Lag screw fixation
1. Principles
Fracture plane
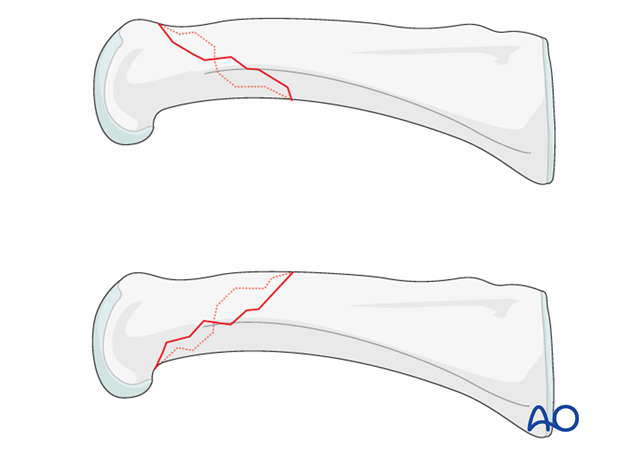
Long oblique/spiral fractures can occur with the obliquity visible either in an AP view, or a lateral view.
Treatment differs somewhat depending upon the direction of the fracture plane.
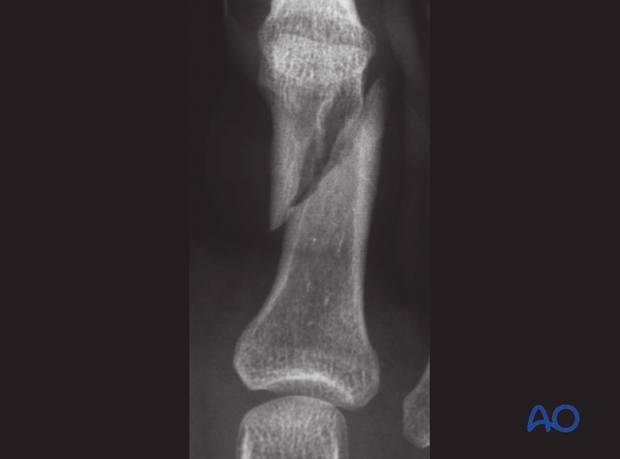
Fracture visible on AP view
A lateral approach is used.
Fracture visible on lateral view
A dorsal approach is used.
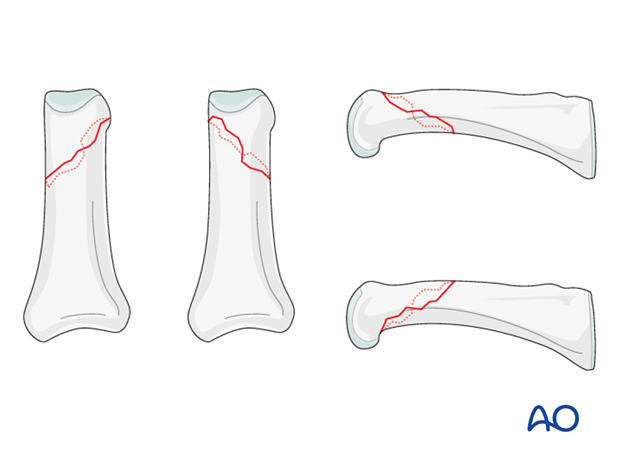
Fracture length
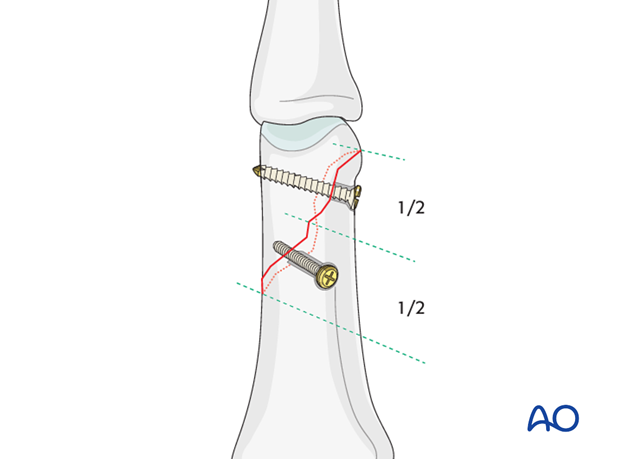
These frequent fractures are usually best treated with lag screws. A minimum of two screws must be used which necessitates that the fracture length is at least twice the diameter of the phalangeal bone. In case of a shorter fracture line, a single lag screw and a protection plate must be used.
