Closed reduction; screw fixation
1. General considerations
Introduction
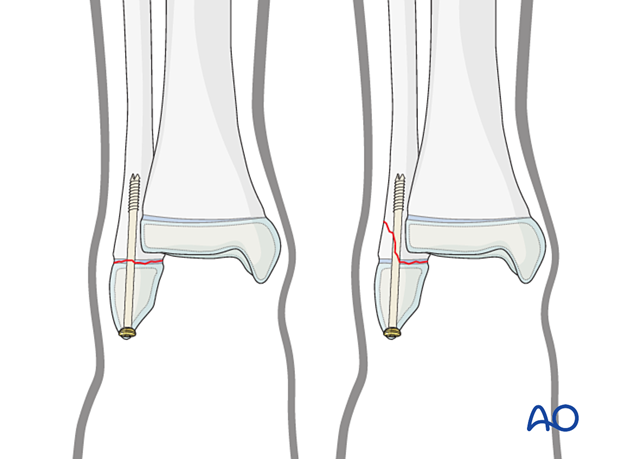
The physeal fragment is fixed with a retrograde intramedullary screw. This risks growth arrest and is only recommended in adolescents.
Open reduction is necessary if it is not possible to obtain or maintain adequate reduction by closed manipulation.
Treatment goals
The main treatment goals are:
- Stabilize the fracture
- Minimize further physeal injury
2. Instruments and implants
Appropriately sized cannulated or noncannulated screws can be used.
The following equipment is used:
- Screw set
- Drill
- Image intensifier

