Intramedullary nailing
1. Principles
Intramedullary nailing
Intramedullary fixation is valuable and appropriate for the majority of tibial fractures. It is well-suited for the mid diaphysis. With newer nail designs and attention to technique, nailing can be extended to both proximal and distal extraarticular fractures.
If the medullary canal is deformed (e.g. prior fracture, or developmental abnormality) nailing may not be possible.
If severe bacterial contamination or infection are present, nailing may spread infection through the medullary canal, and should be avoided. External fixator pins are a common source of contamination. If such pins appear to be infected, or have been present for more than 2–3 weeks, preliminary pin removal, debridement, and antibiotics may be advisable before nailing.
Intramedullary nailing in severe trauma may cause respiratory distress.
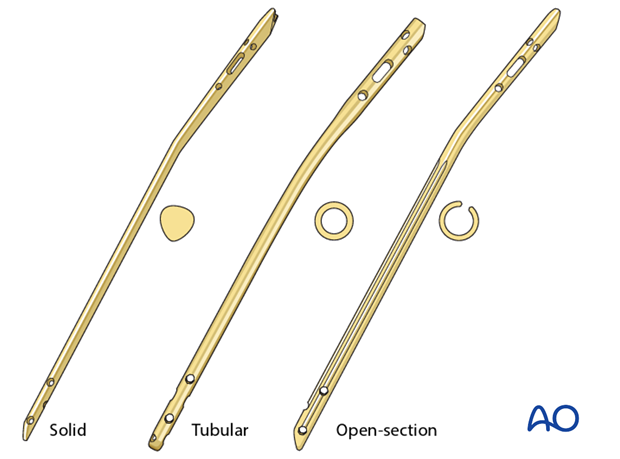
Available tibial nails
Currently available tibial nails have locking screw holes close to both ends, in multiple orientations, for better fixation of proximal and distal fractures. The nails may be either solid or cannulated (hollow). Solid nails may protect somewhat against infection because they have no internal dead space.
The surgeon should be familiar with the nails available in his/her institution, particularly the available sizes. Instrumentation and details of technique vary among nail systems. This should be considered in preoperative planning and surgery.
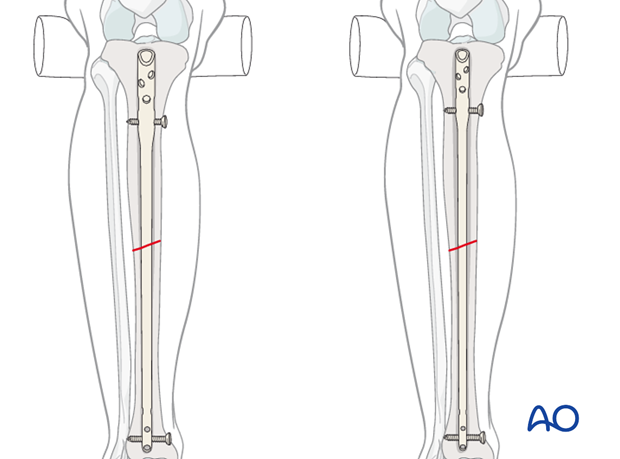
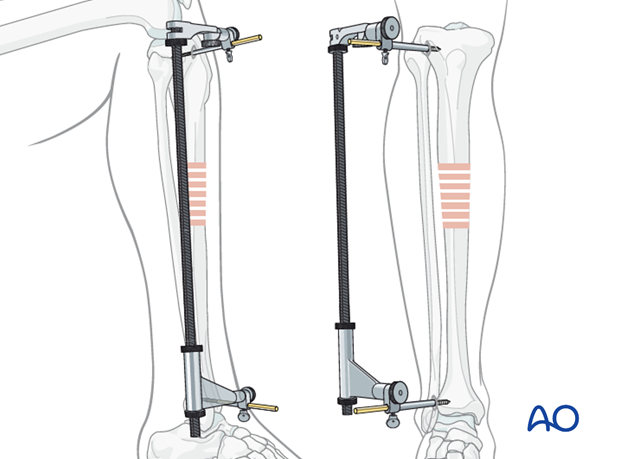
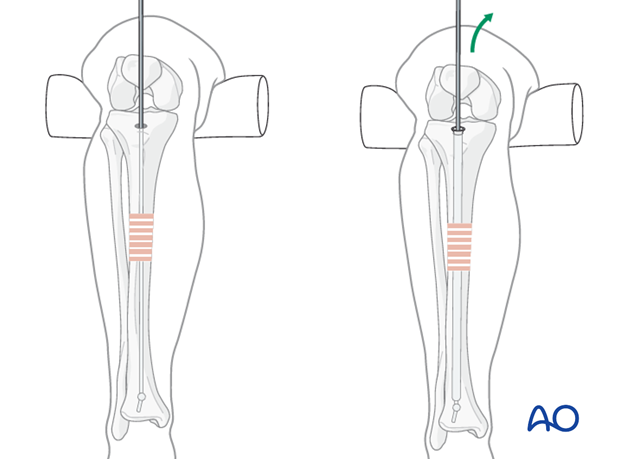
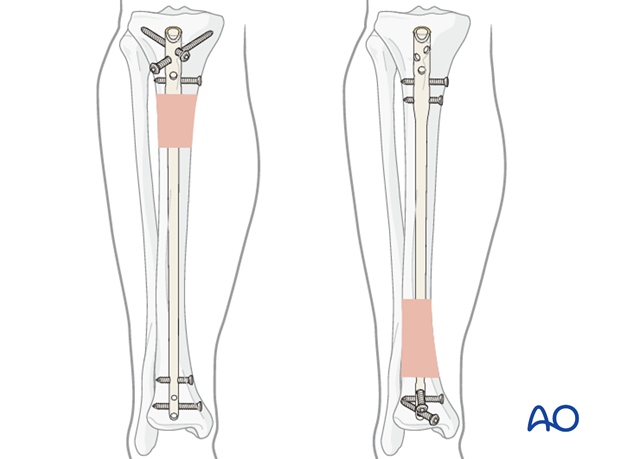
Reamed nailing
The diameter of the tibial medullary canal varies significantly. It may be 8 mm or less. Reamers can be used to enlarge the medullary canal for larger diameter nails. Such nails permit larger diameter locking screws. Both nail and screw strength and durability increase with diameter. The medullary canal should be reamed a bit larger than the intended nail diameter (usually about 1.5 mm more), to ease nail insertion. The image illustrates a non-reamed nail on the left, and a reamed nail on the right. Stability is increased with the reamed technique, because the nail fits snugly in a longer portion of the tibial shaft.
Reaming is currently favored for most tibial nailing, but this should be done gently when the tibial diaphysis is dense, and the canal diameter is small.
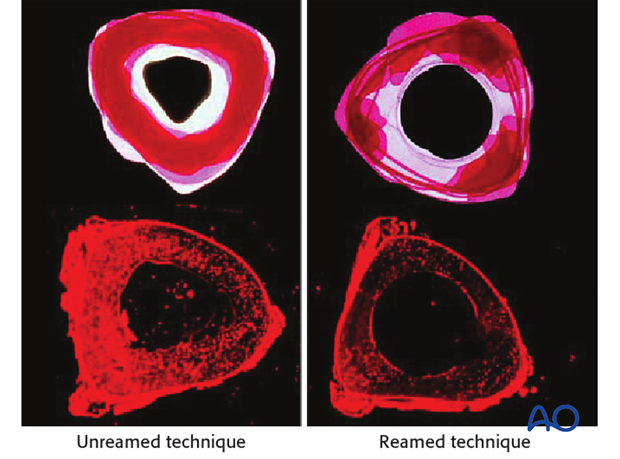
Reaming damages the medullary blood supply and causes temporary necrosis of the diaphyseal bone. Theoretically, this increases the risk of infection, particularly relevant for open fractures. However, clinical studies have not demonstrated that this is very significant.
The surgeon should consider whether or not the benefits of reaming are worth the associated risks when choosing whether or not to use reaming for tibial intramedullary nails.
The individual patient’s medullary canal size, as well as probable mechanical stresses, must be included in this consideration.
