Approach to the posterolateral surface of the tibia
1. Indications
The posterolateral approach can be used for open plate fixation of the tibia on its posterior surface. This may be necessary when the anterior soft tissues are compromised.
The posterior surface of the tibia is relatively flat and therefore little contouring of the plate is necessary.
This approach is often also utilized for treatment of non-unions with posterolateral bone grafting. It allows access to both the tibia and fibula.
It is a more challenging approach requiring a good understanding of the surgical anatomy.
2. Positioning
The patient may be positioned either lateral or prone. Since the fibula lies more posteriorly than the tibia, a prone position greatly facilitates exposure.
A tourniquet helps to minimize venous bleeding, which may become significant. Place it high on the thigh, after the patient is positioned. Inflation is optional.
3. Anatomy
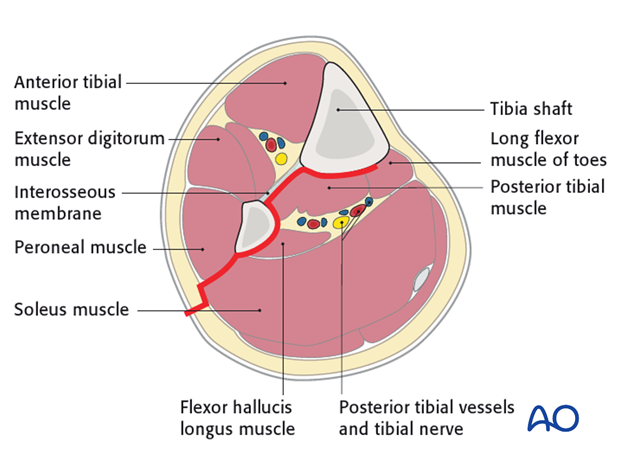
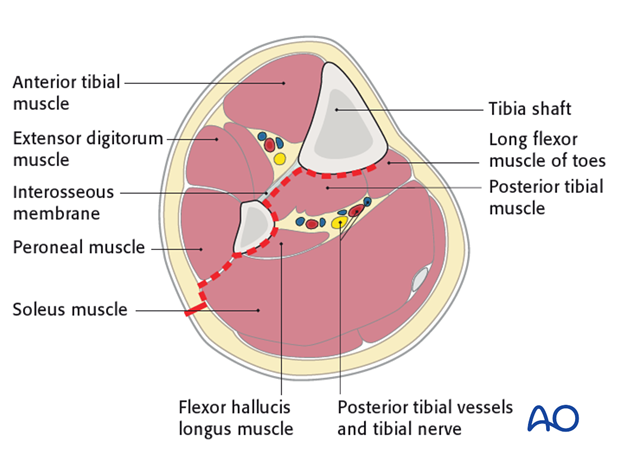
Triangular shape of the tibia
The lateral and posterior surfaces of the tibia are covered by muscle. The anteromedial surface has only a thin layer of subcutaneous tissue and skin. This surface provides less blood supply to the underlying bone.
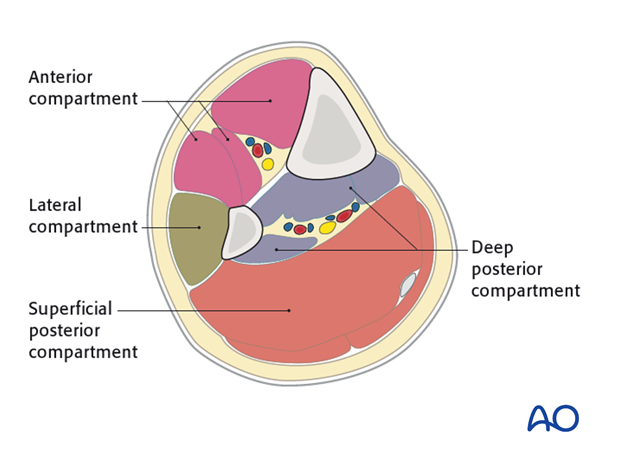
The lower leg has four compartments:
- Anterior
- Lateral
- Deep posterior
- Superficial posterior
The anterior compartment has three muscles and one main artery and nerve: Tibialis anterior, extensor hallucis longus, extensor digitorum longus; the anterior tibial artery and deep peroneal nerve.
The lateral compartment has two muscles and one nerve. The muscles are the peroneus longus and brevis and the superficial peroneal nerve.
