Radius, bowing: ESIN
1. Instruments and implants
Instrument set for ESIN
- 1.5-2.5 and occasionally 3.0 mm elastic nails
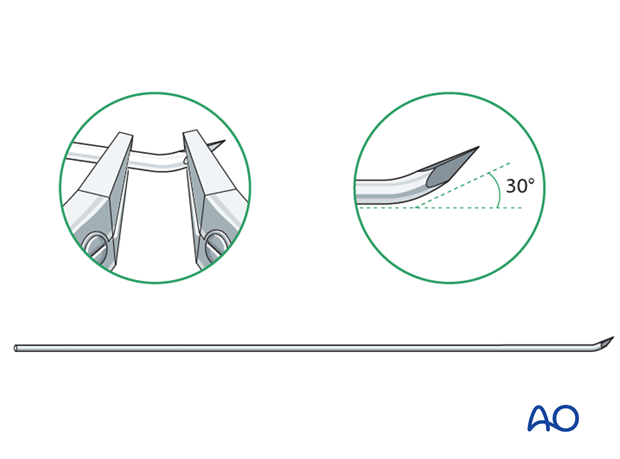
- Alternatively: 30 cm long, 1.6-2.5 mm K-wires with the tip bent
- Awl or drill
- Inserter
- Nail cutter
- Small hammer
- Optional: end caps
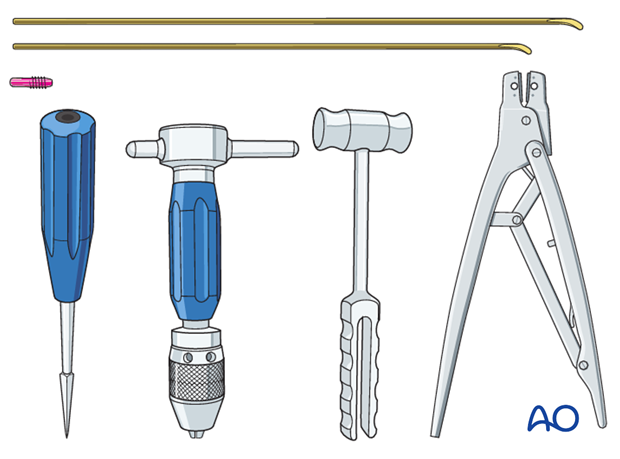
The end cutter is useful to avoid sharp ends and soft-tissue irritation.
Use of K-wires
Ring fixator wires may be used.
Bend the tip by approximately 30° to provide a gliding aid.
Nail diameter
For optimal reduction and intramedullary three-point fixation, the nail diameter should be between 60% and 70% of the medullary canal.
2. Technique
Preliminary reduction
Preliminary reduction is not useful as deformity often recurs following manipulation.
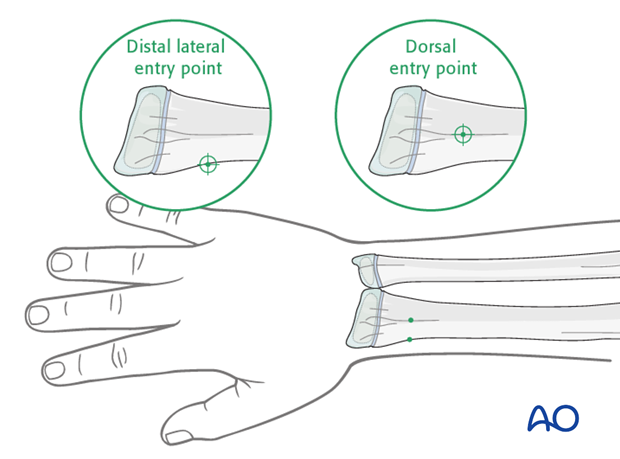
Entry points
The distal lateral entry point is in common use and shown in this procedure.
Insertion through Lister’s tubercle (dorsal entry point) is also well established and offers more versatile nail manipulation and is an alternative for distal 1/3 fractures of the radius.
