Closed reduction; K-wire fixation
1. General considerations
Introduction
Distal tibial fractures often require temporary internal fixation that crosses the physis to produce adequate stability.
The following should be considered to minimize secondary damage to the physis:
- Manipulation of the fracture must be gentle
- Multiple passes across the physis with a K-wire should be avoided
- Select smooth, appropriately sized K-wires
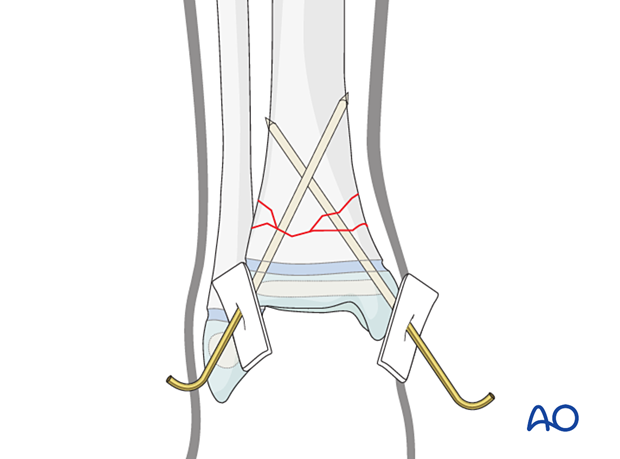
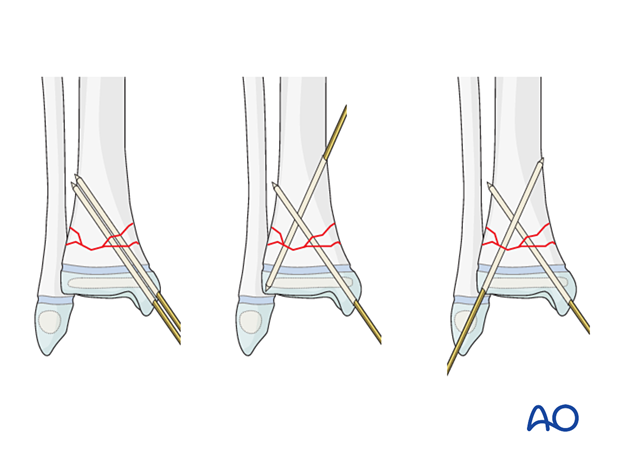
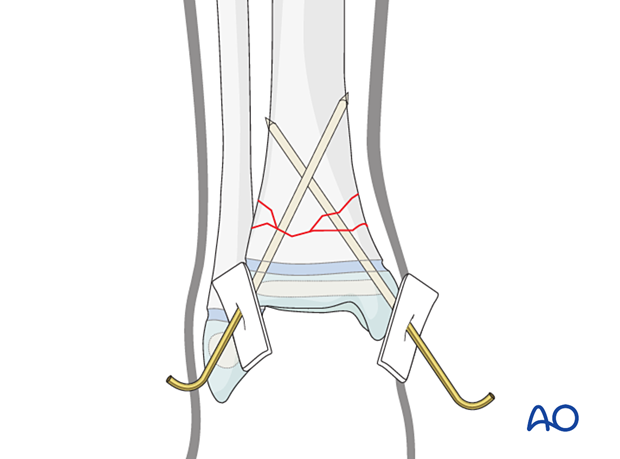
Stabilization is usually performed with two K-wires. There are three commonly used constructs:
- Two parallel or divergent K-wires inserted from the medial malleolus into the lateral metaphysis
- One K-wire from the medial malleolus and one from the medial metaphysis to the lateral epiphysis
- One K-wire from the medial malleolus and one from the lateral tibial epiphysis
Associated fibular fracture
A fibular fracture often reduces with reduction and fixation of the tibial fracture and does not require separate consideration.
If the alignment and stability of the fibular fracture are unsatisfactory after fixation of the tibial fracture, surgical treatment of the fibular fracture is also required.
If the distal tibial fracture is highly comminuted, fixation of the fibular fracture may add to overall stability.
Treatment goals
The goal is to maintain acceptable reduction and stability until healing, without additional damage to the physis.
Closed vs open reduction
If initial closed reduction is unsuccessful, this is usually due to periosteum entrapped in the fracture on the side that has failed in tension.
