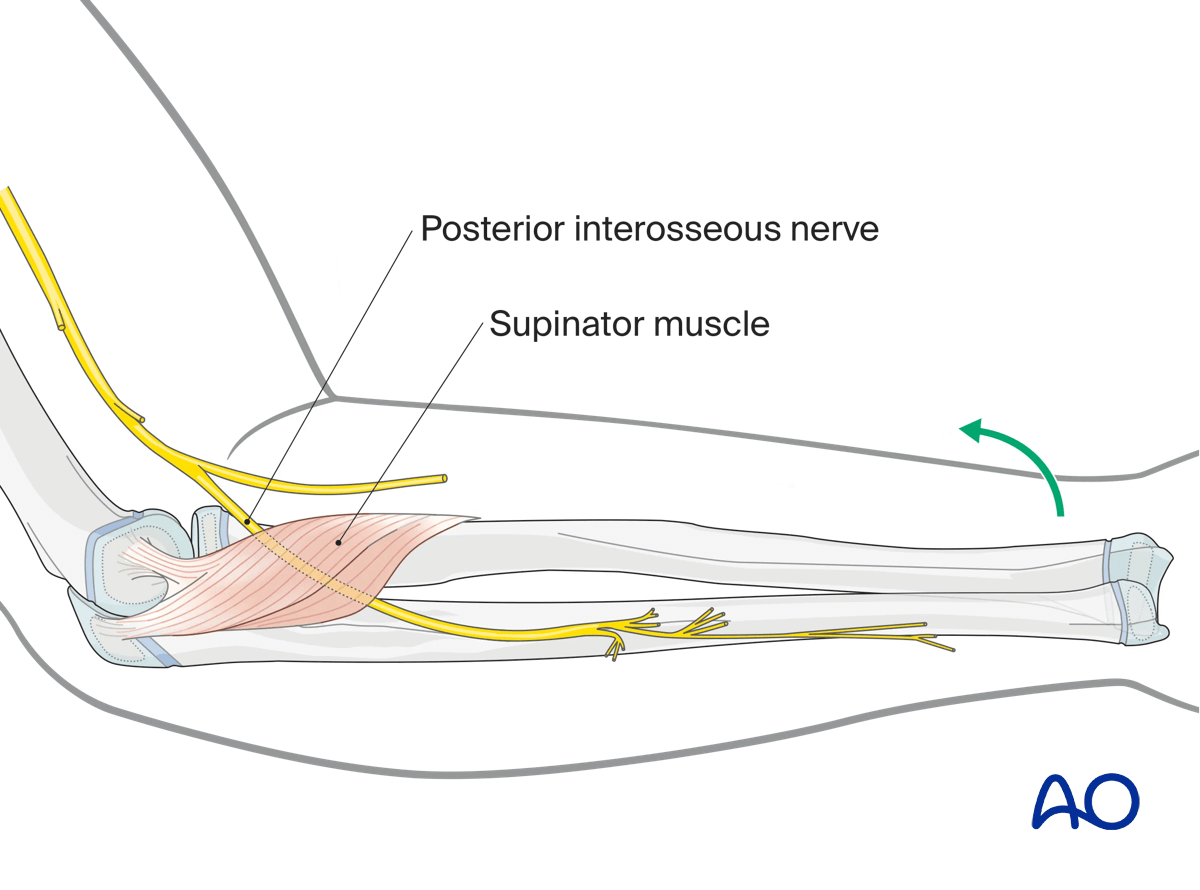
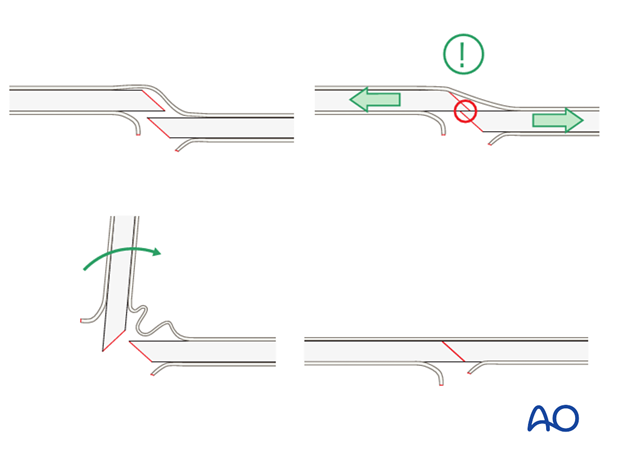
2. Posterior interosseous nerve
The posterior interosseous nerve (PIN, also known as the deep branch of the radial nerve) is at particular risk from open and percutaneous approaches to the proximal radius.
The nerve crosses the proximal radius approximately three patient finger breadths distally to the flare of the radial neck.
Mark this position using the child’s fingers as a reference.
Pronate the arm and thereby move the PIN anteriorly.
