Minimally invasive lateral approach to the tibial shaft
1. Indications
The lateral approach is used for minimally invasive osteosynthesis if the medial soft tissues are injured.
This approach is also used when a precontoured plate (eg, a locking compression plate) is placed laterally for fixation of proximal and mid-tibial fractures.
Distally, the shape of the tibia and the overlying soft tissues make it difficult to contour a plate and place screws.
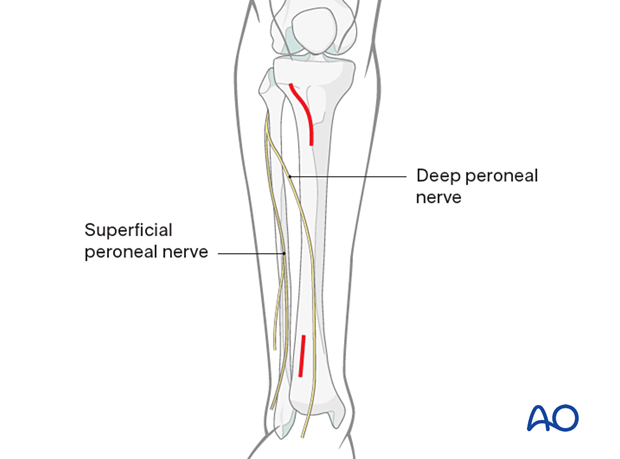
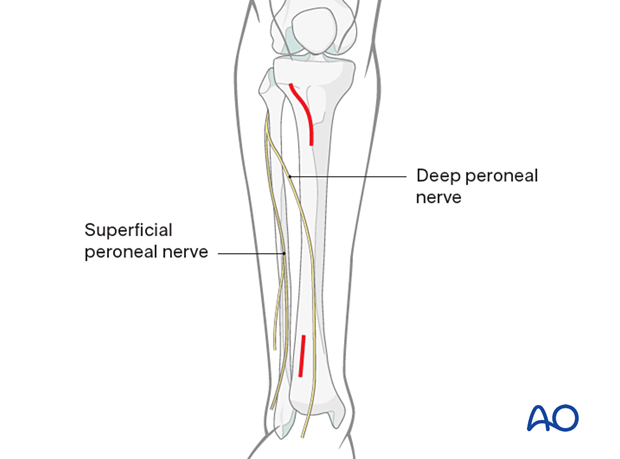
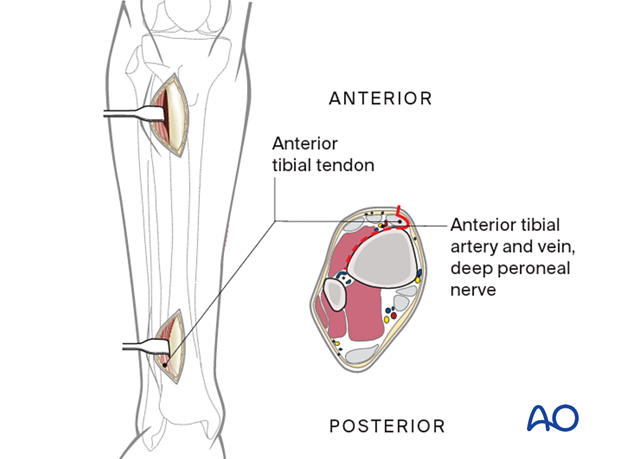
Over the distal third of the tibia (for plates longer than approximately 25 cm), a short incision is advisable in this region to expose and retract the deep peroneal nerve and anterior tibial vessels to avoid their being trapped by a submuscular plate or being injured by percutaneously placed screws.
2. Anatomy
The lateral and posterior surfaces of the tibia are covered by muscle. The anteromedial surface has only a thin layer of subcutaneous tissue and skin. This surface provides less blood supply to the underlying bone.
