Closed reduction; K-wire fixation followed by casting
1. General considerations
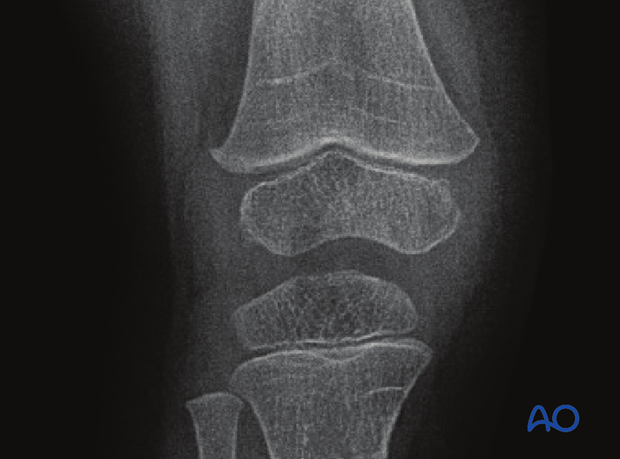
This technique is used for extraarticular distal femoral fractures including Salter-Harris I and II, and low metaphyseal fractures in patients with open growth plates.
Stabilizing these fractures requires temporary internal fixation across the growth plate to produce adequate stability.
To minimize secondary damage to the growth plate, manipulation must be gentle. Multiple passes across the growth plate with a K-wire should be avoided.
Smooth, narrow K-wires reduce the risk of physeal damage.
Threaded K-wires may increase fracture stability.
2. Instruments and implants
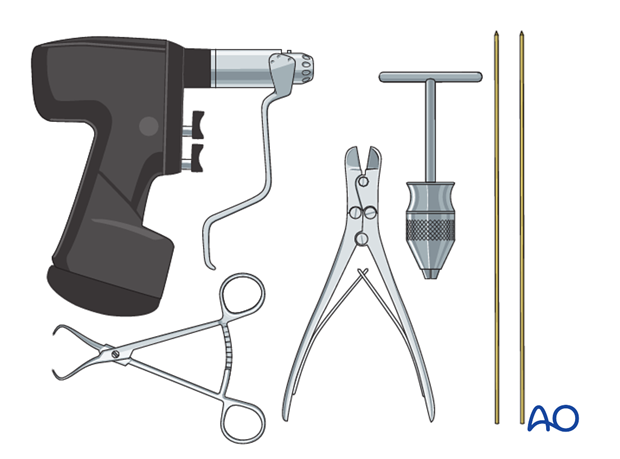
The following equipment is needed:
- K-wires of appropriate sizes
- Drill or a T-handle for manual insertion
- Wire cutting instruments
- Standard orthopedic instrument set
3. Patient preparation
Place the patient in a supine position on a radiolucent table.
Flexion of the knee is often helpful for reduction. Bolsters to support the tibia may help in maintaining reduction. Breaking the table to allow knee flexion may also facilitate traction and reduction.
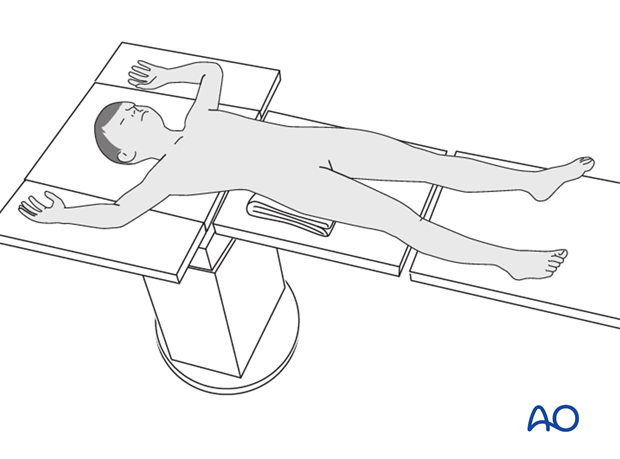
Alternatively, the patient may be positioned prone. This allows reduction with traction and knee flexion similar to dealing with supracondylar fractures of the distal humerus.