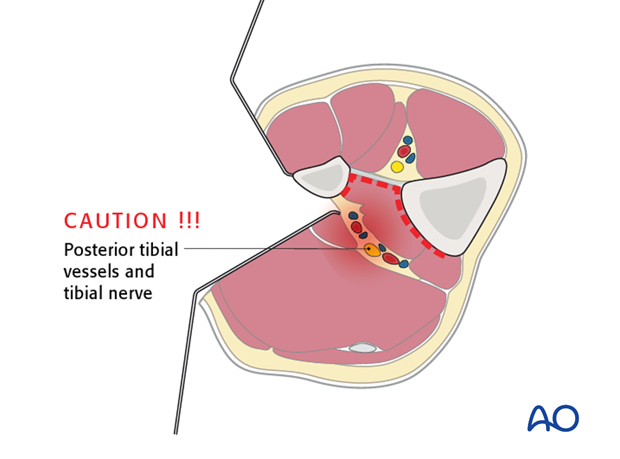
The deep posterior compartment has three muscles and two arteries and one nerve: The muscles are the tibialis posterior, the flexor hallucis longus and the flexor digitorum longus. It also has the peroneal artery and the posterior tibial artery as well as the tibial nerve.
The superficial posterior compartment has just two muscles in it: The gastrocnemis and soleus muscles and the sural nerve.
4. Skin incision
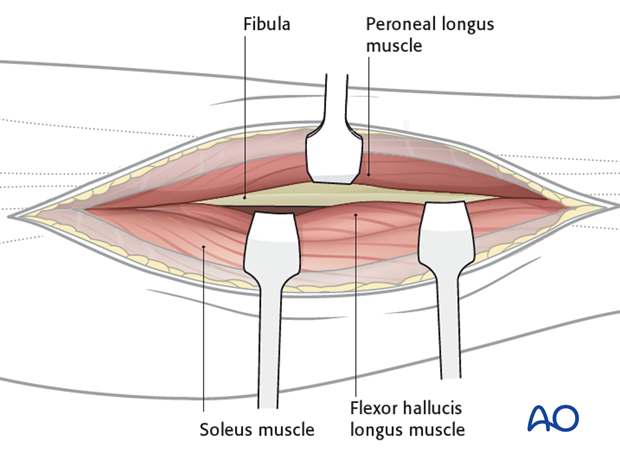
The length of the incision varies, but it should begin over the lateral boarder of the gastrocnemius muscles and extend distally to a point that is midway between the achilles tendon and the fibula.
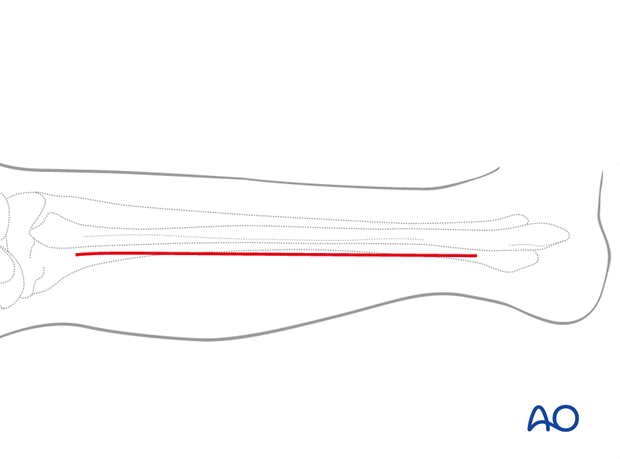
The interval between the lateral and posterior compartments is usually easier to find distally. Further dissection proximally is undertaken as required.
5. Dissection
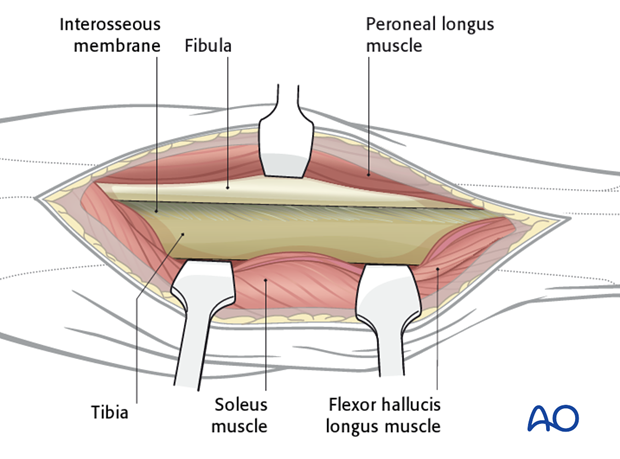
The plane of the dissection will be between the superficial posterior and lateral compartments. The fascia is incised and the gastrocnemius and soleus are mobilized medially leaving the peroneal muscles laterally. In this way, the posterolateral aspect of the fibula is exposed.