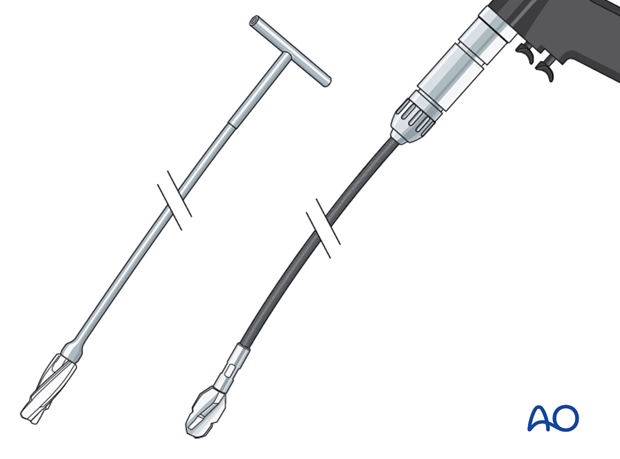
Reamers
These may be either cannulated, and motor driven, or solid hand reamers.
Reamers should be sharp so they cut the bone with little friction, and should have deep flutes and a small diameter shaft. The goal is to minimize pressure in the canal ahead of the reamer, and to avoid friction and resulting overheating of bone and surrounding soft tissues (with resulting full-thickness necrosis of both!).
If the reamer is not cutting bone easily, remove it, clear bone clogging the flutes, and resume reaming slowly and cautiously.
The first reamer of a series should be shaped so that its tip cuts into the bone. Subsequent reamers need only cut against the sides of the medullary canal.
The illustration shows a solid hand reamer (left) and a power reamer (right).
Teaching video: reamed nailing technique
AO teaching video: Tibia Fractures - Intramedullary Nailing with the Expert Tibial Nail (with reaming)
Non-reamed nailing
Non-reamed nailing was developed in hopes of reducing risks of infection and pulmonary dysfunction from embolized medullary debris. These benefits are usually not clinically significant. Since smaller diameter, “non-reamed” nails are mechanically weaker, particularly with regard to smaller locking screws, their reoperation rate is higher.
Such nails may be used for smaller diameter medullary canals, or selected indications, (e.g. increased risk of infection) according to the surgeon’s preference.
Teaching video: non-reamed nailing technique
AO teaching video: Tibia Fractures - Intramedullary Nailing with the Expert Tibial Nail (without reaming)
Locking screws
Modern IM nails permit placement of locking screws through bone and nail, to improve fixation both proximally and distally. Locked nails permit stable fixation which controls length, rotation, and alignment of proximal and distal fractures. However, locking prevents impaction of distracted fractures, and interferes with their healing.
When locking nails were first introduced, their potential for impaired healing was recognized. Delayed removal of locking screws (“dynamization”) was often advised. This is usually not necessary if distraction is avoided, but may be considered when a fracture fixed with length-stable locking is healing slowly. Length-stable locking is often called “static” locking.
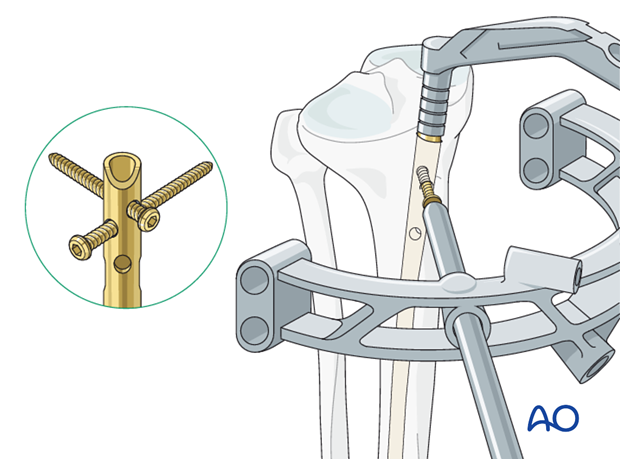
Some locking screw holes are designed with an oval shape so that a screw at one end of the oval will allow some fracture impaction, but still control rotation as well as limit shortening to the length of the oval. These have been called “dynamic locking” screw holes (see illustrations).
To ensure adequate fixation of acute tibial fractures, use of locking screws both proximally and distally is advisable. Dynamic (oval) rather than static (round) holes may be used when the fracture pattern prevents shortening.

2. Patient preparation and approach
Patient preparation
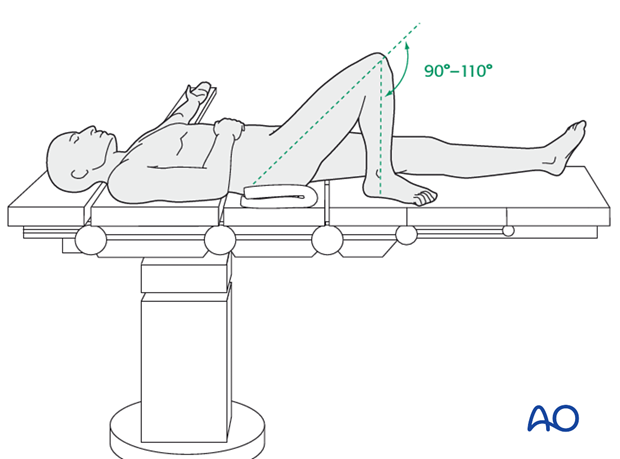
This procedure is normally performed with the patient in a supine position for nailing.
Approach
For this procedure an intramedullary nailing approach is used.
3. Reduction and preliminary fixation
Preliminary remark
Reduction is an essential part of intramedullary nailing. The fracture must be reduced to allow guide-wire placement, during reaming, and during nail insertion. Length, angulation, and rotation are all important to restore. Even after guide-wire insertion, further correction of alignment may be needed to avoid deformity. This should be done before reaming and nail insertion.
Reduction is usually more challenging with proximal and distal fractures as well as with delayed treatment. Sometimes only mild traction and rotational adjustment are required. Percutaneous reduction aids (pointed reduction forceps, Schanz screws or ball-spike pusher) may allow reduction without opening the fracture. With other fractures, open reduction may be necessary.
Unless the fracture is older and consolidated, the surgeon usually begins with less invasive reduction techniques, and if they do not succeed, progresses to techniques which require more fracture exposure .
The following illustrations of the different reduction techniques provide examples that can be used or modified as necessary.
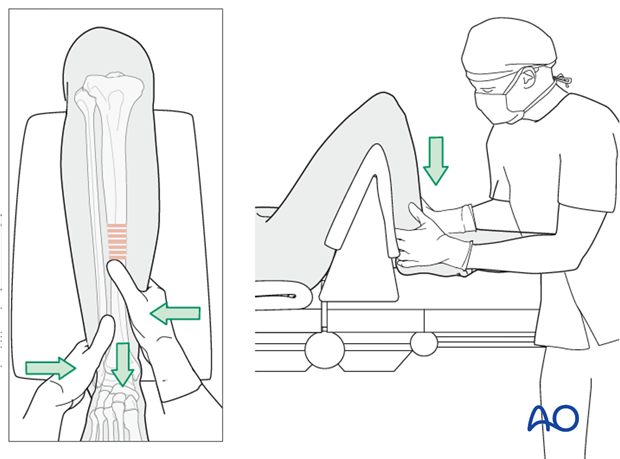
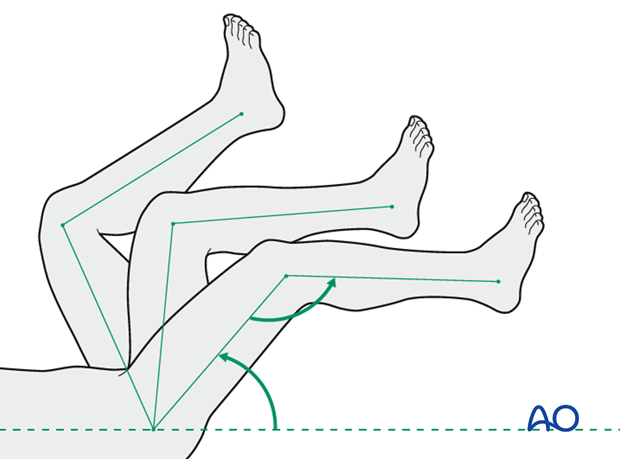
Manual traction
Depending on the patient’s positioning and type of OR table, one or two people may be required to perform manual traction.