2. Instruments and implants
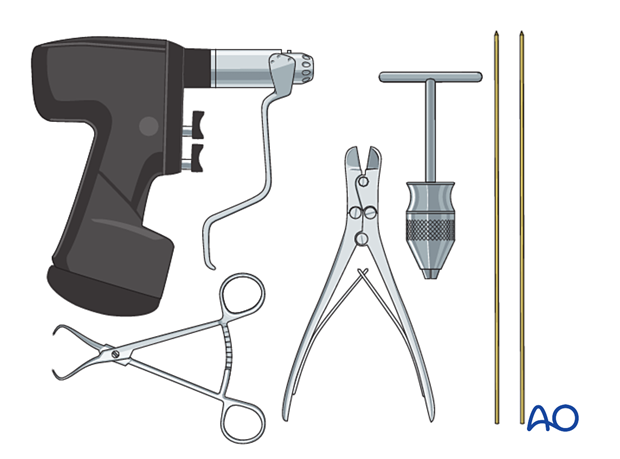
The following equipment is used:
- K-wires of appropriate sizes
- Drill or a T-handle for manual insertion
- Wire cutting instruments
- Standard orthopedic instrument set
3. Patient preparation
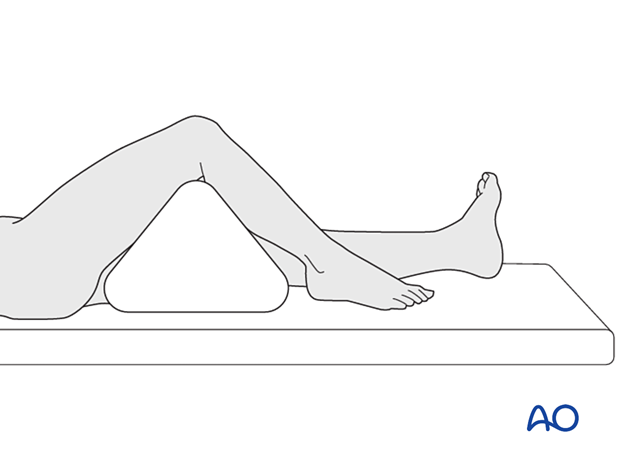
Place the patient in a supine position on a radiolucent table.
Put a bolster or triangle underneath the knee.
4. Reduction
Reduction of distal tibial and fibular fractures may be difficult. Support from at least one assistant, providing countertraction and stabilizing the proximal leg, may be helpful.
With the knee flexed and stabilized, apply longitudinal traction through the foot.
Correct translation and angulation of the fracture and confirm reduction clinically and with an image intensifier if available.
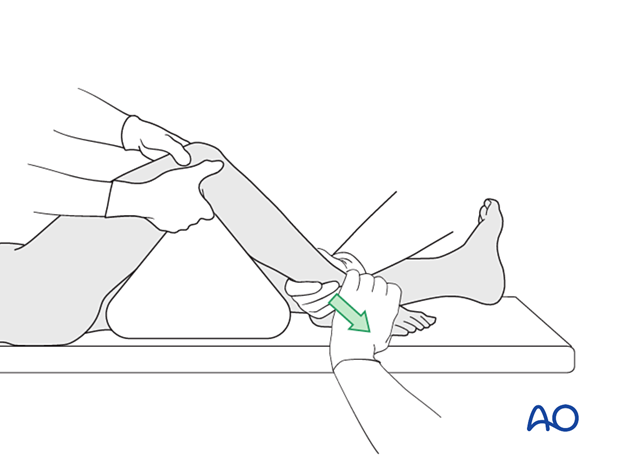
The position of the foot and ankle is important in some metaphyseal fractures.
Placing the foot and ankle in a neutral position may produce an apex posterior deformity in unstable fractures.

