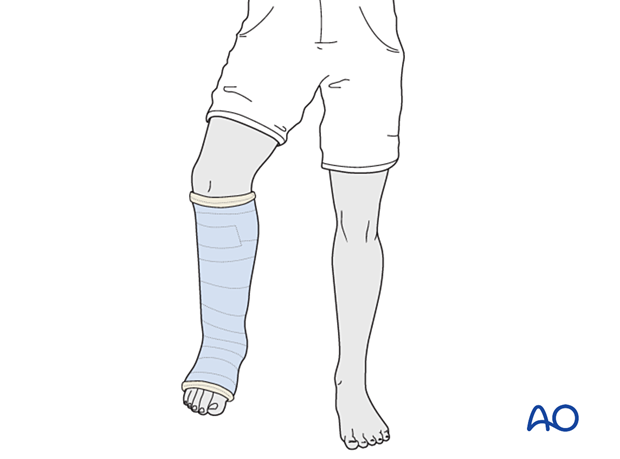
Closed reduction; short leg cast
1. General considerations
Indications
A below-knee cast or short leg splint provides sufficient stability for most stable metaphyseal distal tibial and fibular injuries and allows mobilization of the knee.
It can be used for potentially unstable fractures, provided they are kept under close surveillance.
It can also be used following closed reduction or surgical fixation in the early postoperative period.
Complications
- Pressure sores
- Skin irritation
- Compartment syndrome
- Thermal burns (avoid using hot water)
Splinting
If severe swelling prevents application of a circumferential cast, a temporary splint may be applied as an alternative.
With the knee flexed, apply padding around the leg and slabs of casting material posteriorly, covering half of the circumference.
Secure the splint with an elastic bandage.
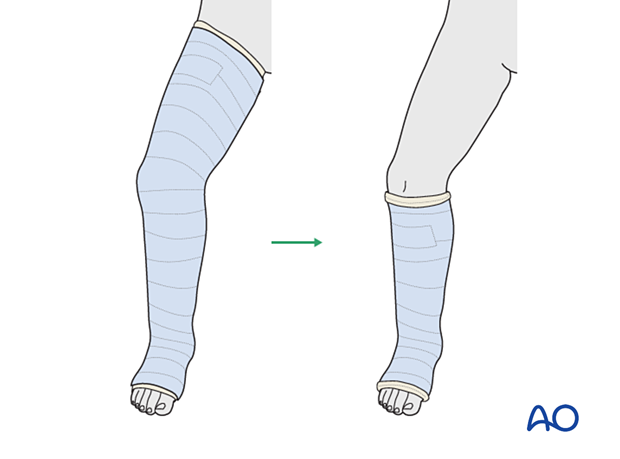
Option: initial long leg cast
A long leg cast may be required to provide more stability and prevent the child from weight-bearing on the injured leg.
This is typically changed to a below-knee walking cast when the fracture is sufficiently stable.
Managing reduction
Closed reduction of distal tibial and fibular fractures may be difficult. Support from at least one assistant, providing countertraction and stabilizing the proximal leg, may be helpful.
2. Patient preparation
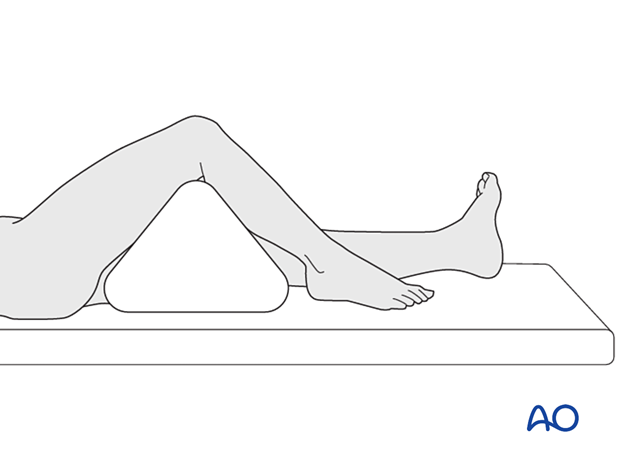
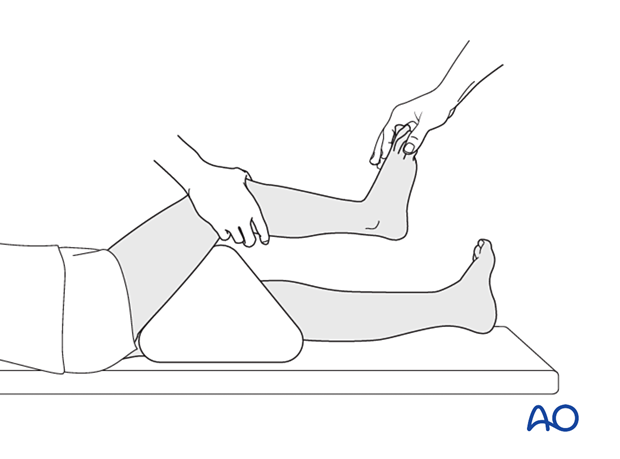
Place the patient in a supine position on a radiolucent table.