The illustration shows a triangular radiolucent supporting frame, with padding over top, placed proximal to the popliteal fossa. It provides “countertraction” when the fracture is lengthened with distal traction.
For patients positioned on a radiolucent table without knee support, one person holds the leg and the other pulls the leg distally.
During traction, the reduction is controlled by palpating the tibial crest and the anteromedial surface.
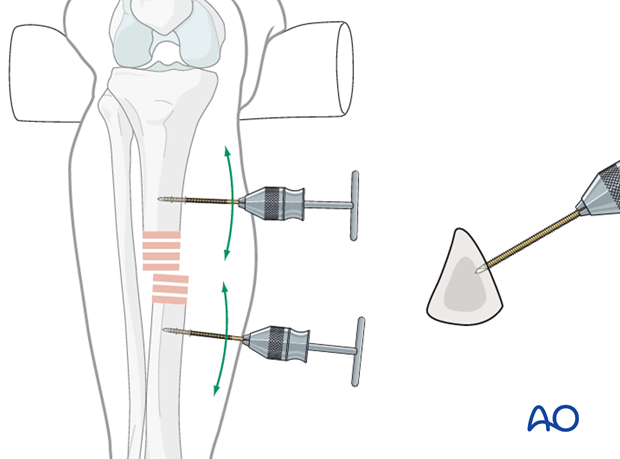
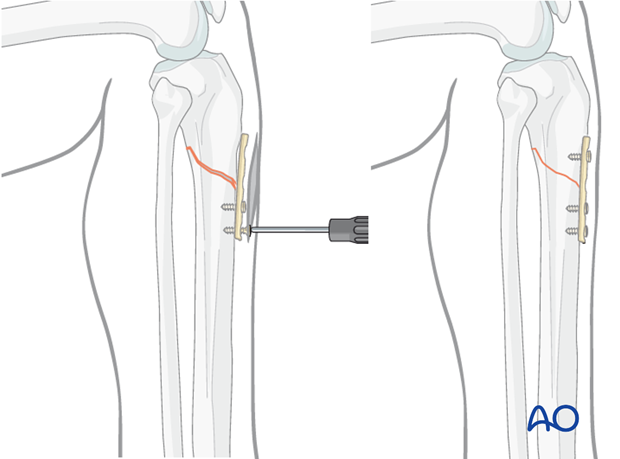
Using a distractor
A large distractor is usually placed in a coronal plane. It lies posterior to the tibia, either laterally or medially. Do not obstruct planned locking screws or x-rays.
The proximal Schanz screw must be proximal and sufficiently posterior to avoid blocking the nail. Place it parallel to the tibial plateau to aid proximal fracture alignment. The distractor’s distal pin should be outside the intended nail location, posteriorly in the distal tibia, or in the talus.
An external fixator may be used instead of the distractor. Pin placements are the same.
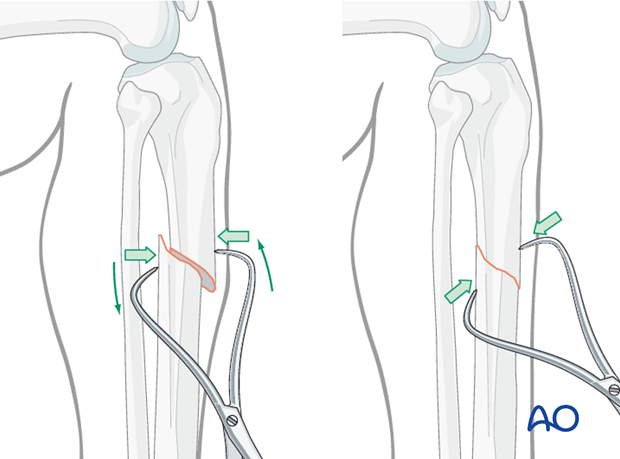
Joysticks
To aid reduction, a “joystick” (in this case a Schanz screw on a T-handled chuck) can be placed into either or both main tibial fragments.
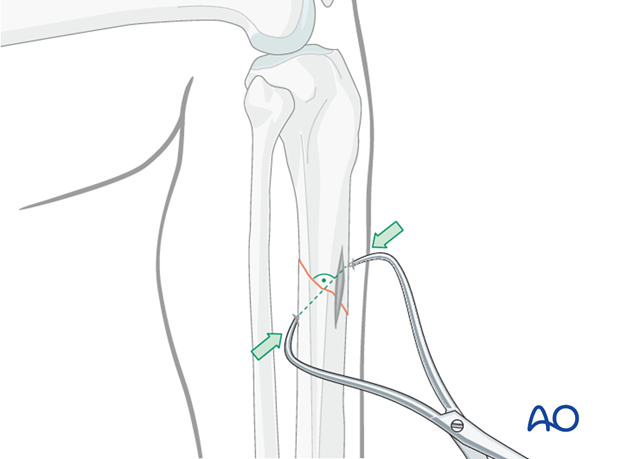
Percutaneous reduction forceps
Oblique or spiral fractures can often be reduced with a pointed reduction forceps applied percutaneously.
Open reduction
In the event of delayed treatment, or if a bone fragment is stuck in the canal, open reduction is performed.
In open reduction, the preservation of the periosteum, and peripheral soft-tissue attachments is recommended.
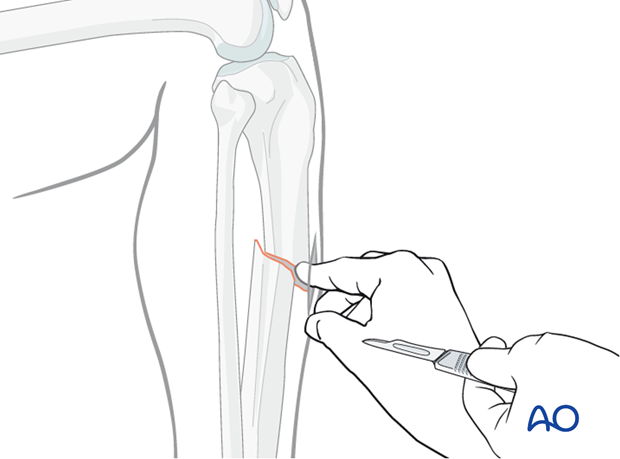
Incision
Locate the fracture by palpation or with image intensifier. Make a small longitudinal incision over the fracture. Extend the incision sufficiently for access. Free up one side of the fracture at a time, with minimal dissection.
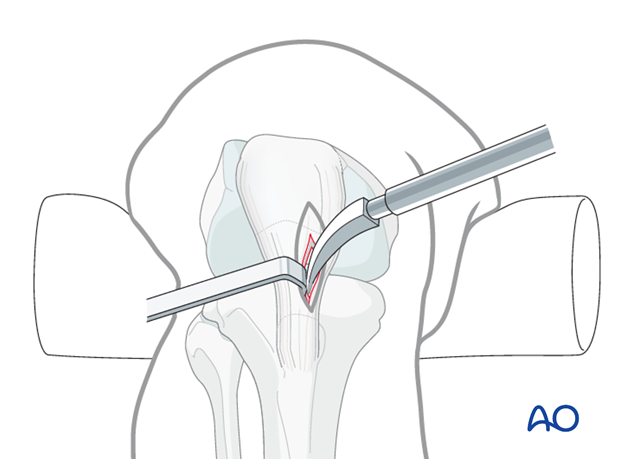
Oblique fractures
If the fracture is oblique, a bone clamp, placed percutaneously, with its tips perpendicular to the fracture plane, can be used to compress the fracture surfaces. Together with some traction, this helps restore length as well as fracture apposition.
Transverse fractures
If the fracture is transverse, it may be reduced with manipulation using clamps on the bone ends. This may require excessive exposure. Percutaneous Schanz screws, or percutaneously applied pointed reduction forceps, as illustrated, are less invasive.
The technique with clamps is as follows:
Free up the ends of both fracture fragments. Align the crest of both fragments. This will assure proper rotation.
