Delayed presentation of infection
Some fracture wound infections present more than two weeks after fracture surgery. Often, there are atypical systemic or local symptoms (mild fever, or less erythema). Ultimately, increasing pain, redness, and swelling, etc., become evident. Sometimes, late onset of wound breakdown or drainage (formation of a sinus tract) is the first indication that an indolent infection is present.

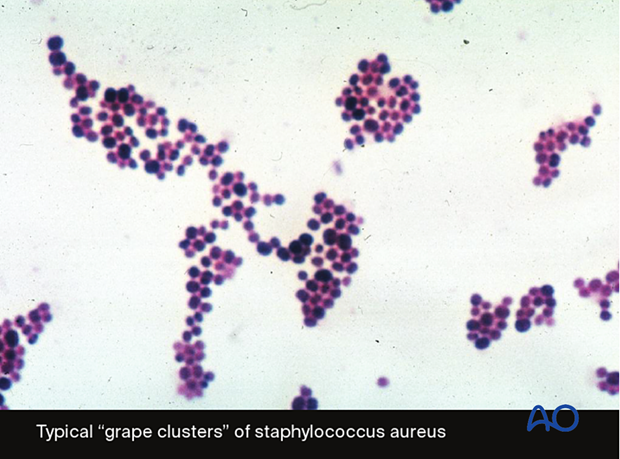
The microorganisms that cause delayed infection are usually of lower virulence (eg, coagulase-negative staphylococci). Infecting bacteria have often been present long enough to have become adherent to metallic implants and dead bone and are thus more resistant to antibiotics. Thorough surgical debridement is required and provides an important opportunity for fracture-wound evaluation. Nonviable bone and soft tissue require debridement. Hardware may need to be removed if loose. If hardware still provides stable fixation, an attempt may be made to leave it in place and suppress the infection with antibiotics until the fracture has healed.
If more extensive debridement, including substantial bone removal, is required, or the internal fixation construct needs to be removed, treatment may require temporary external fixation, nailing, or plating with more involved bone and/or soft-tissue reconstruction. In all instances, appropriate vascularized soft-tissue reconstruction will be necessary to cover the affected area.