Put a bolster or triangle underneath the knee.
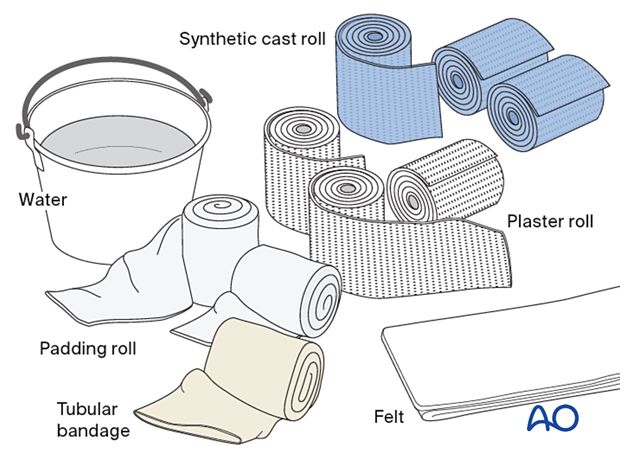
3. Material
- Tubular bandage (stockinette) of appropriate size
- Cast padding
- Felt
- Casting material: synthetic, plaster of Paris, or a combination of both
- Water
The water temperature should ideally be between 22° and 25° C.
4. Closed reduction
With the knee flexed and stabilized, apply longitudinal traction through the foot.
Correct translation and angulation, and confirm reduction clinically and with an image intensifier if available.

5. Casting
Patient and leg positioning
An assistant supports the knee.
Dressing
The cast extends from just below the knee to the base of the toes.
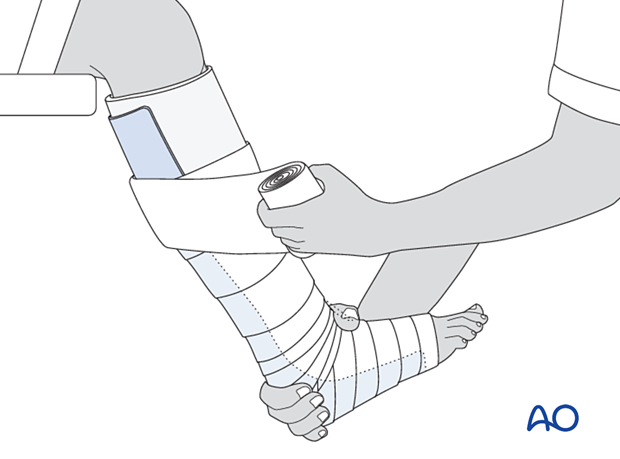
Apply a tubular bandage and cut it slightly longer than the length of the final cast.
The assistant holds the toes, not the stockinette, with the ankle in a neutral position.
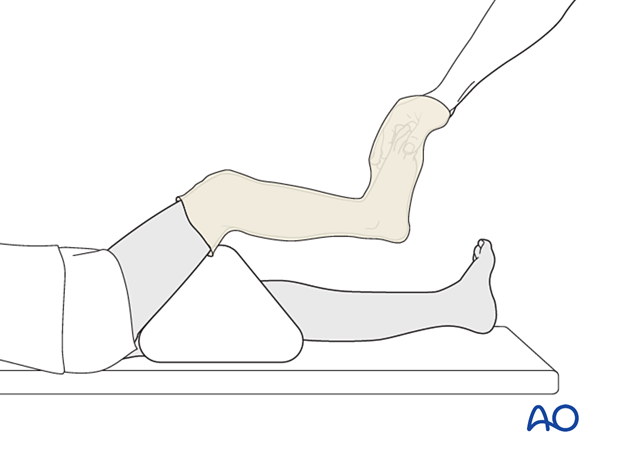
Padding
Consider adding thick felt over the padding at the malleoli, tibial crest, heel, and the free edges of the cast.
