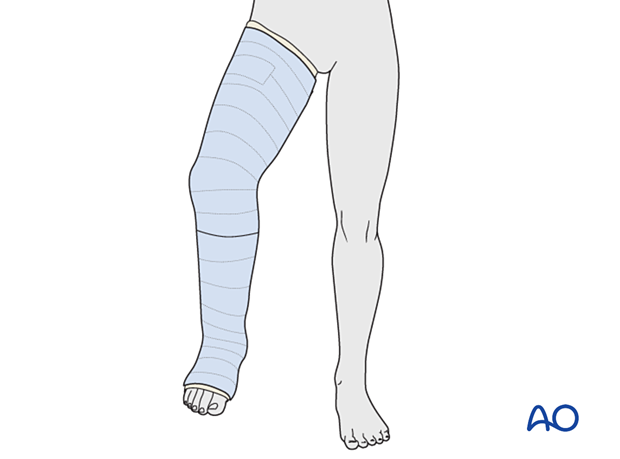
Closed reduction; long leg cast
1. General considerations
Introduction
A long leg cast may be necessary for unstable injuries of the distal tibia and fibula.
The cast may be applied in two stages, initially over the leg and foot and then extending to the upper thigh with the knee flexed.
This initially controls the ankle and facilitates casting of the thigh with the knee in the correct position.
Complications
- Pressure sores
- Skin irritation
- Loss of reduction
- Compartment syndrome
- Thermal burns (avoid using hot water)
Splinting
If severe swelling prevents application of a circumferential cast, a temporary splint may be applied as an alternative.
With the knee flexed, apply padding around the leg and slabs of casting material posteriorly, covering half of the circumference.
Secure the splint with an elastic bandage.
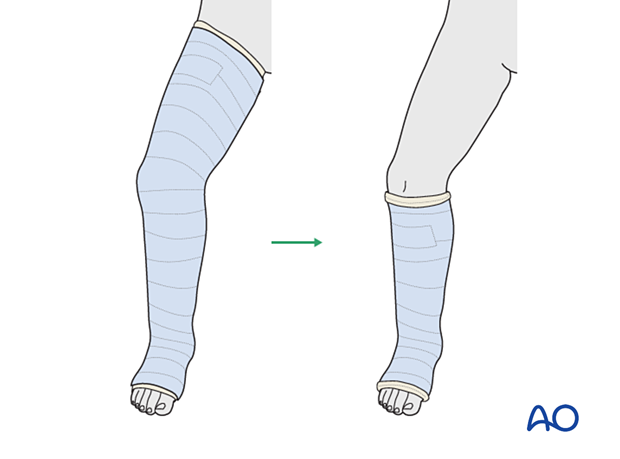
Option: conversion to a short leg cast
This is typically changed to a below-knee walking cast when the fracture is sufficiently stable.
Managing reduction
Closed reduction of distal tibial and fibular fractures may be difficult. Support from at least one assistant, providing countertraction and stabilizing the proximal leg, may be helpful.