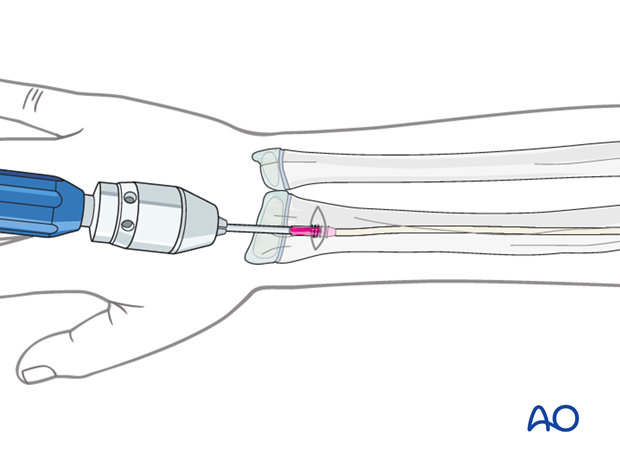
Opening the canal
Use small scissors or a surgical clip and small retractors to dissect to the bone under direct vision.
Note: Avoid injury to the superficial radial nerve and the cephalic vein.
Place the awl or drill directly onto the bone and perforate the near cortex, under direct vision, perpendicular to the bone.
Do not hammer the awl to avoid perforation of the far cortex.
When the medullary canal is reached, lower the awl or drill 45° to the shaft axis and advance it with oscillating movements to produce an oblique canal.
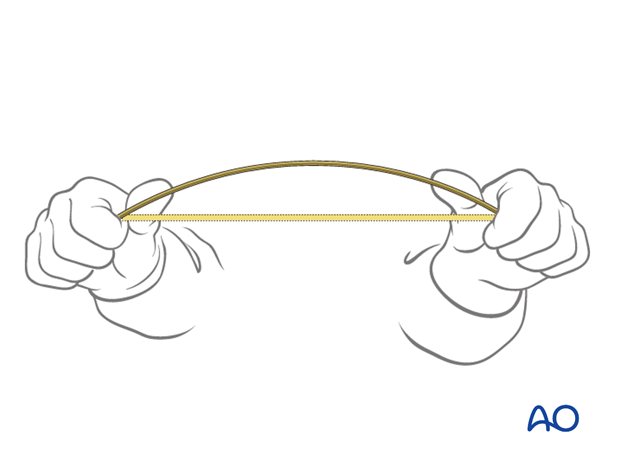
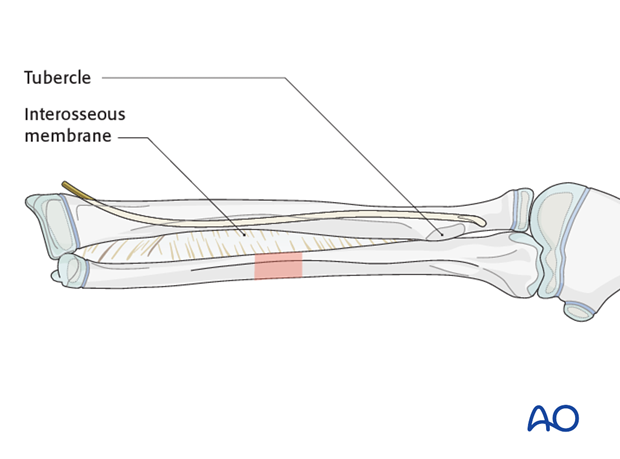
Nail precontouring
Precontour the nail to reproduce the geometry of the bowing deformity.
Nail insertion
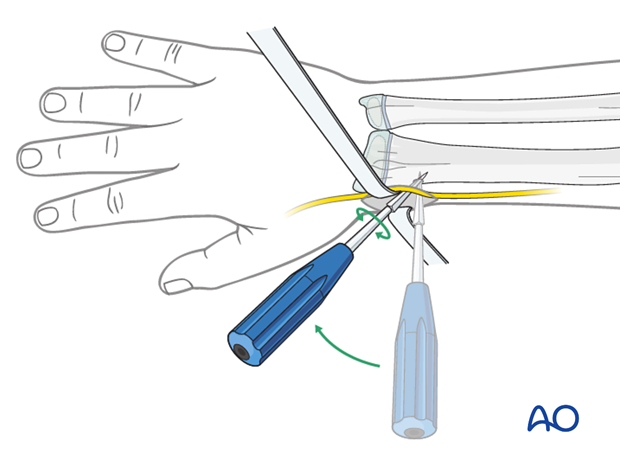
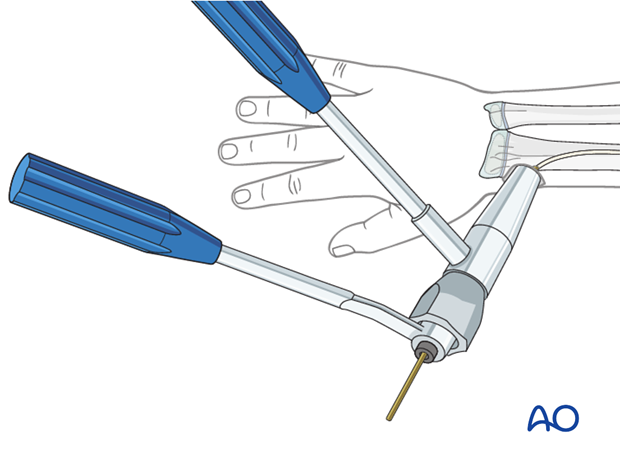
Fix the nail into the inserter and pass it into the canal.