Flex the fracture to 45 degrees, or enough to place one fragment onto the other. Approximate the cortical edges, and gradually straighten the fracture, which compresses the fracture site. Recheck alignment.
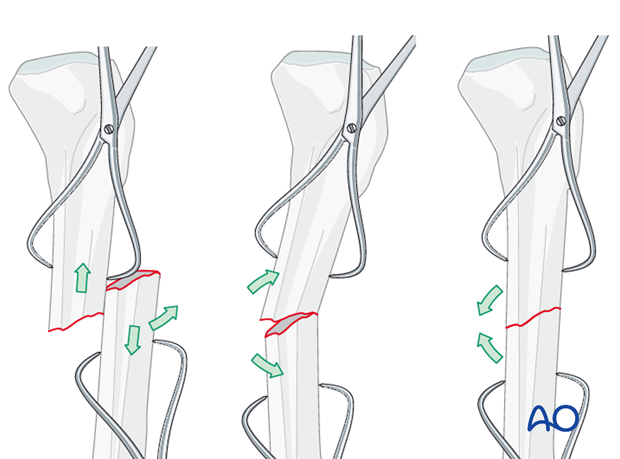
Alternatively, a Hohmann retractor can be used for reduction by placing it between the fracture fragments and prying them apart. It is important to hold this position for at least 30 seconds to allow the visco-elastic tissues to stretch gradually.
It is very important to maintain the reduction while the nail is inserted. This often requires an assistant, or temporary use of distractor, external fixator, or plate with unicortical screws.
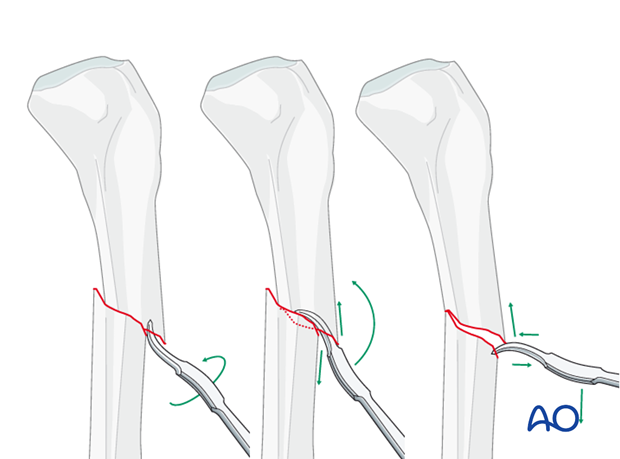
Plate as reduction aid
Particularly for proximal tibial fractures it may be difficult to achieve and maintain reduction while inserting the nail.
As illustrated, a small plate with unicortical screws can be used, both as a reduction aid and to hold the reduction during nail insertion.
This is an open technique, but little soft-tissue dissection is required. The plate can be left in place after the nail is inserted.
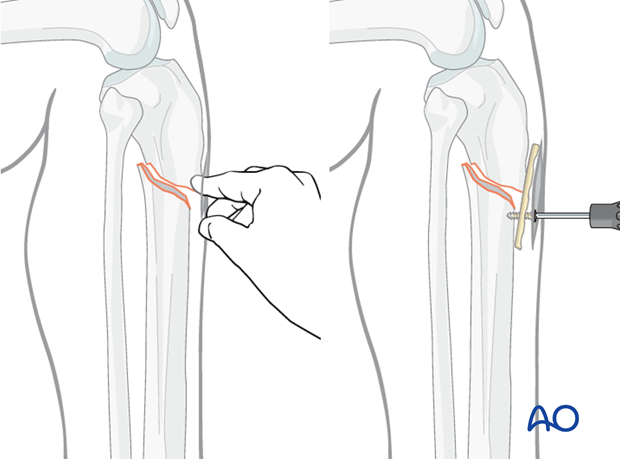
Tightening the straight plate against the distal tibial segment pushes the proximal segment into alignment, thus correcting the gap and apex-anterior angulation. The proximal screw increases stability, to help avoid redisplacement during nail insertion.
Reduction difficulties
Delayed reduction
If nailing will be delayed, a temporary external fixator can maintain distraction, thus aiding reduction. If the fracture consolidates with shortening, closed reduction will be difficult to achieve, particularly after 10-15 days. If an initial attempt at closed reduction is unsuccessful, open the fracture and release enough peripheral callus to allow reduction.

4. Creation of the nail entry site
Approach
For details about determination of the entry point and incising the skin, please refer to the intramedullary nailing approach. Remember that a precisely placed bony entry site is usually essential for successful intramedullary nailing, and that the skin incision must be placed to permit a proper bony entry site, and also to allow a straight, minimally traumatic passage for the nail as it enters the bone.
Tools for opening the bone
A preliminary guide pin helps locate the proper entry site. Various cannulated instruments can be inserted over such a pin. Alternatively, a solid awl can be used for the same purpose. Make sure that the location is correct before the full opening is created.
Placement of the guide pin
Insert a finger through the incision and palpate the anterior edge of the tibial plateau. With the finger in place, insert a guide wire just distal to the finger, essentially just beyond the angle between plateau and proximal metaphysis.
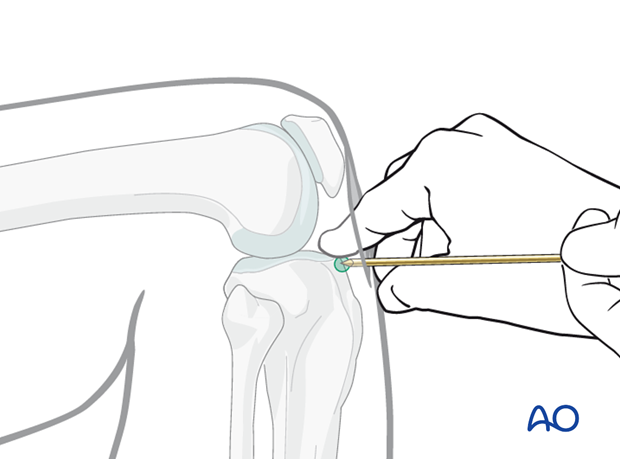
Insertion of the guide pin
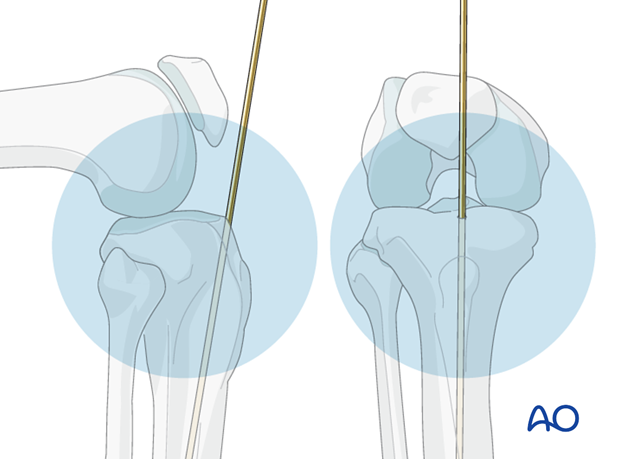
Frontal plane:
Insert the guide wire aiming down the tibial crest, and thus the center of the medullary canal.
Sagittal plane:
Press the guide pin into the bone so the tip does not slip. While entering the bone, correct the guide pin alignment by pushing the proximal end of the pin posteriorly. This brings the pin almost in line with the axis of the tibia, as illustrated.
Radiographic control
Radiographic confirmation of correct guide-wire location and direction is strongly recommended, if possible, before creating the entry in the bone. If the procedure is being done without fluoroscopy, landmarks as described must be used with care to place the entry site in line with the medullary canal.