Following successful reduction and stabilization with K-wires, place the patient in a supine position for application of a plaster cast.
4. Reduction
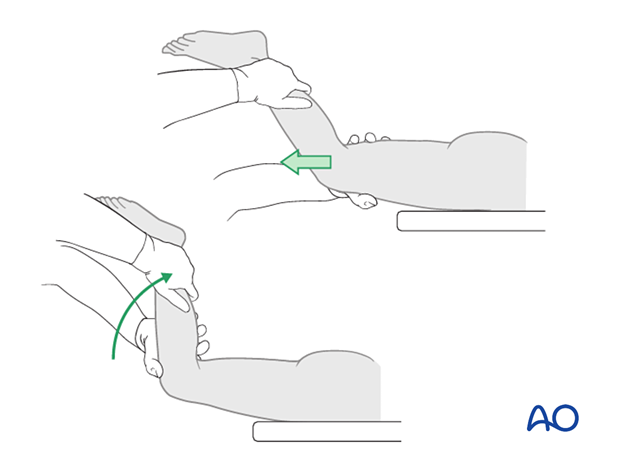
Place the anesthetized patient supine on a radiolucent table.
Because of the irregularity of the distal femoral physis reduction must be applied with care.
Gentle, prolonged longitudinal traction is the most important maneuver to avoid damage to the growth plate.
After a sufficient period of traction, gently manipulate the limb to reduce the fracture.
An assistant should be available to apply countertraction.
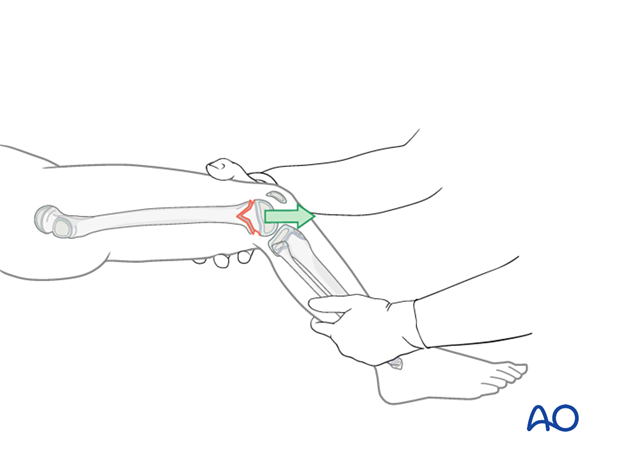
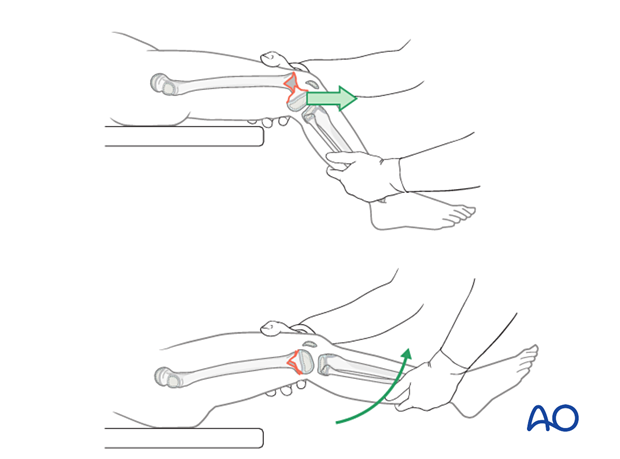
In the more common extension-type fracture, initially apply traction with the knee in 30°–45° flexion and then gently flex the knee to 90°, maintaining longitudinal traction.
Confirm reduction with image intensification.
Alternative: Traction and knee flexion, with the patient prone, is an alternative reduction maneuver, similar to dealing with supracondylar fractures of the distal humerus.