A good rule is the following:
The fracture line (B) should be at least twice the length of the diameter of the phalangeal diaphysis (A), i.e. B >= 2A.

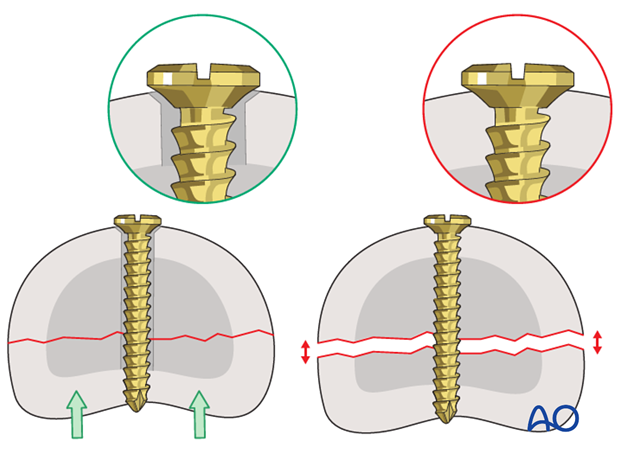
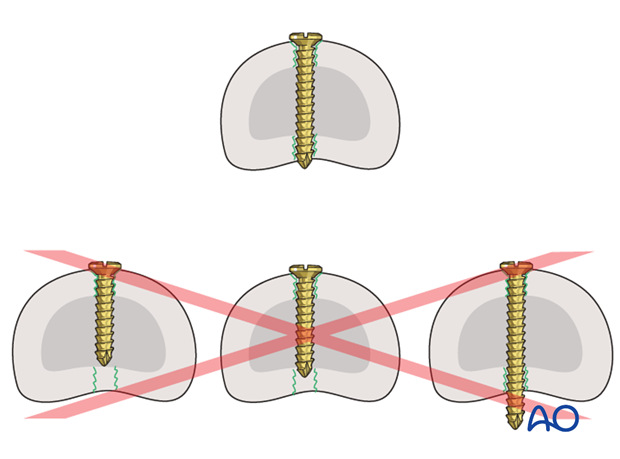
Use lag screws
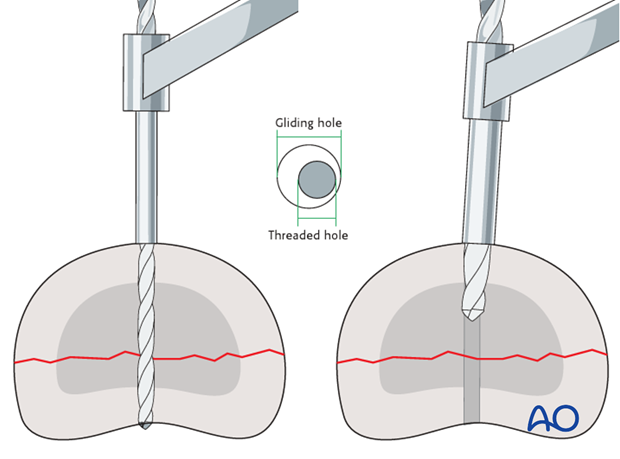
Be sure to insert the screw as a lag screw, with a gliding hole in the near (cis) cortex, and a threaded hole in the far (trans) cortex.
Inserting a screw, across a fracture plane, that is threaded in both cortices (position screw) will hold the fragments apart and apply no interfragmentary compression.