Apply cast padding without creases, overlapping each layer by 50%.
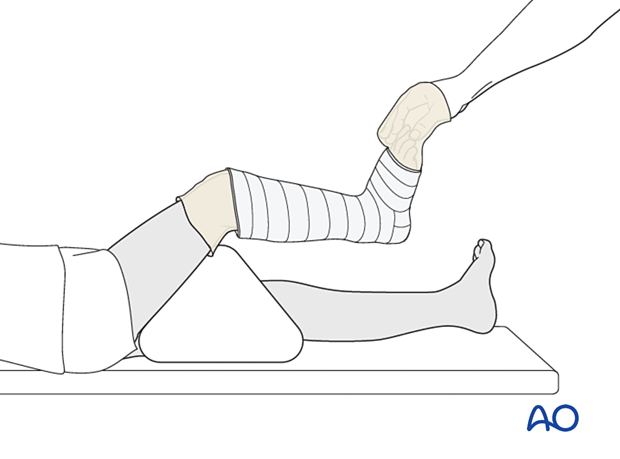
Cast application
Apply the first layer of cast material and overlap each layer by 50%.
Avoid sharp edges at the ends of the cast. Make sure the upper end of the cast is well below the popliteal fossa.
Apply further layers of cast material to produce sufficient stability.
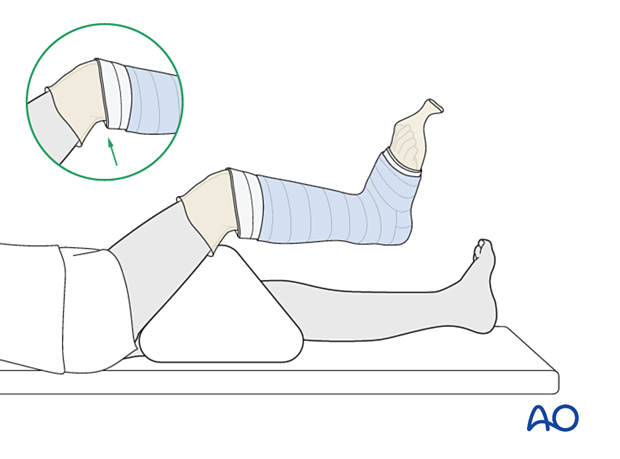
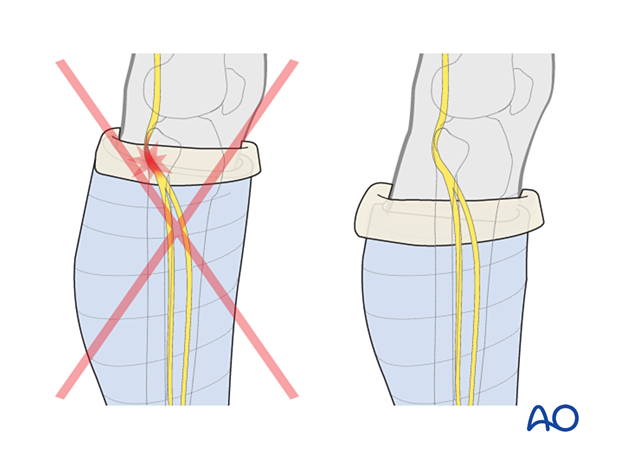
Avoid pressure over the fibular head and neck by adding sufficient padding and shortening the cast to prevent injury to the peroneal nerve.
Fold the tubular bandage and padding over the edges of the cast before applying the final layer of casting material.
6. Final assessment
After cast application, check the fracture configuration with x-rays in both planes.