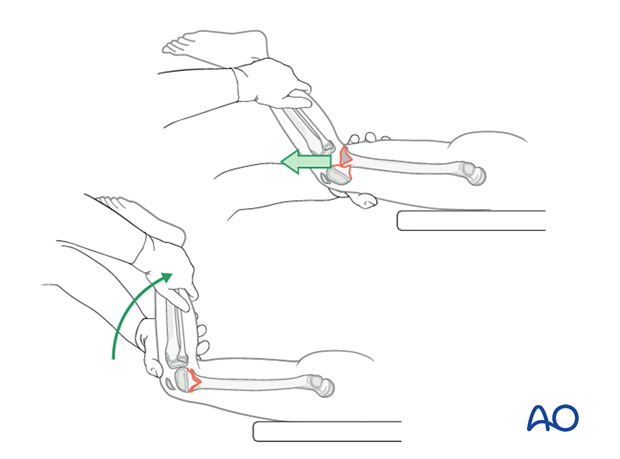
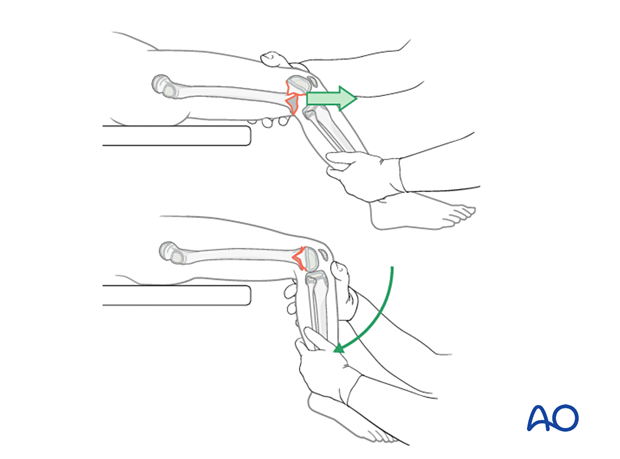
In a flexion-type fracture, initially apply traction with the knee flexed to 45° and then gently extend the knee.
Confirm reduction with image intensification.
In a valgus displaced fracture, initially apply longitudinal traction to the knee and then gently apply a varus force to the leg.
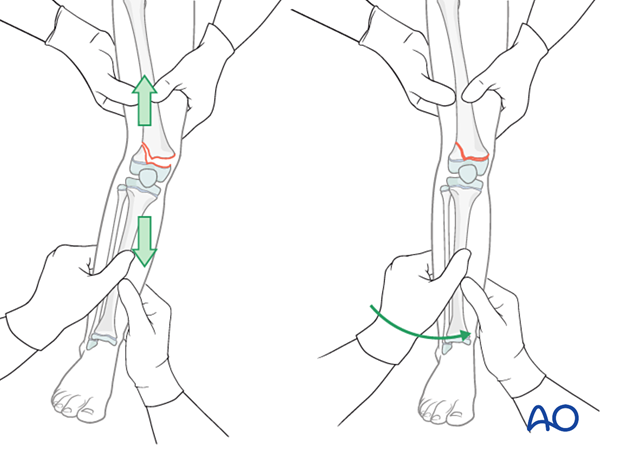
In a varus displaced fracture, initially apply longitudinal traction to the knee and then gently apply a valgus force to the leg.
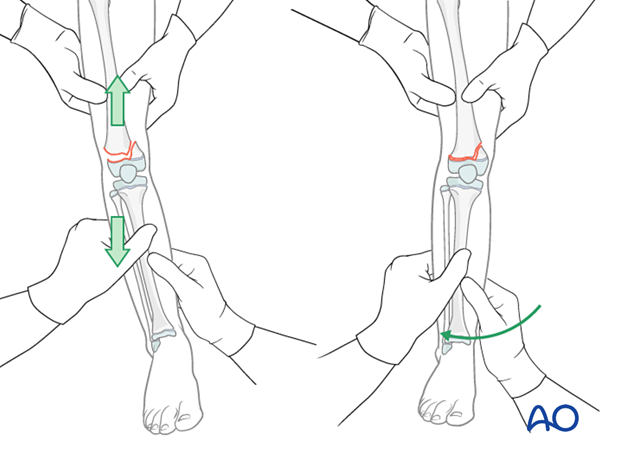
Confirm reduction with image intensification.