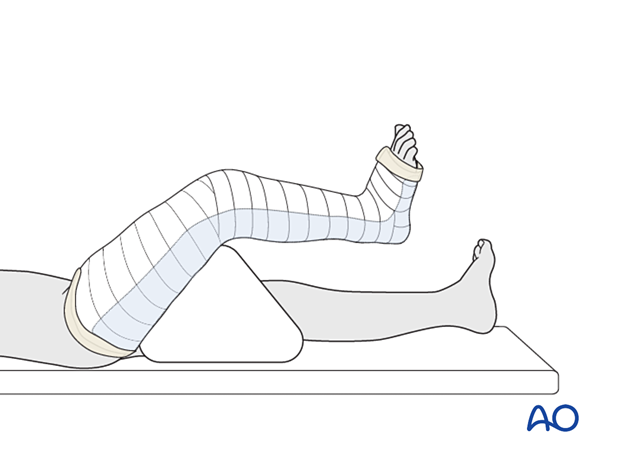
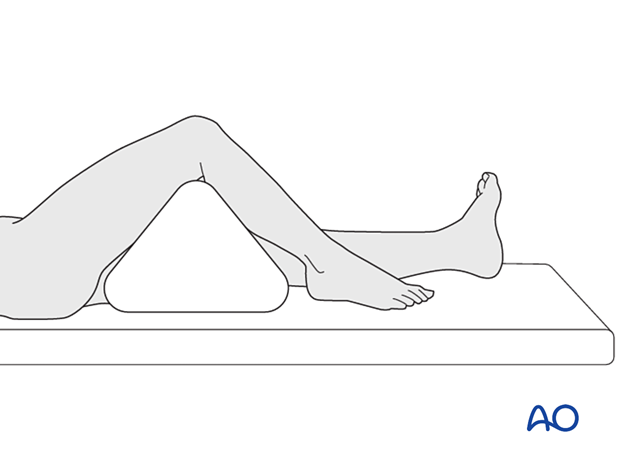
2. Patient preparation
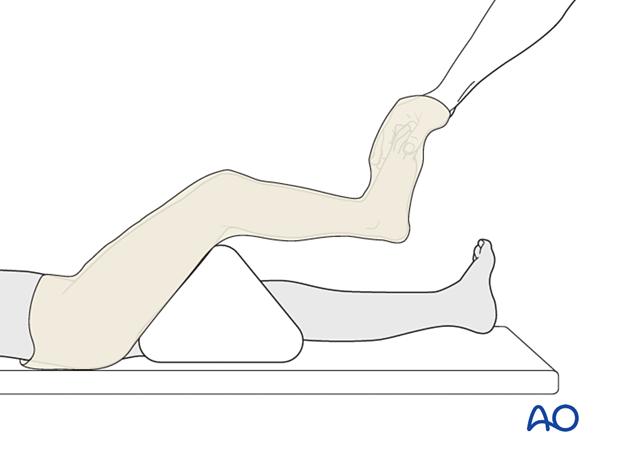
Place the patient in a supine position on a radiolucent table.
Put a bolster or triangle underneath the knee.
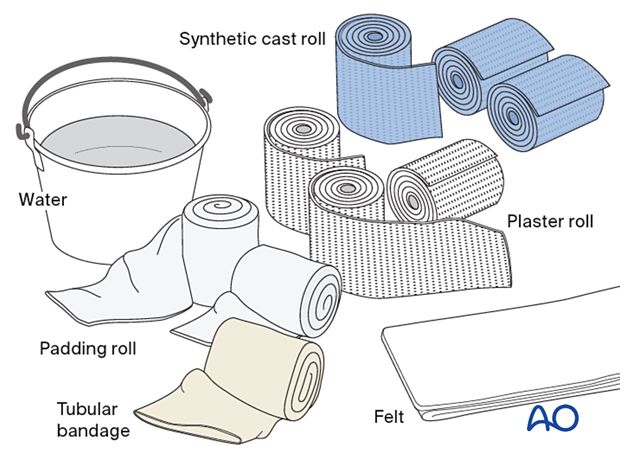
3. Material
- Tubular bandage (stockinette) of appropriate size
- Cast padding
- Felt
- Casting material: synthetic, plaster of Paris, or a combination of both
- Water
The water temperature should ideally be between 22° and 25° C.
4. Closed reduction
With the knee flexed and stabilized, apply longitudinal traction through the foot.
Correct translation and angulation, and confirm reduction clinically and with an image intensifier if available.

5. Casting
Dressing
An assistant supports the leg with knee flexion.
The distal edge of the cast extends to the base of the toes. The proximal edge lies just below the groin.
Apply a tubular bandage and cut it slightly longer than the length of the final cast.
The assistant holds the toes, not the stockinette, with the ankle in a neutral position.