5. Fixation
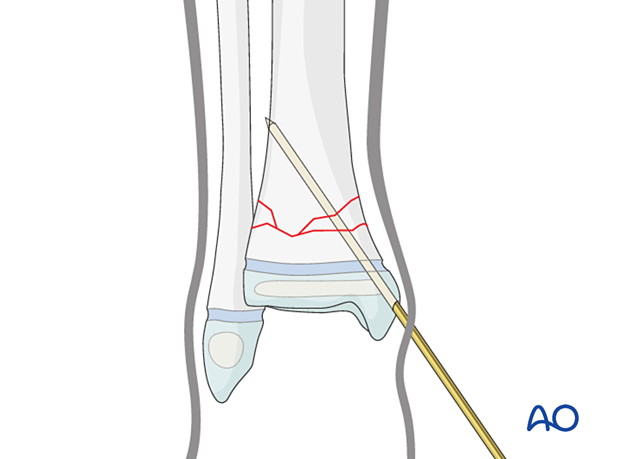
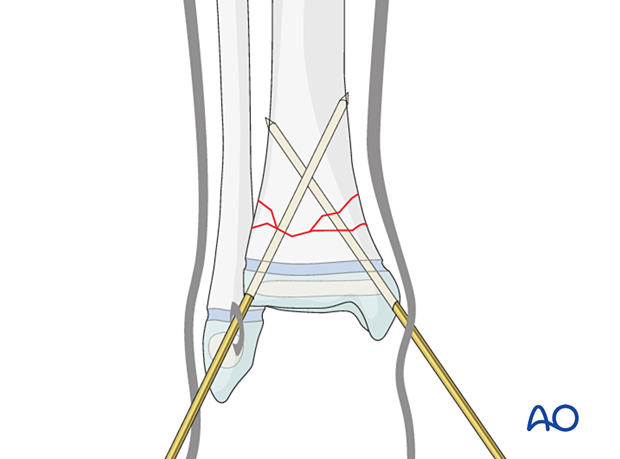
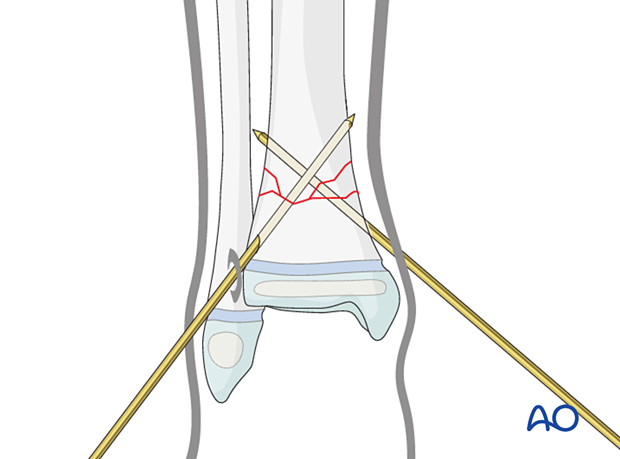
Insert the initial K-wire from the medial malleolus.
Advance the K-wire across the physis after confirming a trajectory that will gain sufficient metaphyseal engagement on AP and lateral views.
Engage the K-wire in the far cortex.
A second parallel or divergent medial K-wire may be inserted.
Inserting a K-wire too far posteriorly may damage the posterior tibial neurovascular bundle.
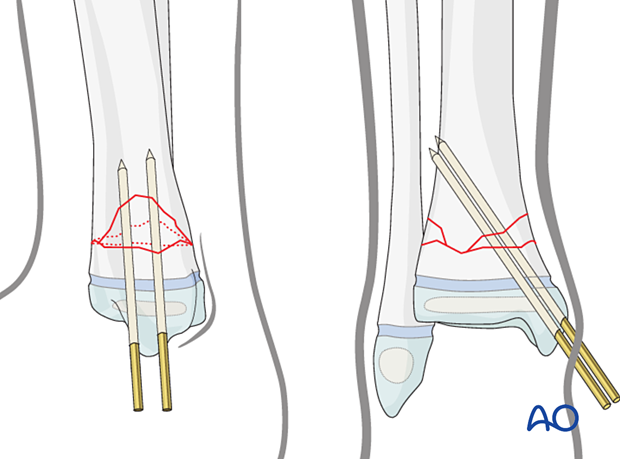
On the lateral side, the insertion point for the second K-wire is just anterior to the fibula.
A small incision with blunt dissection is recommended to avoid damage to the superficial branch of the peroneal nerve.