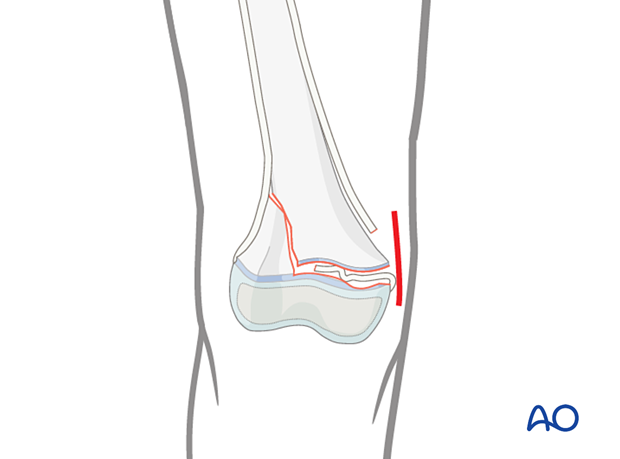
In SH I and II fracture patterns, there is a risk of incarcerated periosteum.
If a gap remains after reduction, a small open approach may be required to release the periosteum.
5. Fixation
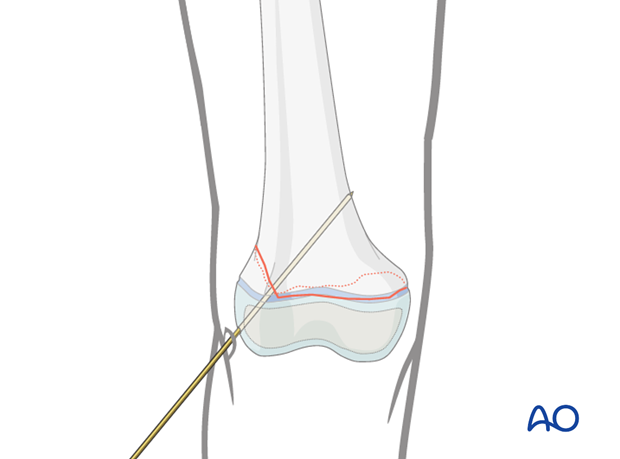
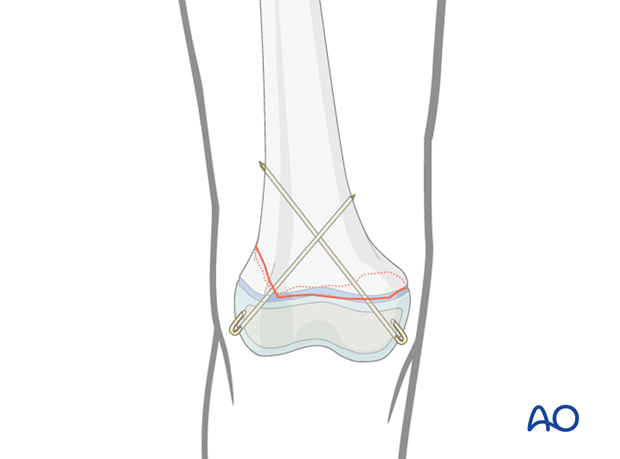
Insertion of first K-wire
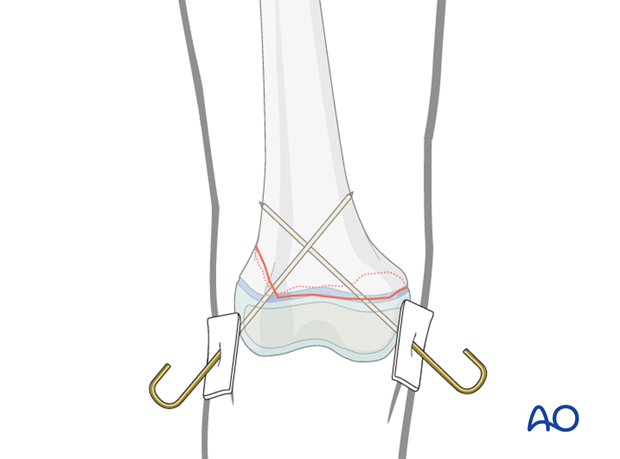
Insert the first K-wire from distal to proximal starting on the lateral femoral condyle.