Minimize the risk to the nerve by placing K-wires from a lateral or a posterior direction.
Never place percutaneous K-wires from an anterior direction into the proximal radius.
3. Forearm axis and rotation
The radius, ulna, elbow joint, and proximal and distal radial/ulnar joints function together to provide nearly 180° of pronation and supination. The radius can be thought of rotating around a fixed ulna.
Clinical implications:
- Both bone fractures are common.
- Monteggia lesions are common.
- Other single bone fractures are rare.
- Accurate reduction and stability is required to maintain forearm function.
- Anatomic or near anatomic reduction is necessary if little or no growth remains.
- Younger children with tough periosteum can be successfully treated with closed reduction and casting.
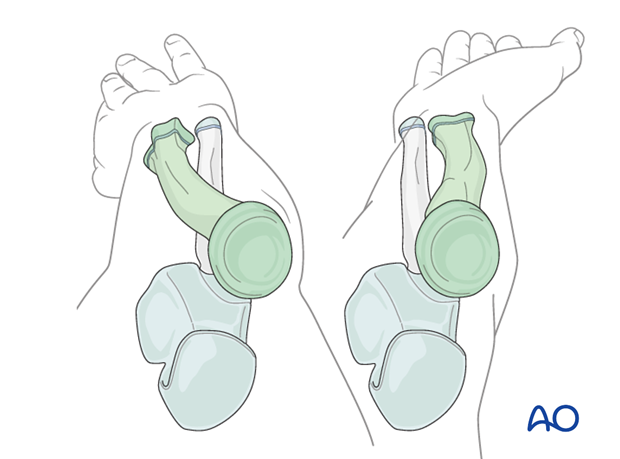
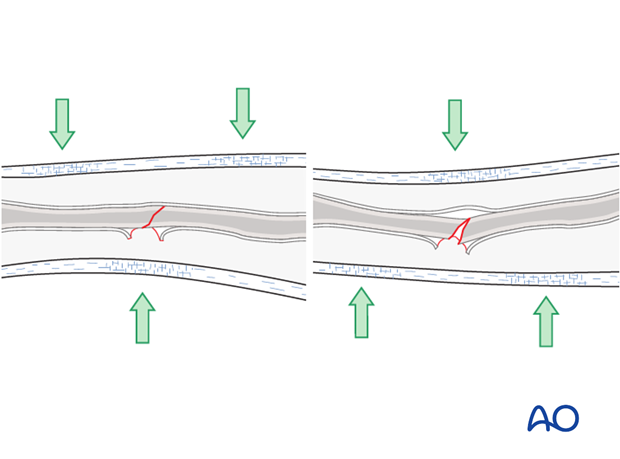
4. Periosteum as a factor in reduction and stability
Children’s periosteum is a thick, tough tissue and is often intact on the concave (compression) side of a fracture.
The stability of the periosteum is an advantage when performing gentle reduction maneuvers.
If the periosteum needs to be loosened to allow gentle reduction, it may be necessary to exaggerate the fracture deformity.
Thick periosteum confers extra stability with three-point molding as the concave periosteum acts as a tension band.
5. Developmental anatomy
The proximal radius ossification center is the second to appear around the elbow at the age of 3-5 years.
This fuses close to maturity at about 12 years in girls and 14 in boys.
The olecranon ossification center appears at nine years and fuses gradually between 11 to 13 years in girls and 13 to 15 years in boys.
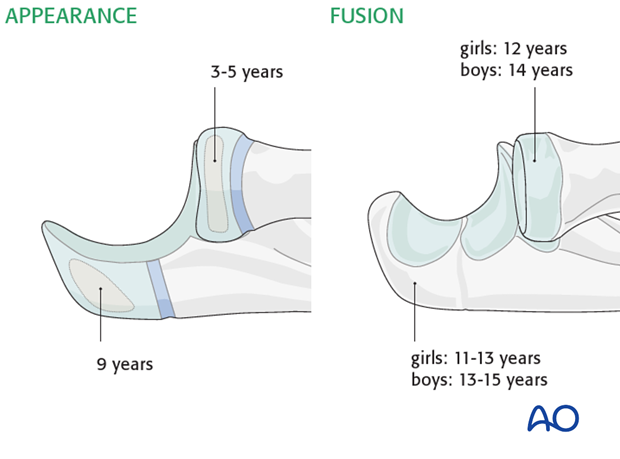
The distal radial ossification center typically appears by 1-2 years and fuses at 14 in girls and 16 in boys.
The distal ulnar ossification center appears between 3 to 5 years and fuses at 14 years in girls and 16 in boys.

The majority of longitudinal growth in the forearm is from the distal radius and ulna.
Clinical implications:
- Growth related modeling of distal metaphyseal fractures is significant.
- Modeling cannot be relied on to realign malunions of shaft or proximal radius and ulna.