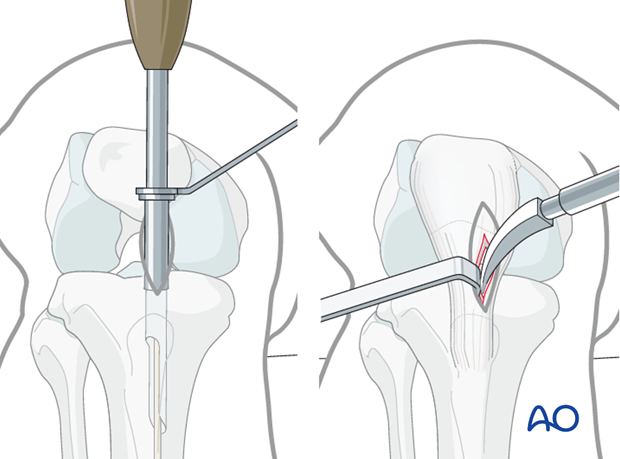
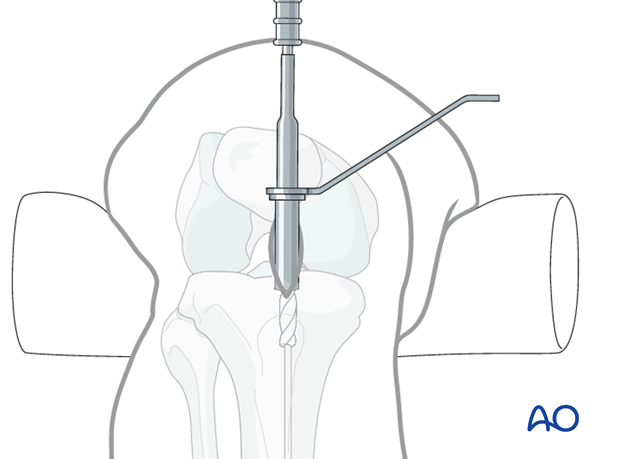
Opening the cortex
The illustration shows entry creation with a cannulated drill inserted over the previously placed guide pin. A protective sleeve minimizes soft-tissue injury.
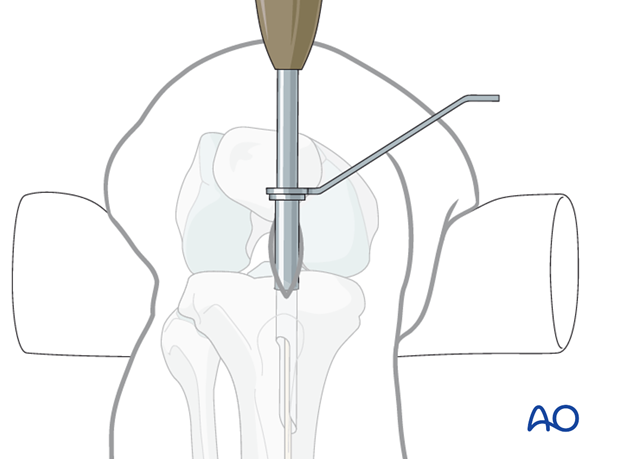
Alternative: cannulated cutting tool
Alternatively, one can use a cannulated cutting tool over the previously placed guide pin to open the entry site, as illustrated.
Alternative: curved solid awl
In addition to cannulated cutting tools, or drills, the cortex can be opened with a solid awl.
The important principle is that the entry site must be placed so that the nail enters the tibia freely, and does not disturb the anatomical fracture alignment. This is very important for proximal tibial fractures.
5. Guide wire insertion
Hand reamer
Entry site preparation with one of the techniques just described usually permits insertion of the guide wire into the diaphyseal medullary canal. If cancellous bone remains in the way, complete the entry with a hand reamer. These instruments (in diameters of 6,7 and 8 mm) are also helpful for old fractures and non-unions, when the medullary canal is plugged with callus.
Ball-tipped guide wire
Once the proximal metaphysis is breached, pass a ball-tipped guide wire down the medullary canal into the distal metaphysis. This requires fracture reduction. If reduction is difficult or the fracture is comminuted, special efforts may be required.
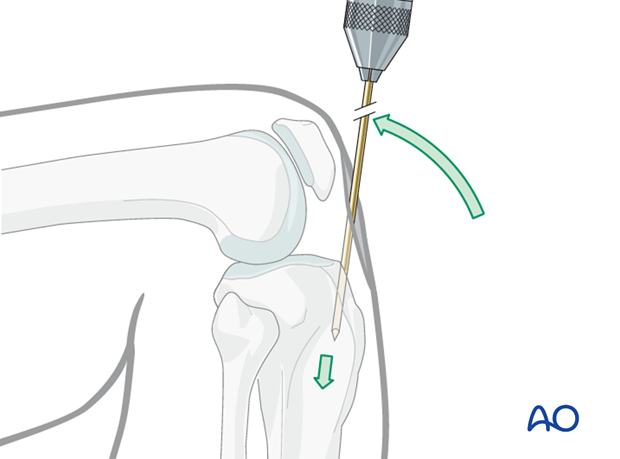
Bending the guide wire
Slightly bending the guide wire 10-15 mm above its tip is helpful for two reasons:
- Passing through the fracture site into the distal fragment is easier, since rotation of the guide wire redirects its tip.
- It also facilitates the proper position of the tip in the distal metaphysis.
A guide wire like the one illustrated, with its ball a little proximal to the end, allows the bend to be placed beyond the ball, so that it cannot jam inside a cannulated reamer.
Fluoroscopic control
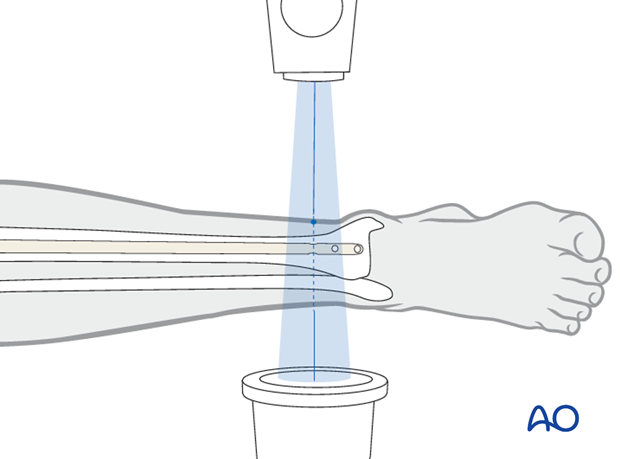
Use fluoroscopy to check that the guide wire is positioned above the centre of the ankle joint.
6. Determination of nail length
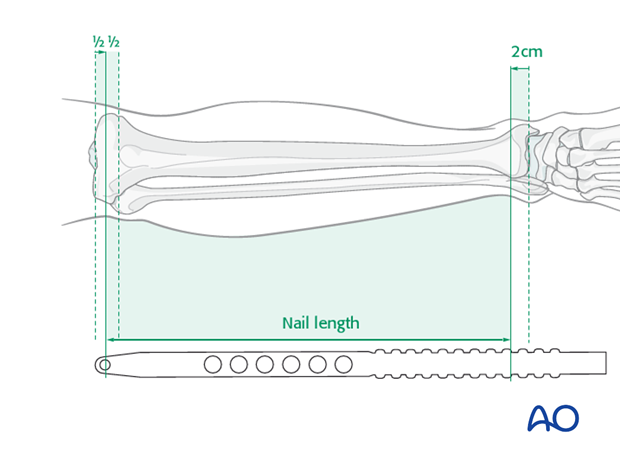
Nail length
Nail length is estimated preoperatively, but intraoperative measurement is more precise. Use a radiographic ruler, provided with the nail’s instruments. With the fracture reduced, measure the distance from the planned nail entry site to just above the ankle joint.
Select a nail that extends from the distal tibia to the entry site without protruding above the bone surface. Nail length may be critical for distal fractures. Some nails have proximal extensions of different lengths, that can be added after insertion to correct for an excessively short nail.