Advance the K-wire across the growth plate after confirming a trajectory that will engage the metaphysis of the medial supracondylar region on AP and lateral views.
Engage the K-wire in the cortical bone of the medial supracondylar region.
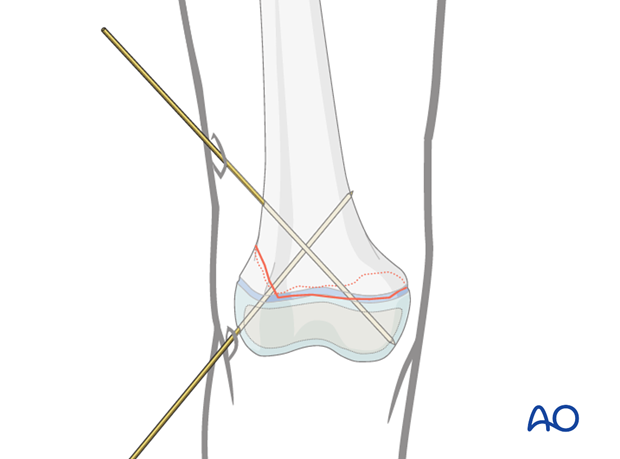
Insertion of second K-wire
The second K-wire may be inserted from distal to proximal starting on the medial femoral condyle, ...
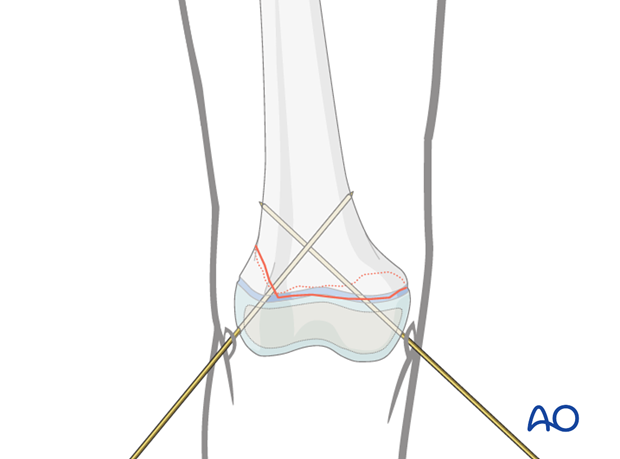
... or from proximal to distal starting in the lateral supracondylar region.
In either case, maximize the spread of the K-wires at the fracture site to increase stability.
K-wire cutting and dressing
Bend the K-wires approximately 2 cm from the skin to allow for swelling as illustrated.
Cut the K-wires and apply a dressing or sponge to stabilize the K-wires against the skin ...
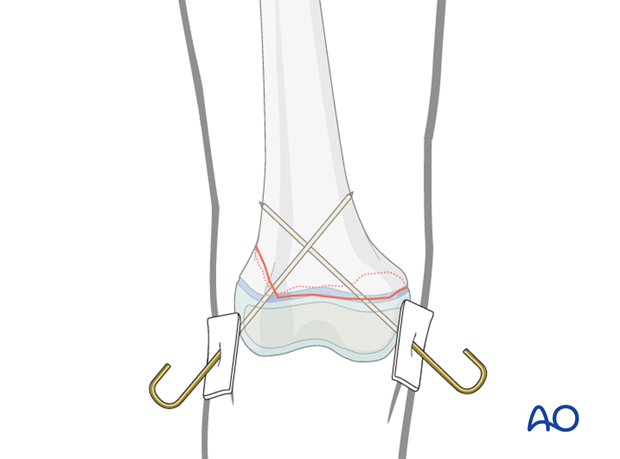
... or the K-wires may be buried.