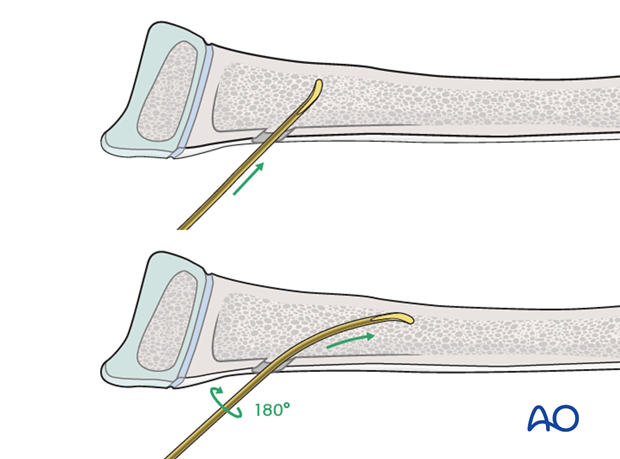
Pearl: insertion of nail tip perpendicular to shaft
Insert the nail with the tip perpendicular to the shaft axis until the far cortex is felt. Rotate the nail 180° and advance it using the curved side of the tip as a gliding aid.
If the tip is stuck in the far cortex and cannot be advanced, remove the nail and bend the tip to give a slightly more pronounced curvature.
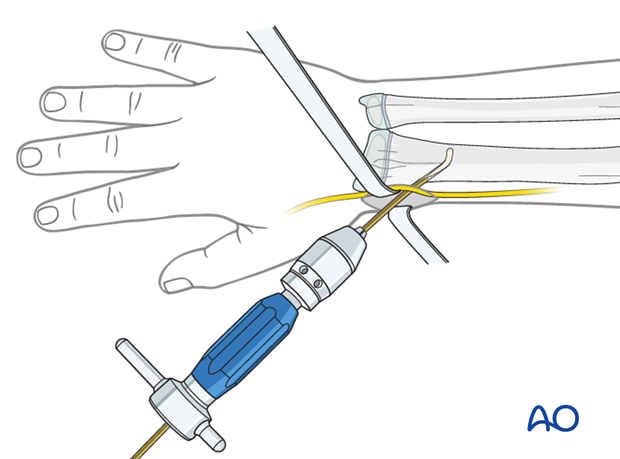
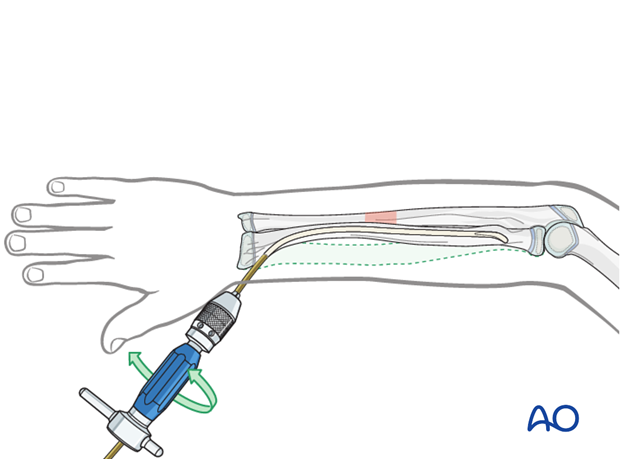
Advancing the nail
Advance the nail into the strong metaphyseal bone at the radial tubercle with an oscillating maneuver.
The precontouring and bowing should be in the same plane.
