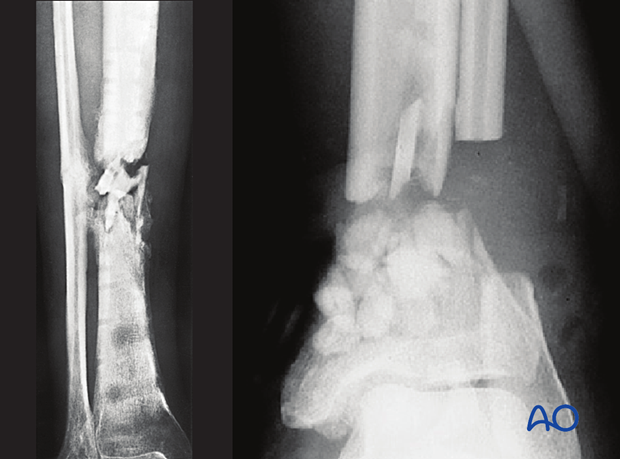
Recurrent osteomyelitis
Fracture-site infections may be intermittent, with periods of symptomatic inflammation (pain, redness, swelling and perhaps development of an open wound). They may recur after many years of quiescence.
Such patients need thorough assessment and treatment planning. If the fracture is satisfactorily united, and the patient is functional, the primary goal is to heal the infection. Recurrence is usually due to a persisting collection of bacteria, typically around fixation hardware, or necrotic bone. A necrotic fragment (sequestrum) may lie adjacent to, or within, the previously fractured bone. If hardware is present, its removal is almost always an essential part of treating the infection. A sequestrum may be hidden under a retained plate or be hard to find because it is adjacent to an intramedullary nail. If a sinus tract is present, it typically leads to the source of recurrent infection and offers a guide to debridement. Cross-sectional imaging (CT, or MRI) helps in locating sequestra and necrotic bone. This may be most helpful after hardware removal.
Surgical cultures of the infected tissues are essential for correct identification of the responsible bacteria and appropriate definitive choice of antibiotics.
Occasionally, an early recurrent infection can be successfully treated with prompt antibiotic treatment based on the results of cultures from previous recurrences. A trial of antibiotics should be considered, if a patient presents in the early stages of recurrence, prior to wound breakdown.
If the infected fracture has not united, symptoms of nonunion (pain, instability, impaired weight bearing, and deformity) will usually be evident. In such a situation, definitive treatment requires that the nonunion be addressed after hardware removal and debridement of necrotic bone.