3. Patient preparation
Place the patient in a supine position on a radiolucent table with a block under the heel.

4. Reduction
Apply longitudinal traction through the foot.
If this is not successful, consider open reduction.

5. Fixation
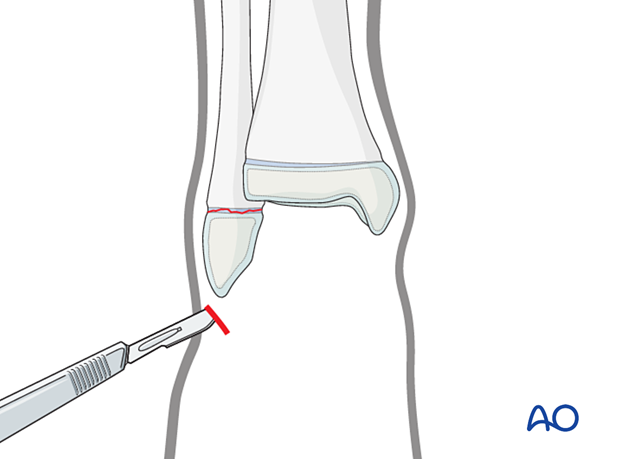
Incision
Perform a stab incision the tip of the fibula.
Spread the underlying soft tissues with a clamp and place a soft-tissue protector down to the bone.
Screw insertion
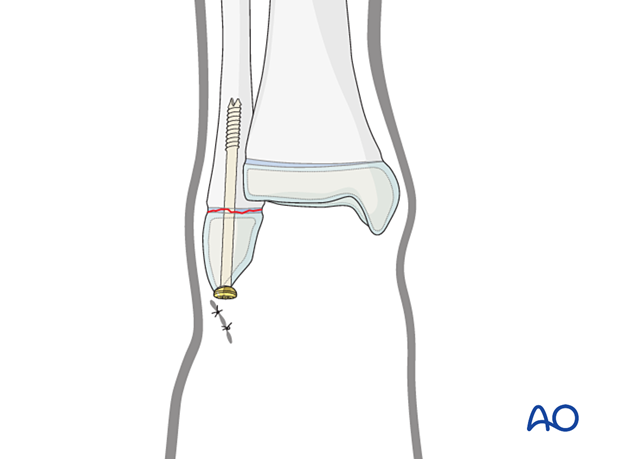
Insert a screw in a standard manner.
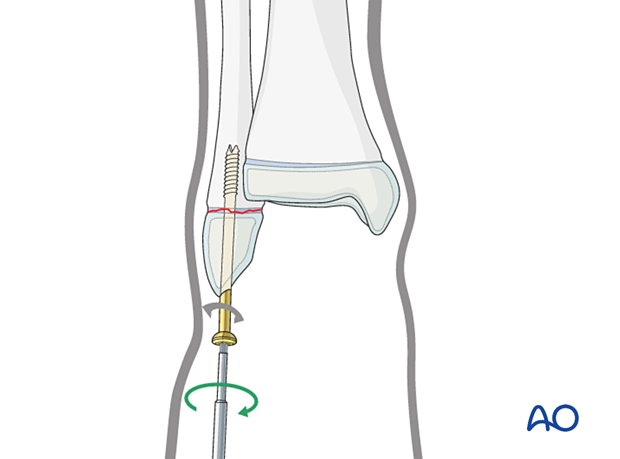
Assessment of reduction
Confirm reduction, fracture stability, and screw placement with an image intensifier.
Close the percutaneous incision.
6. Immobilization
A molded below-knee cast or fixed ankle boot is recommended for a period of 2–6 weeks as the strength of fixation may not provide sufficient stability for unrestricted weight bearing.
7. Aftercare
Immediate postoperative care
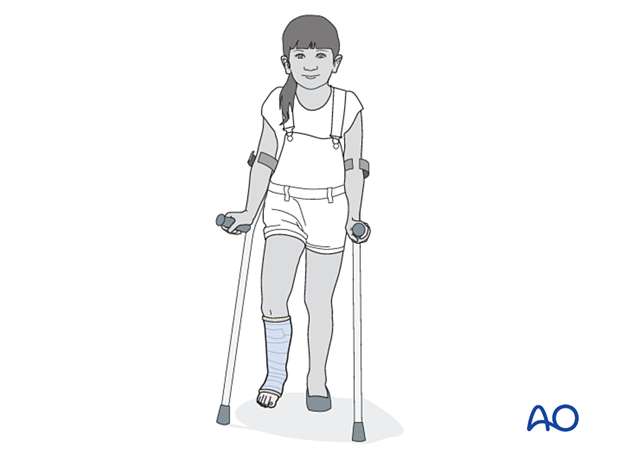
Weight-bearing is encouraged.
Older children may be able to use crutches or a walker.
Younger children may require a period of bed rest followed by mobilization in a wheelchair.
Pain control
Patients tend to be more comfortable if the limb is splinted.
Routine pain medication is prescribed for 3–5 days after surgery.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Discharge care
Discharge follows local practice and is usually possible within 48 hours.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days after surgery to check the wound and confirm that reduction has been maintained.
Cast removal
A cast or boot can be removed 2–6 weeks after injury.
Mobilization
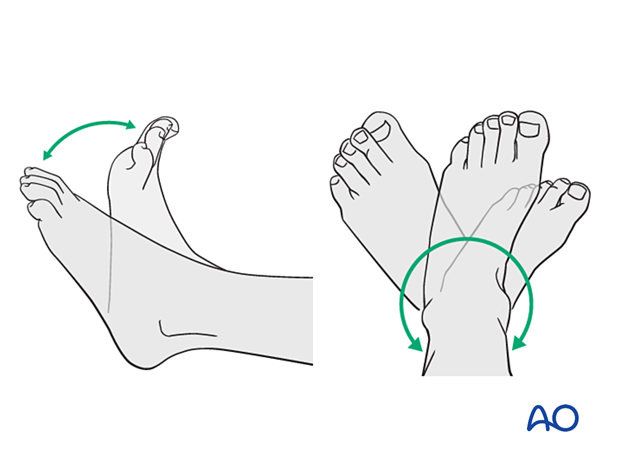
After cast removal, graduated weight-bearing is usually possible.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be required in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.