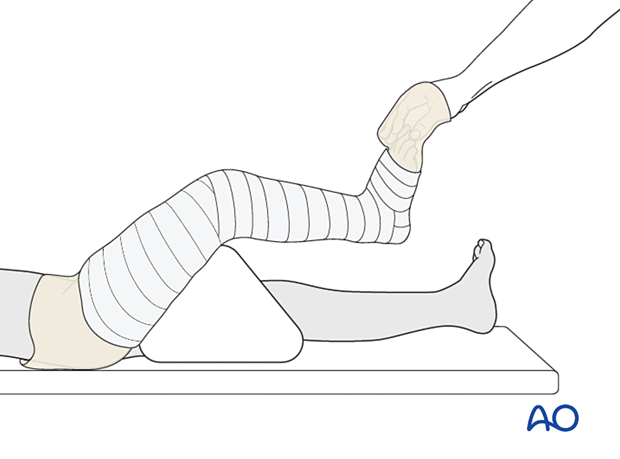
Padding
Consider adding thick felt or additional padding at the free edges of the cast and prominent areas (eg, fibular head, patella, tibial crest, malleoli, and heel) to prevent pressure sores.
Apply cast padding without creases, overlapping each layer by 50%.
It should be appreciated that, when more padding is applied, there will be less support at the injury site.
Cast application to the lower leg
The assistant holds the ankle in a neutral position if the fracture configuration allows.
Apply the first layer of cast material and overlap each layer by 50%.
Avoid sharp edges at the ends of the cast. Make sure the upper end of the cast is well below the popliteal fossa.
Apply further layers of cast material to produce sufficient stability.

Fold the tubular bandage and padding over the lower edge of the cast before applying the final layer of casting material to the leg.
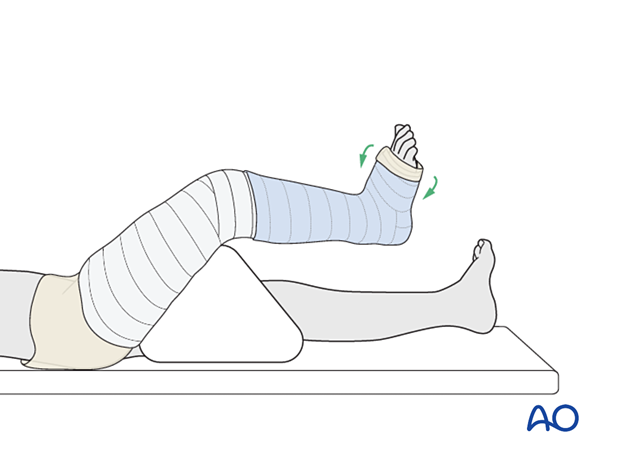
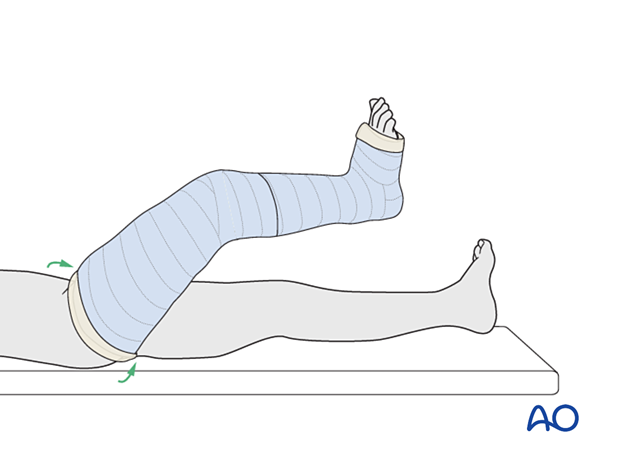
Extending the cast
Remove the triangular support.
Do not increase knee flexion while applying the upper part of the cast. This prevents injury to the skin behind the knee by the edge of the lower cast.
Extend the cast to include the thigh, overlapping the upper part of the leg cast.
Fold the tubular bandage and padding over the upper edge of the cast before applying the final layer of casting material to the thigh.
6. Final assessment
After cast application, check the fracture configuration with x-rays in both planes.