7. Aftercare
Instructions to parents/carers
Parents/carers should understand the following precautions and instructions:
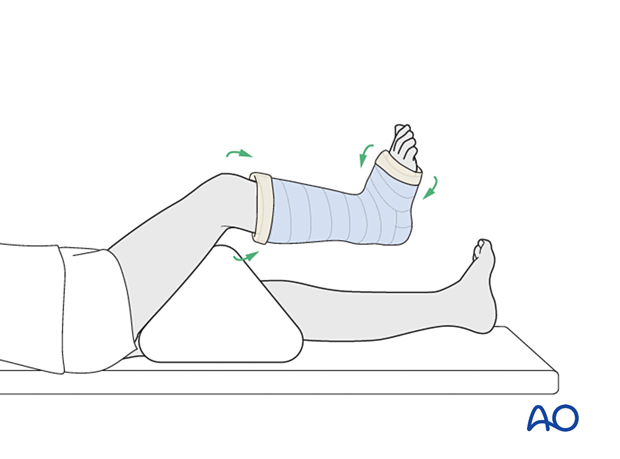
- Elevate the foot to the level of the heart to avoid swelling
- Check daily for swelling, discoloration, and impaired toe circulation (any of which should be reported urgently)
- Immediately report signs suggesting skin irritation ulceration, and cast soiling
- Make sure the cast padding remains dry and avoid inserting anything between the cast and skin
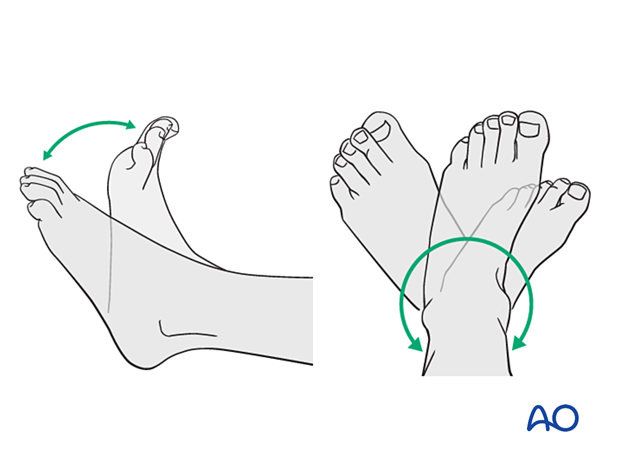
- Encourage active toe movement
Immediate postinjury care
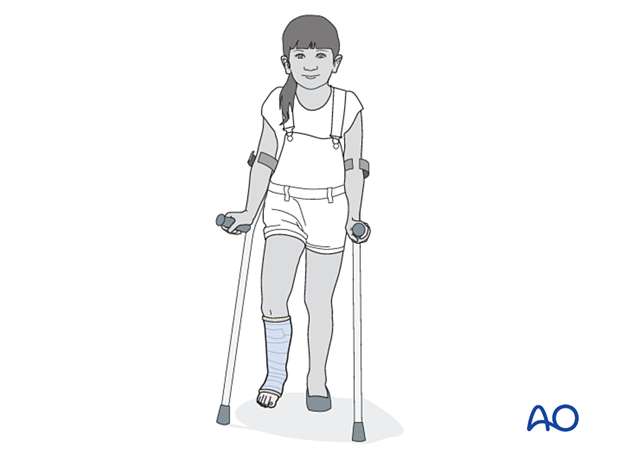
Non-weight-bearing or touch weight-bearing is encouraged for unstable injuries.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Routine pain medication is prescribed for 3–5 days after injury if required.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after injury to confirm fracture stability.
Cast removal
Physeal and metaphyseal fractures heal rapidly, and the cast is typically removed 3–6 weeks after injury.
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be necessary in some cases but is not mandatory.
Activities that involve running and jumping are not recommended until full recovery of local symptoms.
Follow-up for growth disturbance
All patients with distal tibial physeal fractures should have continued clinical and radiological follow-up to identify signs of growth disturbance.
Compare alignment and length clinically with the uninjured leg.
A Harris growth arrest line, parallel to the physis, is radiological evidence of continuation of normal growth.
Recommended reading:
- Nguyen JC, Markhardt BK, Merrow AC, et al. Imaging of Pediatric Growth Plate Disturbances. Radiographics. 2017 Oct;37(6):1791–1812.