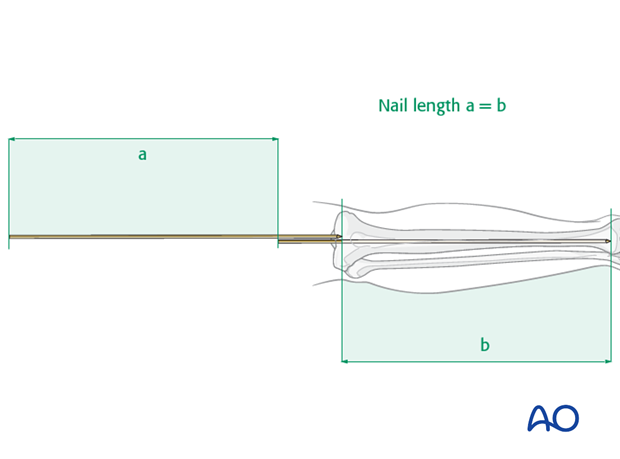
If there is no radiographic ruler and/or image intensifier available, a simple, clinical, intraoperative length measurement is advised. With the intramedullary guide wire in proper position, place a second guide wire of equal length at the entry portal and measure the difference in length between the two wires (a). This difference represents the proper nail length (b), see illustration.
It is always advisable to double-check the measured length by comparison with the contralateral (intact) tibia.
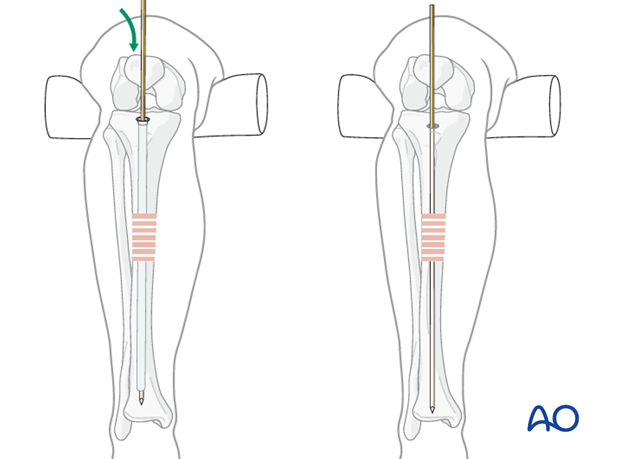
7. Reaming and determination of nail diameter
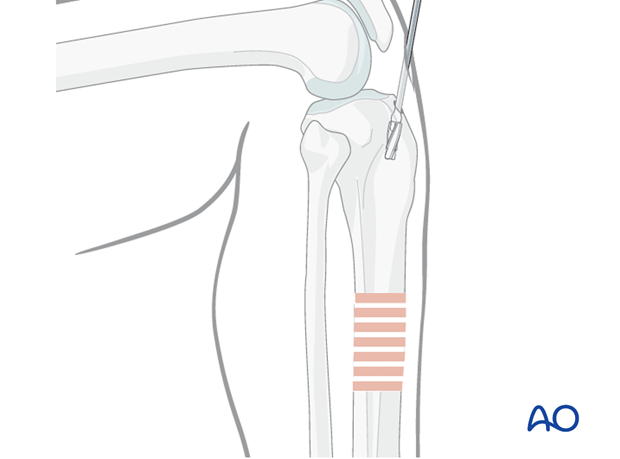
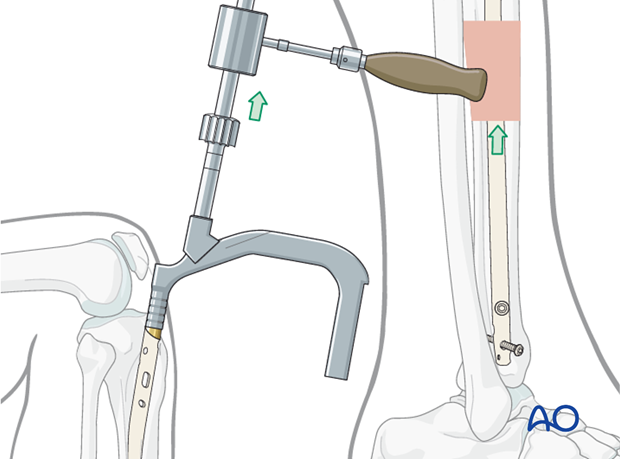
Reaming
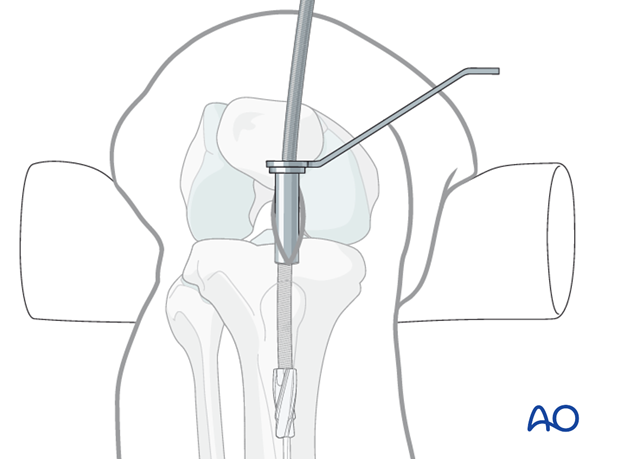
Insert the cannulated, flexible-shaft reamer over the ball-tipped guide wire.
Begin with an end-cutting reamer and proceed sequentially to larger reamer diameters, usually in increments of 0.5 mm. Protect the soft tissues at the entry site during this process with a reamer sleeve, as shown, or suitable retractors.
Do not force the reamer! While advancing, intermittently pull back a little to clear debris from the medullary canal.
A chattering sensation indicates that the reamer is in contact with the internal cortical surface. A millimeter or two of additional reaming usually permits passage of an appropriate diameter nail.
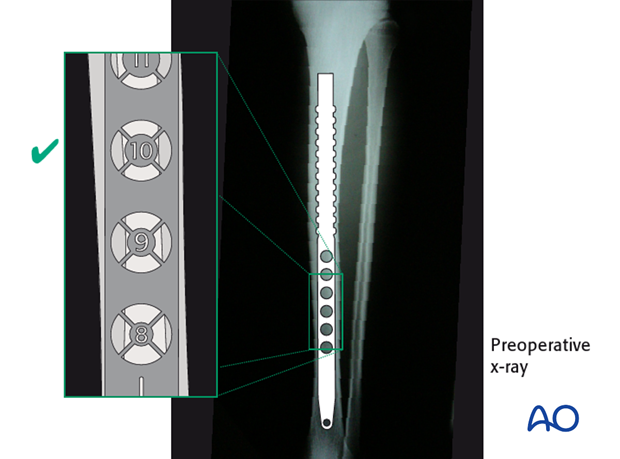
Choosing nail diameter
A radiographic gauge, as illustrated, helps assess the medullary canal diameter. Check both AP lateral views.
The nail diameter should be large enough to provide sufficient strength and durability of both nail and locking screws. Consult the nail manufacturer’s instructions. Usually a 10 mm nail is sufficient. Reaming should be to 0.5 to 1.5 mm greater than nail diameter, since the medullary canal is not perfectly straight.
Preparing for nail insertion
Cannulated nails are inserted over appropriate guide wires. No guide wire is used for a solid nail. The ball-tipped, or significantly bent, guide wire used for reaming may be too big to remove through a given cannulated nail. If so, the wire must be replaced before the nail is inserted. A plastic medullary exchange tube is available for exchanging guide wires. Pass the medullary tube over the reaming guide wire and all the way passed the fracture site. Hold it in place while removing the reaming guide wire.
Insert the nailing wire through the tube, and confirm that it is properly positioned in the distal tibia (AP and lateral x-rays). Then remove the medullary exchange tube.
8. Insertion of the cannulated nail
Nail insertion
With adequate reduction and sufficient over-reaming, it should be possible to insert the cannulated nail over the guide wire by hand, or with gentle hammering. Ensure that reduction is maintained as the nail crosses the fracture. If insertion is difficult, correct the reduction and/or remove the nail and ream to a larger diameter.
Make sure that the proximal end of the nail is below the surface of the bone at the entry site, to decrease the risk of knee pain. Careful choice of nail length may be necessary, particularly for distal fractures, to ensure both distal fixation and proper length proximally.