7. Aftercare
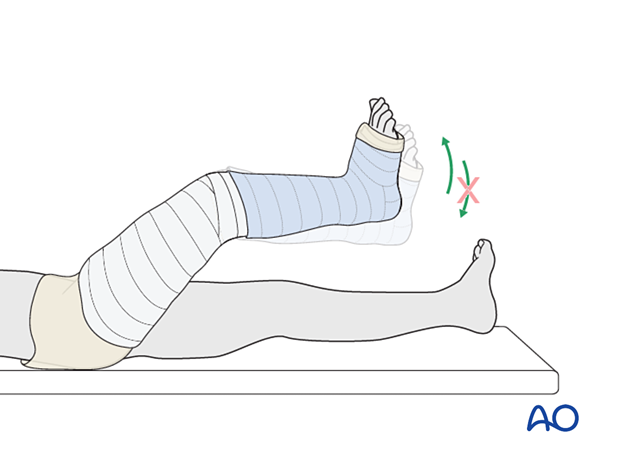
Instructions to parents/carers
Parents/carers should understand the following precautions and instructions:
- Elevate the foot to the level of the heart to avoid swelling
- Check daily for swelling, discoloration, and impaired toe circulation (any of which should be reported urgently)
- Immediately report signs suggesting skin irritation ulceration, and cast soiling
- Make sure the cast padding remains dry and avoid inserting anything between the cast and skin
- Encourage active toe movement
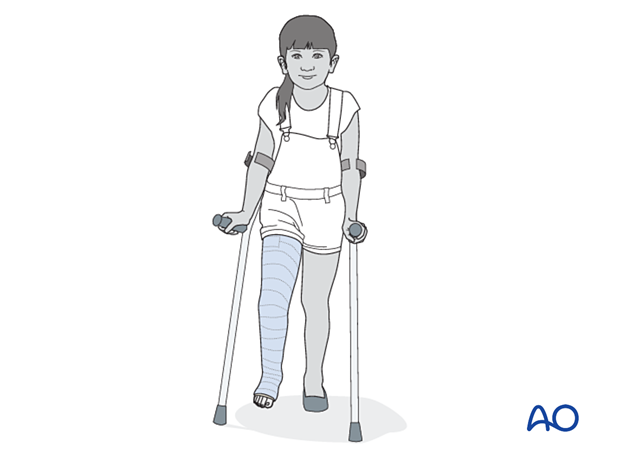
Immediate postinjury care
Non-weight-bearing or touch weight-bearing is encouraged for unstable injuries.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Routine pain medication is prescribed for 3–5 days after injury if required.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after injury to confirm fracture stability.
Cast removal
Physeal and metaphyseal fractures heal rapidly, and the cast is typically removed 3–6 weeks after injury.
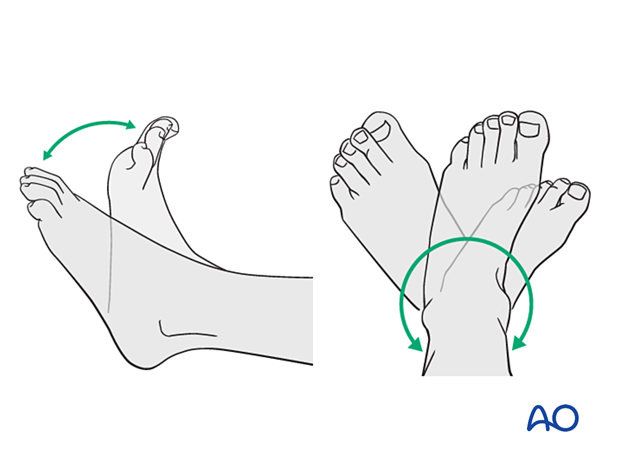
Mobilization
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be necessary in some cases but is not mandatory.
Activities that involve running and jumping are not recommended until full recovery of local symptoms.
Follow-up for growth disturbance
All patients with distal tibial physeal fractures should have continued clinical and radiological follow-up to identify signs of growth disturbance.
Compare alignment and length clinically with the uninjured leg.
A Harris growth arrest line, parallel to the physis, is radiological evidence of continuation of normal growth.
Recommended reading:
- Nguyen JC, Markhardt BK, Merrow AC, et al. Imaging of Pediatric Growth Plate Disturbances. Radiographics. 2017 Oct;37(6):1791–1812.