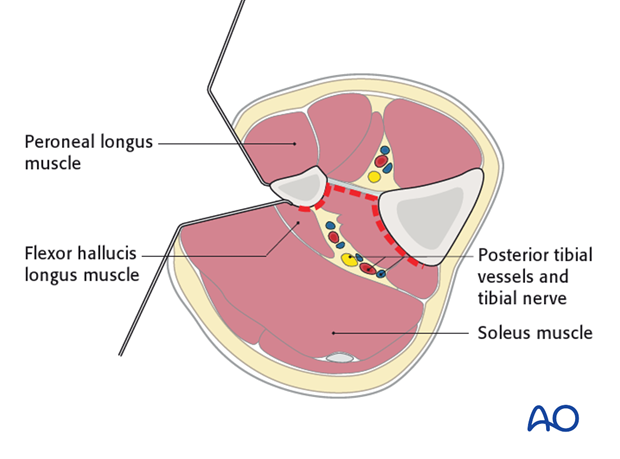
Often there are crossing perforating branches of the peroneal vessels, which must be ligated.
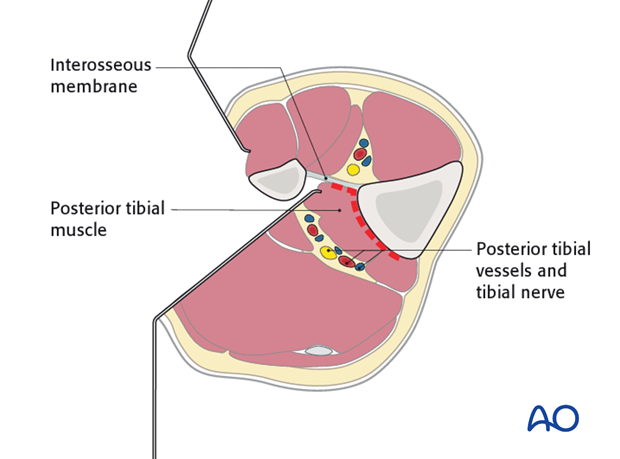
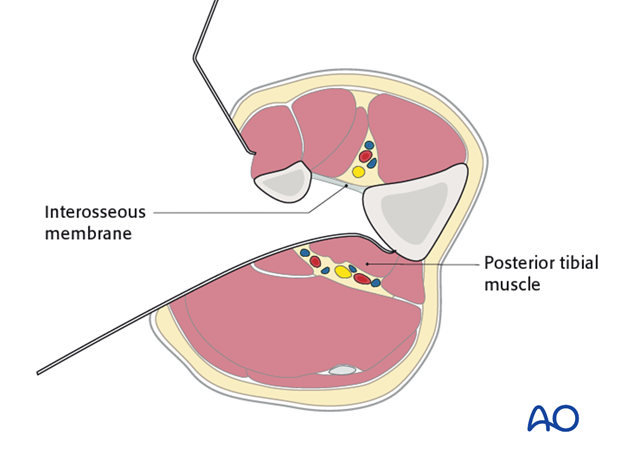
Arising from the posterior aspect of the fibula is the Flexor hallucis longus (FHL), which is mobilized posteromedially. Medial dissection is continued until the interosseus membrane is encountered.
6. Note
One should proceed with caution when mobilizing the deep posterior compartment. It is crucial that the entire compartment is mobilized from the fibula, interosseous membrane and tibia.
Beginning outside the fracture zone, expose the posterior and medial surfaces of the fibula, and follow these to the interosseous membrane. Retract the deep posterior compartment contents from lateral to medial, to protect the neurovascular structures.
With the interosseous membrane identified, mobilize the remainder of the deep posterior compartment medialwards until the posterior aspect of the tibia is encountered. Extend the exposure proximally beyond the fracture as far as necessary for plate fixation.
Be aware of the common peroneal nerve crossing the fibular neck very proximally.
At the conclusion of the dissection the surgeon should have access to the posterior aspects of both the tibia and the fibula.
7. Pearl:
The posterior dissection is often difficult in the zone of injury, so often it is best to begin the dissection outside of this zone, where the anatomy is more normal.
8. Wound closure
A drain should be placed in the deep zone of the dissection to prevent postoperative hematoma formation. While the fascia may be closed between the superficial posterior and lateral compartments, swelling and compartment syndrome are definite risks.
If there is any concern about a developing compartment syndrome, the fascia should be left open and only the skin and subcutaneous layers are closed.