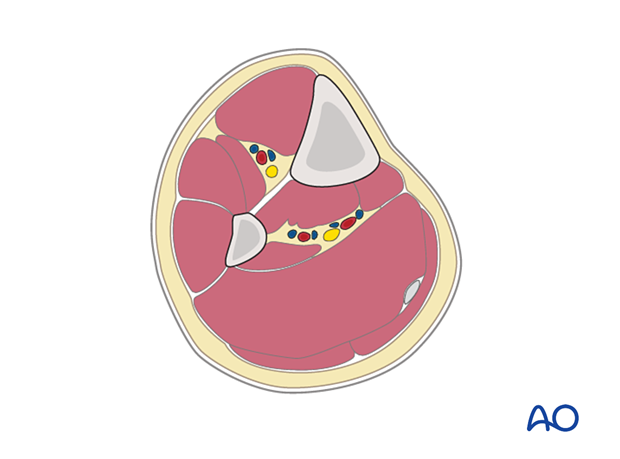
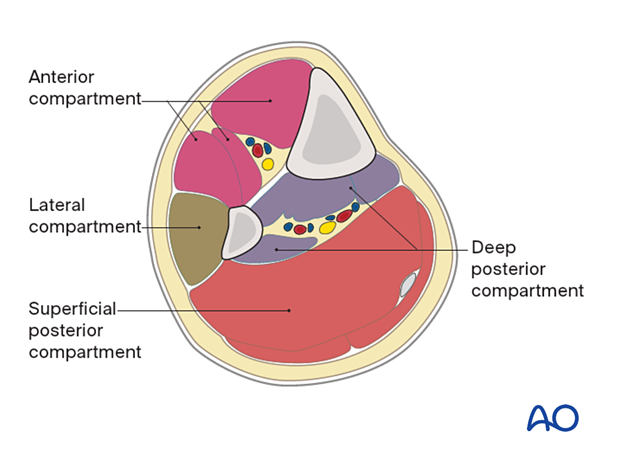
The lower leg has four compartments:
- Anterior
- Lateral
- Deep posterior
- Superficial posterior
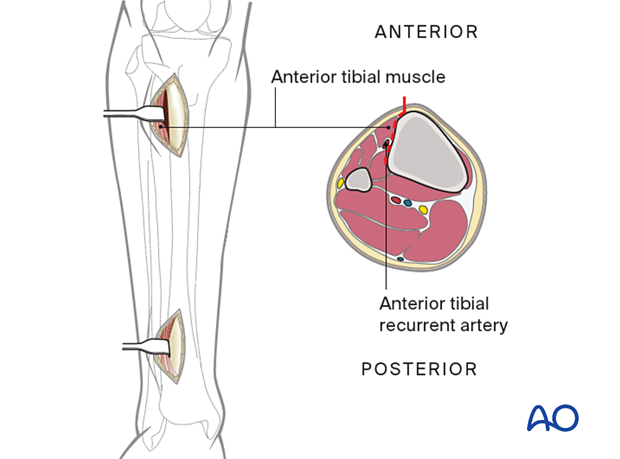
The anterior compartment has three muscles, one main artery, and one nerve: the tibialis anterior, extensor hallucis longus, extensor digitorum longus, the anterior tibial artery, and the deep peroneal nerve.
The lateral compartment has two muscles and one nerve: the peroneus longus and brevis, and the superficial peroneal nerve.
The deep posterior compartment has three muscles, two arteries, and one nerve: the tibialis posterior, flexor hallucis longus and flexor digitorum longus, and the peroneal and posterior tibial arteries, as well as the tibial nerve.
The superficial posterior compartment has two muscles and one nerve: the gastrocnemius, the soleus, and the sural nerve.
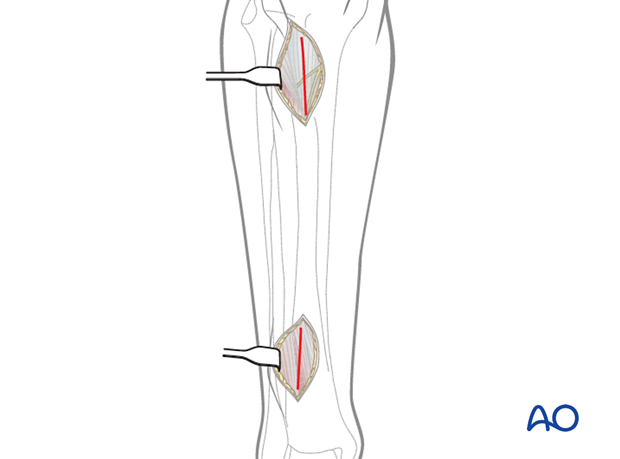
3. Skin incisions
The proximal incision, approximately 5 cm long, begins distal to the tibial tubercle and 1.5–2 cm lateral to the tibial crest. The proximal portion should curve slightly posteriorly.
The distal incision is made to prevent neurovascular injury from percutaneously placed screws. The anterior tibial vessels and deep peroneal nerve cross the anterolateral surface of the tibia approximately at the junction of its third and fourth quarter.
4. Deep dissection
Incise the fascia a few millimeters lateral to the tibial crest.
At the distal incision, dissect the anterior tibial tendon from the bone, preserving the paratenon.
Retract the tendon together with the deep peroneal nerve and the anterior tibial vessels to the lateral side.
At the proximal incision, dissect the anterior tibial muscle from the bone without stripping the periosteum.
Retract the anterior tibial muscle laterally.
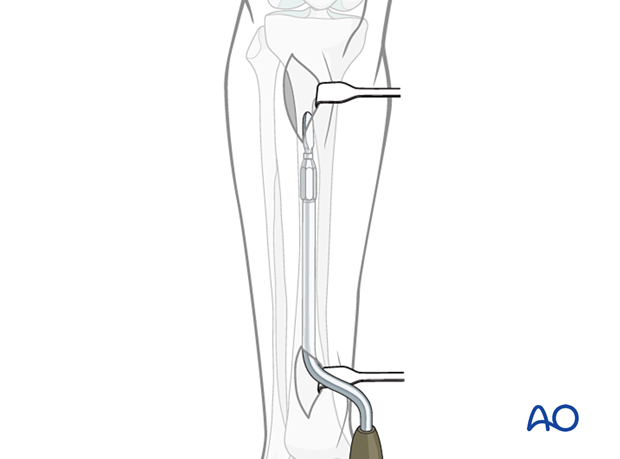
Use a soft-tissue elevator, a tunneler, as shown, or a plate to prepare a tunnel between the anterior tibial muscle and the periosteum.
Protect the anterior tibial vessels and deep peroneal nerve distally. Depending on how distal the plate is placed, they should be gently retracted laterally or lifted anterolaterally so that the instruments or plate can be placed under the neurovascular bundle, with direct observation.
5. Wound closure
Skin and subcutaneous tissues should be closed. Consideration of closing the fascia should be made carefully as there is always the risk of compartment syndrome developing postoperatively.