Pearl: A short working length (3-5 cm) between the entry point and the inserter improves control of the nail during insertion.
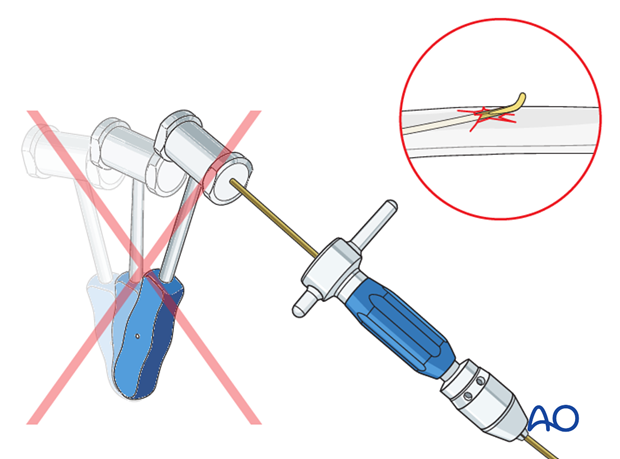
Pitfall: iatrogenic fracture
In young children, the nail tip may become stuck because of the narrow medullary canal.
Do not use a hammer if the nail is stuck as this risks iatrogenic fracture.
Withdraw by 2 cm, rotate the nail to free the tip and continue advancing.
Pearl: estimation of nail length
If an image intensifier is not available, estimate the optimum nail length with a second identical nail placed parallel to the initial nail.

Reduction
Rotate the nail 180° to counteract the deformity and re-anchor the tip in the cortex.
Full realignment of deformity may take several days.
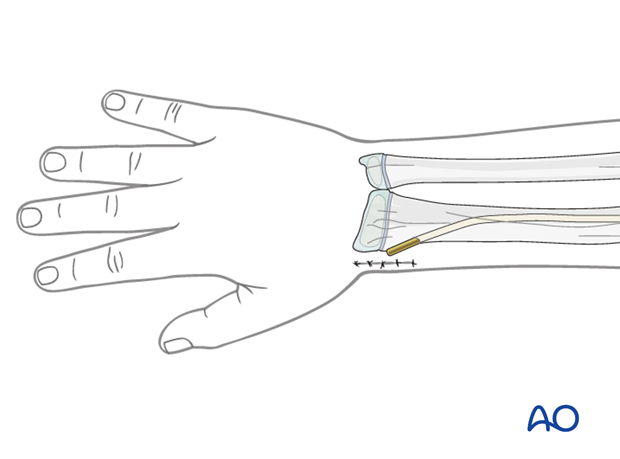
Cutting the nail and wound closure
When using the lateral entry point, cut the nail near the bone.
If a dedicated nail cutter is not available, cut the nail slightly shorter as the end will be sharper and this prevents skin perforation.
Gently withdraw the nail by 1 cm, cut the nail outside the skin and reinsert to the original position with an impactor.
Ensure that the nail tip does not irritate the superficial radial nerve.
When using the dorsal entry point, the nail should be left long or protected with small end cap to prevent rupture of the extensor pollicis longus.
Close the subcutaneous tissue and skin in a standard manner.
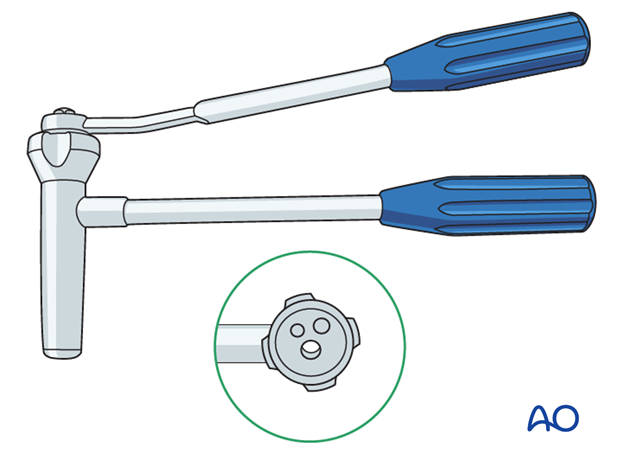
3. Option: end caps
End caps may be useful for:
- Stabilization of length unstable fractures
- Protection of soft tissues (eg EPL)
The nail should finally be advanced using the beveled impactor.
A small end cap can be inserted over the nail using the inserter.