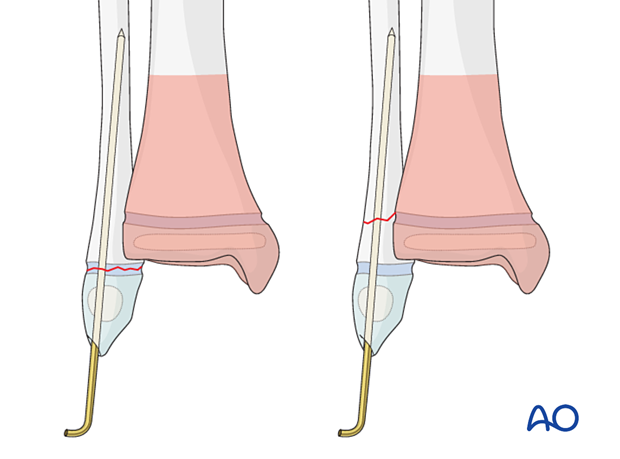
A second medial K-wire may be inserted in an antegrade direction.
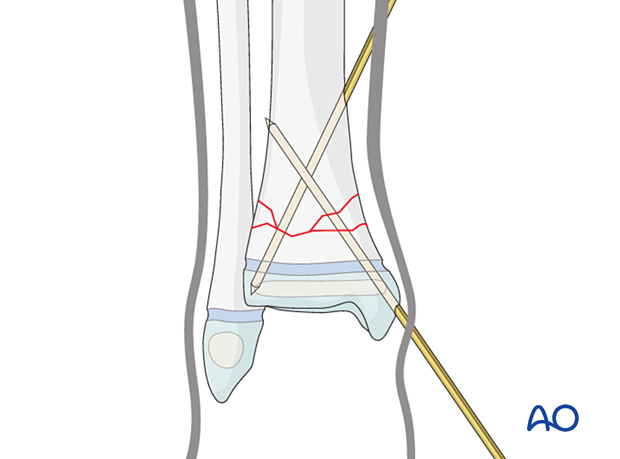
Option
If the distal metaphyseal fragment is large enough, placing both K-wires entirely within the metaphysis may be possible. This has the advantage of avoiding the joint and minimizing the risk of physeal disturbance.
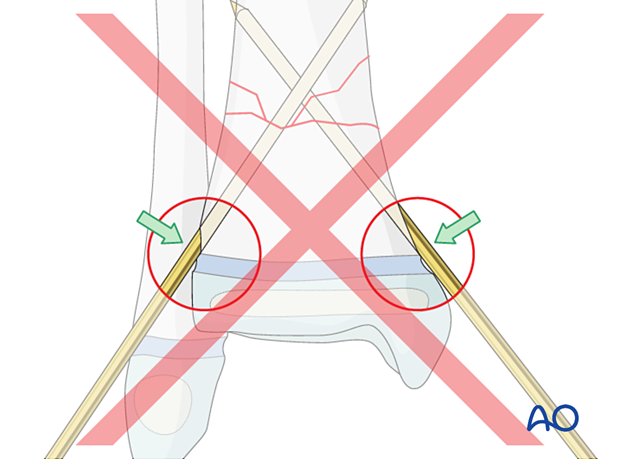
Avoid inserting the K-wire at the edge of the physis as this may damage the perichondrial ring by direct trauma or indirect pressure.
K-wire cutting and dressing
Bend the K-wires approximately 1 cm from the skin to allow for swelling.
Cut the K-wires and apply a dressing to protect the skin.
Release tethered skin around the K-wire by extending the incision.
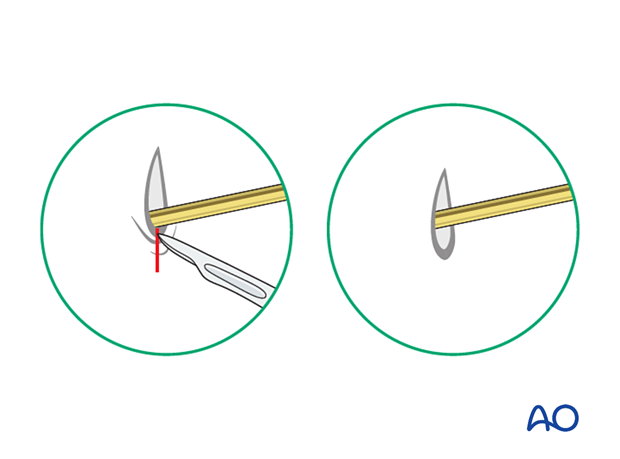
Alternatively, the K-wire may be placed under the skin with the bent end on the surface of the bone.