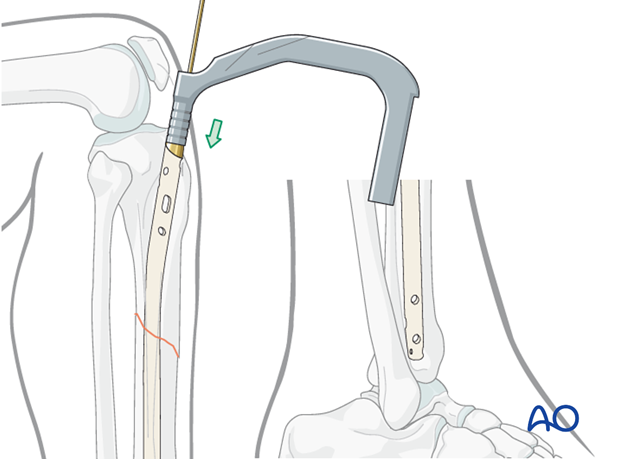
The tip of the nail should be placed in the center of the distal tibia, approximately at the level of the physeal scar (denser bone). Distal placement of the nail is particularly important for fractures below the medullary isthmus. Proper fracture alignment must be maintained by the surgeon, since at this level, passage of the nail does not reduce the fracture.
Pitfalls
The nail should advance into the medullary canal with each tap of the hammer. If resistance is encountered, it may be caused by the wrong entry point, or the tip of the nail hitting the cortex of the distal fragment.
Forced hammering may cause fracture comminution, nail incarceration, or twisting of the nail.
9. Locking of the nail
Proximal locking or distal locking first?
If the length is correct, proximal locking screws are inserted first, and then the insertion handle is removed.
The knee is then extended and the distal locking is performed, with fluoroscopic guidance using instrumentation and technique chosen by the surgeon.
If the fracture is distracted, distal locking is performed first with 2–3 screws, and the nail is pulled back with gentle hammer blows until fracture contact is achieved (see “Backslap technique”). Recheck the proximal end of the nail, which should not protrude proximally.
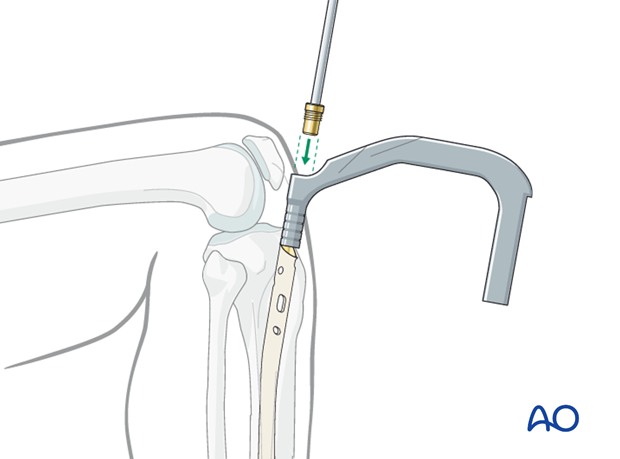
Proximal locking
Aiming guides for proximal locking screws are a standard part of intramedullary nailing instruments. These are used as intended.
With proximal fractures, multiple locking screws may be required for adequate stability. Their choice usually depends upon the fracture pattern. For diaphyseal fractures, a single locking screw may be sufficient, if the fracture is length-stable. (Use of an oval (“dynamic”) hole will permit fracture impaction while controlling rotation.) If the fracture is length-unstable, two proximal locking screws should be used, for better maintenance of length.
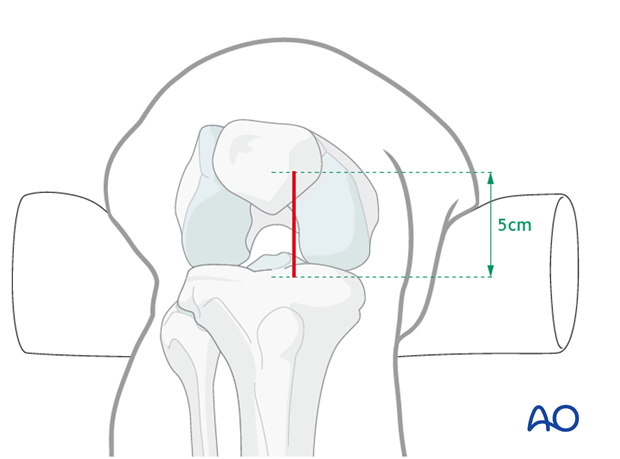
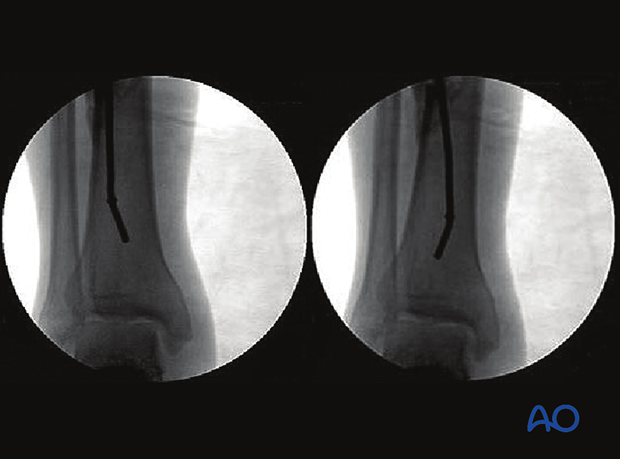
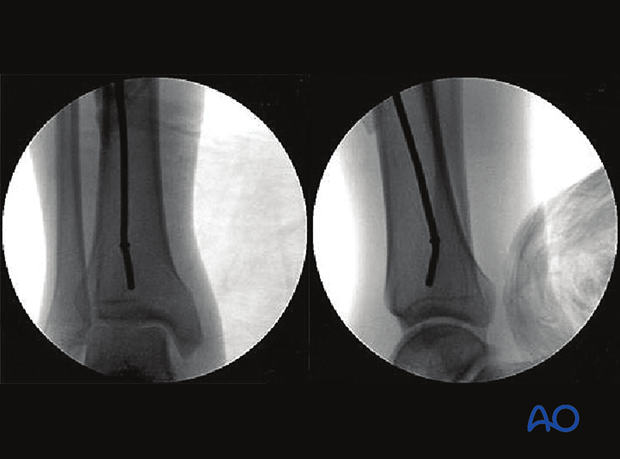
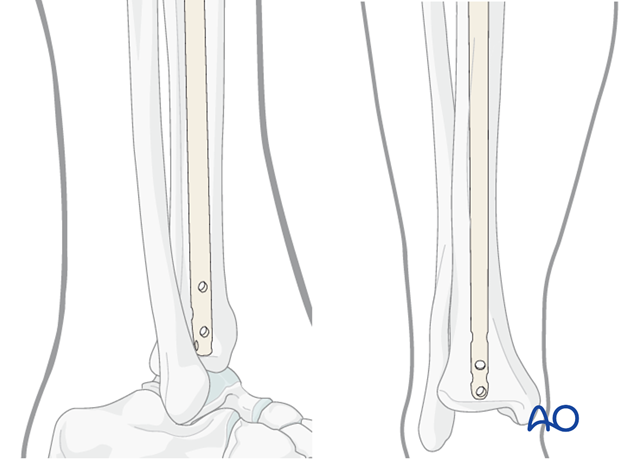
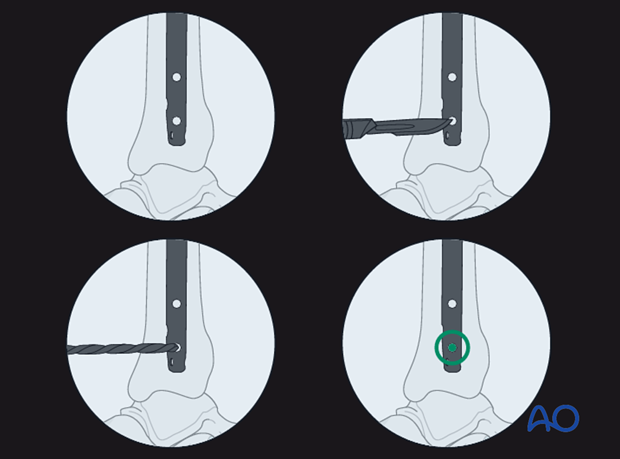
Distal interlocking with fluoroscopic guidance
The leg must be positioned so that precise images can be obtained. The central ray of the fluoroscope must pass through the locking hole so that its image is perfectly round, and centered on the display screen. This confirms that the central ray is perpendicular to the nail.