6. Final assessment
Check implant position and fracture reduction with image intensification.
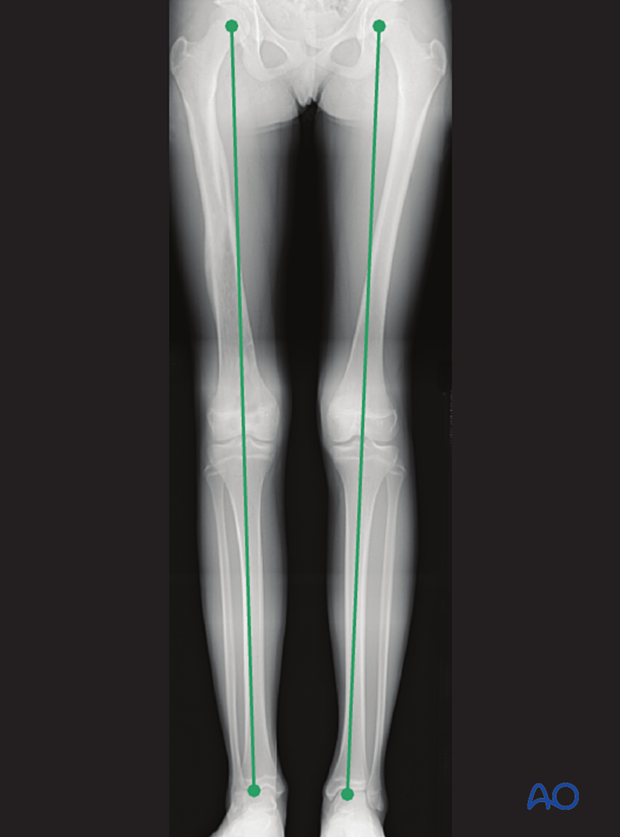
Use clinical examination to check lower extremity alignment.

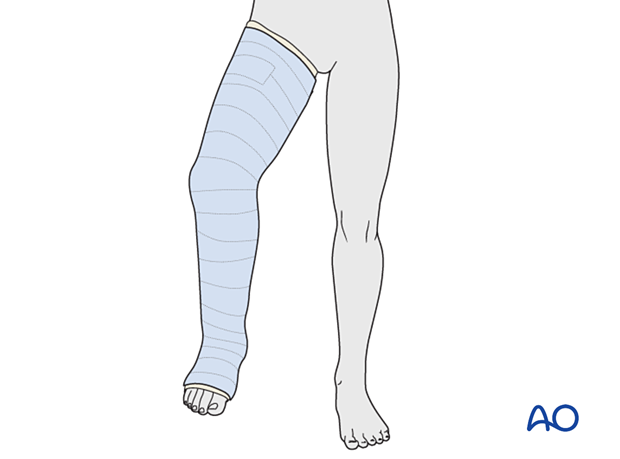
7. Application of cast
A molded cast is mandatory because the strength of the K-wires is inadequate to neutralize muscle forces.
Apply a long leg cast with the knee flexed 30°–45°.