6. Fibular fracture management
Most fibular fractures do not require treatment. Indications for fixation include:
- Augmentation of the stability of tibial fracture fixation
- Significant displacement of the fibular fracture
The type of fracture pattern dictates the fixation of the fibular fracture.
K-wires are inserted in a standard manner. Multiple passes of the K-wire through the physis should be avoided.
In an unstable tibial eversion fracture, an associated diaphyseal fibular fracture may require plate fixation.
7. Final assessment
Recheck the fracture alignment and implant position clinically and with an image intensifier before anesthesia is reversed.
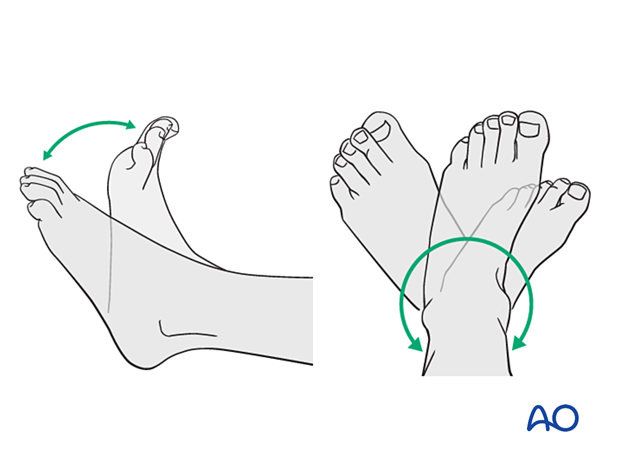
Confirm stability of the fixation by moving the ankle through a range of dorsi/plantar flexion.
8. Immobilization
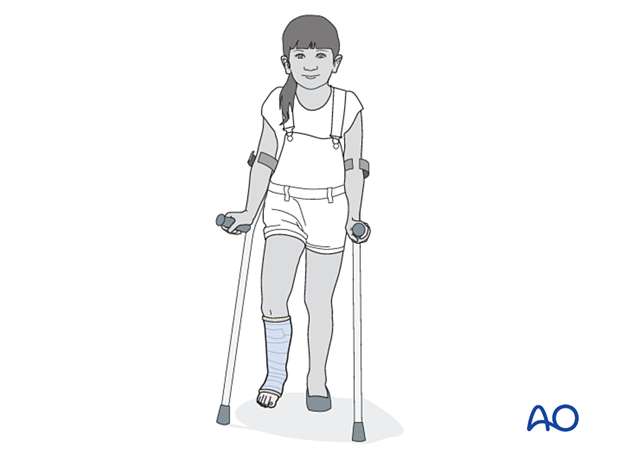
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight-bearing.
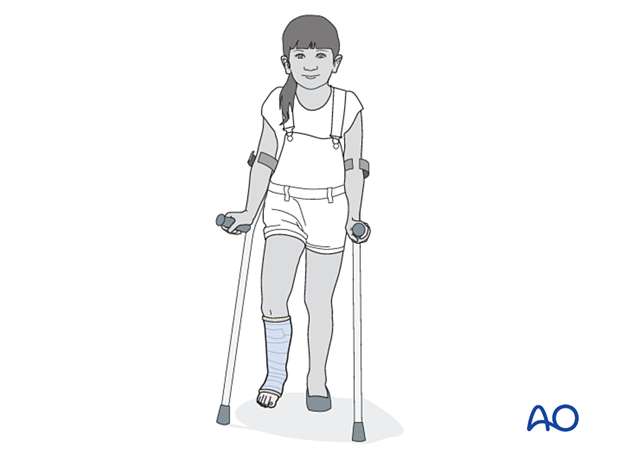
9. Aftercare
Immediate postoperative care
Non-weight-bearing or touch weight-bearing is encouraged for unstable injuries.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast and K-wire removal
Distal tibial and fibular fractures heal rapidly. Cast and K-wires are typically removed 3–6 weeks after injury, depending on the age and weight of the patient.
Mobilization
Once K-wires and cast are removed, gradual weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.