2. Reduction
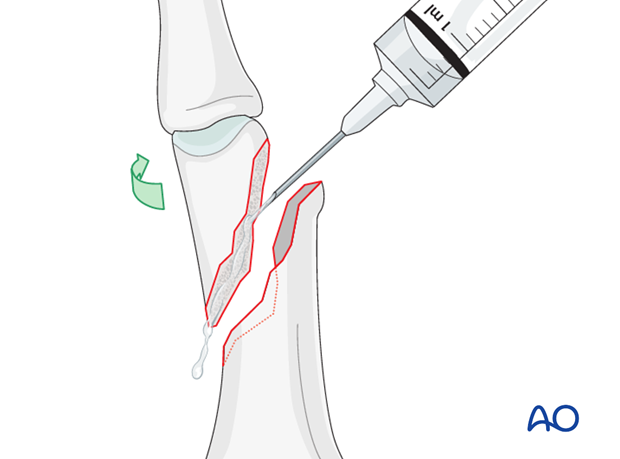
Visualization of the fracture
To determine the exact geometry of the fracture and correct placement of the screws, it may be helpful to open the fracture plane by exerting traction and rotation on the finger.
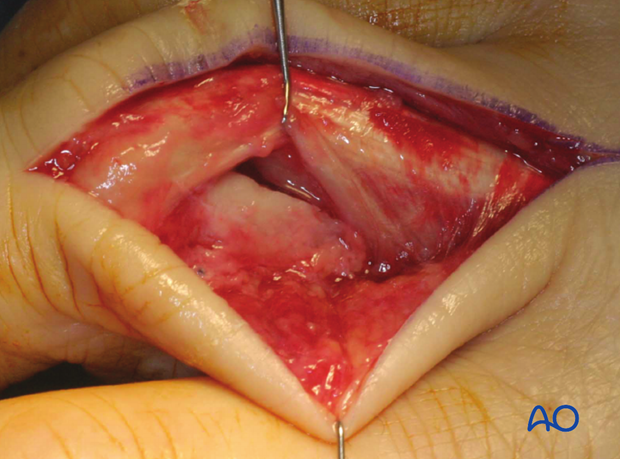
The fracture may be cleared of interposed soft tissues; if necessary, the fracture site can be irrigated for better visualization.
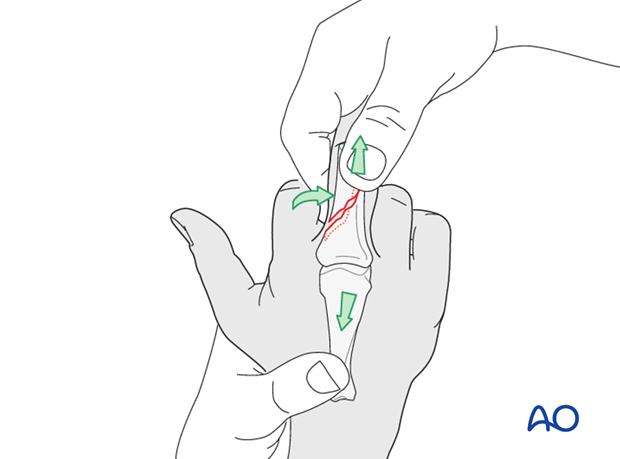
Reduction by traction
Traction is exerted by an assistant while the surgeon reduces the fracture using pressure from a periosteal elevator, or a dental pick.