8. Aftercare
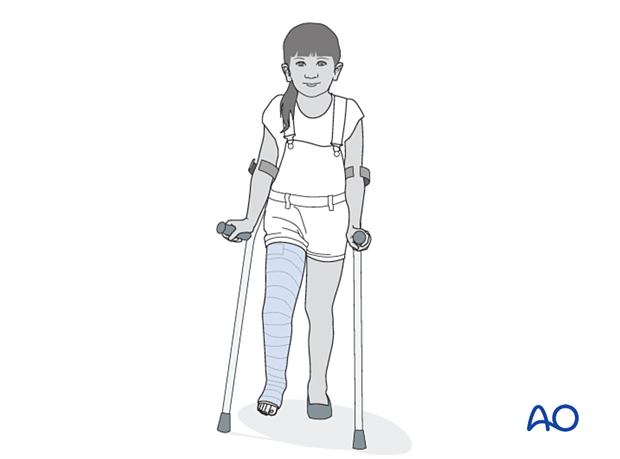
Immediate postoperative care
The patient is kept touch-weight bearing to decrease forces across the fracture. Older children may be able to use crutches or a walker. For younger children, bed rest and a wheelchair is more reliable.
Analgesia
Routine pain medication is prescribed for 3–5 days postoperatively.
Neurovascular examination
The patient should be examined regularly, to exclude neurovascular compromise or evolving compartment syndrome.
With displaced high-energy fractures watch for signs of delayed vascular problems.
Discharge care
Discharge from hospital follows local practice and is usually possible after 1–3 days.
Follow-up
The first clinical and radiological follow-up is usually undertaken 5–7 days postoperatively to confirm reduction.
Cast and K-wire removal
Physeal fractures heal quickly and cast and K-wires are typically removed 3–6 weeks after injury.
Mobilization
Once K-wires and cast are removed, partial weight bearing and knee range-of-motion exercises are started.
Follow-up for growth deformity
All patients with physeal fractures of the distal femur should have clinical and radiological examination 8–12 weeks postoperatively to assess for signs of physeal growth disturbance or resumption of growth.
Examination should be repeated at intervals until resumption of normal growth is documented. This can be seen as a horizontal growth line (Harris line) that is parallel to the entire physis on both AP and lateral views.
A growth line that converges towards the growth plate may be the earliest sign of growth arrest and should prompt investigation/treatment or referral as appropriate.
Clinical assessment of leg length and alignment is recommended at one-year.
Clinical assessment of leg length uses a tape measure from the ASIS to the medial malleolus.
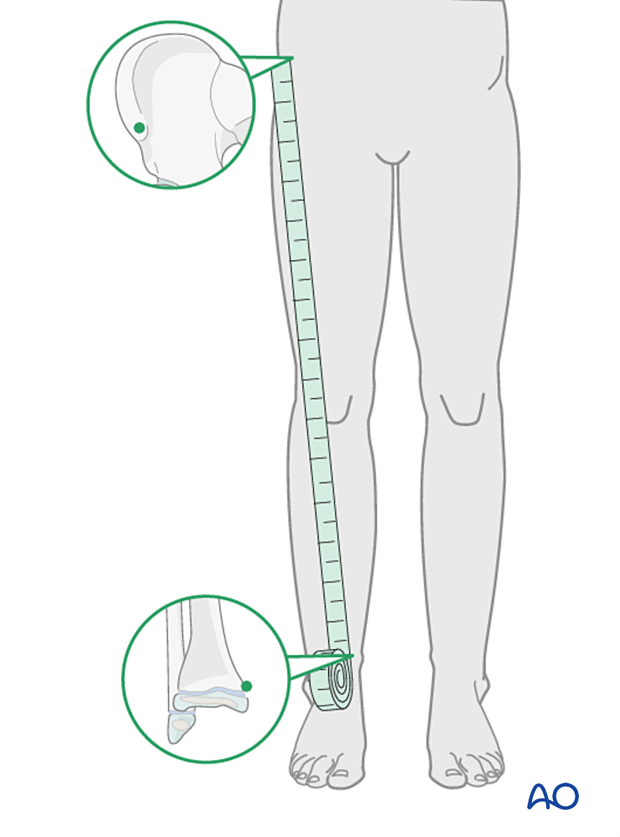
If there is any concern about leg length discrepancy or malalignment, long leg x-rays are recommended.
Leg length is measured from the femoral head to the ankle joint.