The leg is elevated on folded linen or other material, and carefully supported to maintain the desired reduction (length, rotation and angulation). The C-arm is positioned to permit imaging while the entry site is located and drilled. Leave enough room for instruments between the image source and the patient’s leg.
Distal locking
With the leg and fluoroscope properly positioned, an incision is made with radiographic guidance over the selected locking hole. Soft tissues are bluntly spread, and the drill is positioned over the locking hole (in line with the fluoroscopic central ray). The drill is then advanced through the near tibial cortex, the locking holes in the nail, and the far tibial cortex. Its position is confirmed radiographically. If correct, screw length is measured, the appropriate screw is inserted, and its proper placement is confirmed radiographically. Details of this procedure may vary somewhat according to surgeon’s experience and available equipment (e.g. radiolucent drill, hand awl, etc).
Typically, two distal locking screws are used for diaphyseal or proximal fractures, though if the pattern is length-stable, a single screw may be sufficient. Particularly for distal fractures, multiple screws including AP and/or oblique orientation may be necessary to provide stability. Repeat the above insertion technique as necessary for each screw.
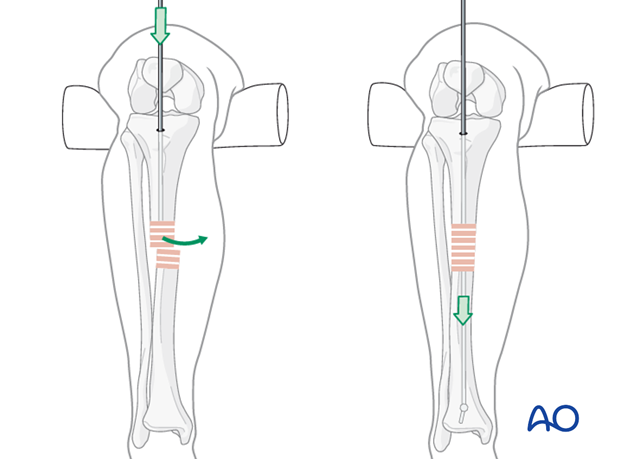
Backslap technique for correction of fragment diastasis
Fracture distraction interferes with healing, and must be eliminated. Distraction may be corrected by locking the nail distally, and then “backslapping” the nail with the appropriate instrumentation. The distal locking screws must be inserted first. Carefully hammer the nail, as if removing it, under fluoroscopic control until fracture contact and desired length are achieved.
10. Nail capping and wound closure
Insertion of an end cap
Remove the insertion handle and its connecting screw.
Insert an end cap, if desired, to prevent ingrowth of bony tissue, which will interfere with nail removal.
End caps of different lengths may be available to increase the overall length of the nail, if necessary, after final positioning of nail for distal fracture. Make sure that the proximal end of the end cap does not protrude above the tibial surface.
Radiographic guidance may help orient the end cap and make insertion easier.
Pearl: Using the 0 mm end cap
With the AO expert tibial nail, the 0 mm end cap (the end cap which fits completely within the nail) may be inserted through the insertion handle. To do this, the connection screw has to be removed carefully without moving the insertion handle. The end cap can then be passed through the channel of the insertion handle. This is not possible for longer end caps as they are of a larger size.
Wound closure
Repair the patellar tendon and its paratenon with interrupted sutures, if they have been incised. Skin and subcutaneous tissue are closed with a few loose sutures, which should be left in until the wound is securely healed. Apply a soft dressing that will permit knee motion.
11. Aftercare
Immediate postoperative care
Immediately after surgery, while the patient is still in the hospital, emphasis is given to
- Pain control
- Mobilization
- Infection and deep veinous thrombosis (DVT) prophylaxis
- Early recognition of complications
Compartment syndrome occasionally develops after IM nailing. During the first day after nailing, sensation and strength should be followed carefully. Increasing pain may be a warning sign.
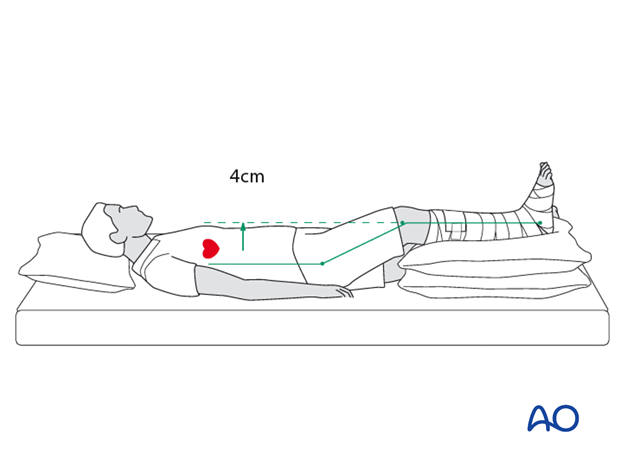
The patient’s leg should be slightly elevated, with the leg placed on a pillow, approximately 4 cm above the level of the heart. This maintains perfusion while helping to avoid swelling.
Soft-tissue protection
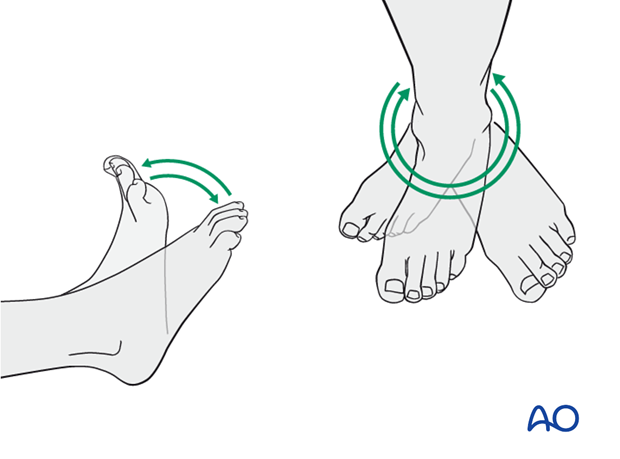
A brief period of splintage may be beneficial for protection of the soft tissues, but should last no longer than 1–2 weeks. Thereafter, mobilization of the ankle and subtalar joints should be encouraged.
Mobilization
Encourage active motion of all joints (hip, knee, ankle, and toes). Gentle, progressive stretching to achieve knee extension and ankle / foot dorsiflexion begins as soon as tolerated.
Weight bearing
Partial weight bearing with crutches is started as soon as the patient is able. Unrestricted weight bearing should be delayed until fracture callus is visible, fibular healing is evident, and weight bearing is without pain.
Follow up
Clinical and radiological follow-up is recommended after 2, 6 and 12 weeks. Depending on the consolidation, weight bearing can usually be increased after 6–8 weeks, with full weight bearing when the fracture has healed.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implants. The best time for nail removal is after complete remodeling, usually at least 12 months after surgery.
Locking screws may need to be removed sooner if they are prominent and/or painful. Once callus is evident, such screws are usually unnecessary, but individual assessment is necessary to avoid premature screw removal, with late loss of fracture alignment.
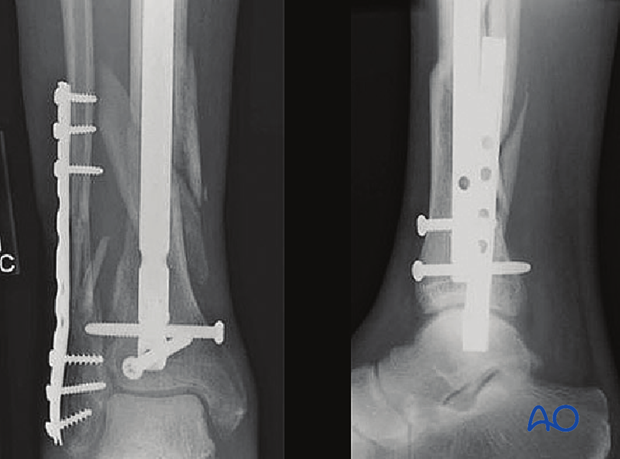
In this case, 12 weeks after nailing the fibula was bridge-plated for additional stability.