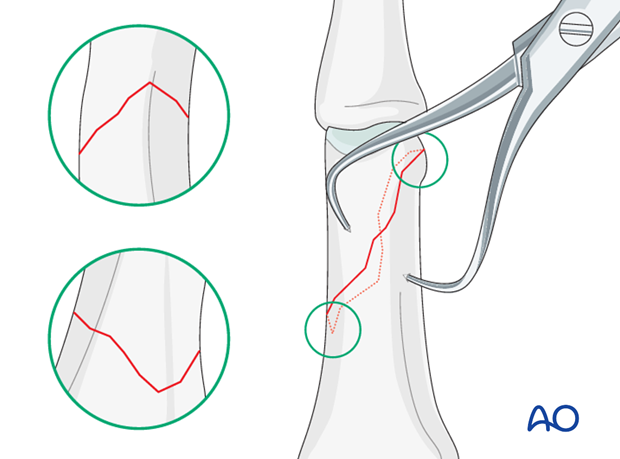
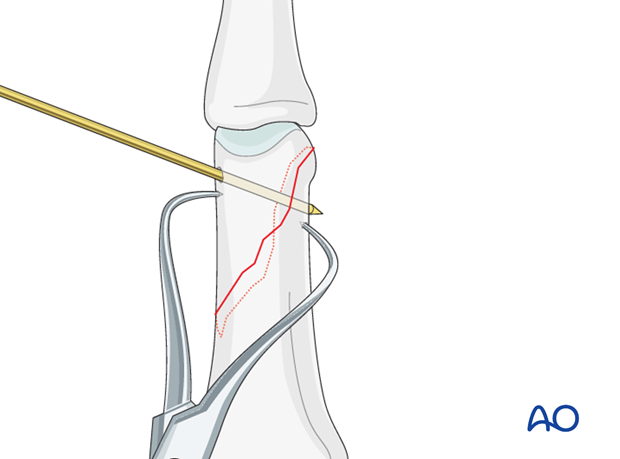
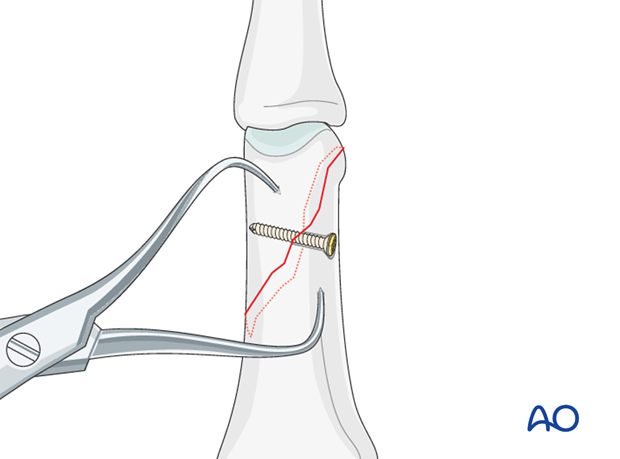
Direct reduction
Secure the reduction with one or two pointed reduction forceps, and confirm using image intensification. Make sure that the reduction forceps does not conflict with the planned screw positions.
It is mandatory to confirm that the apex of each fracture fragment has been anatomically reduced.
Provisional fixation
A temporary K-wire may also be used for provisional fixation.
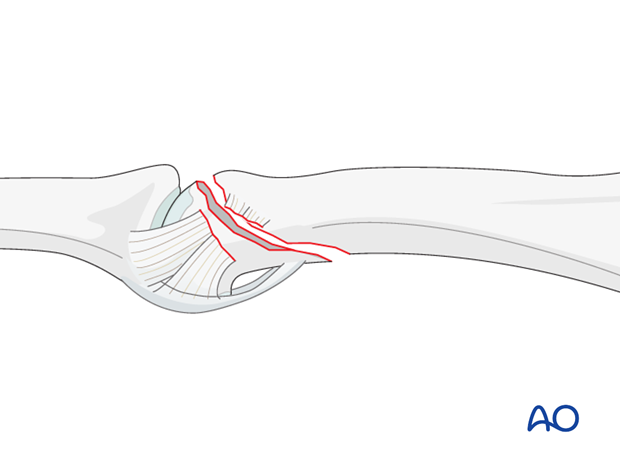
Detachment of collateral ligament
In some cases the fracture line extends to the insertion of the collateral ligament, detaching it.
If this be the case, the collateral ligament must be reattached after the fixation is completed. A tension absorbing suture or an anchoring suture can be used for this purpose.
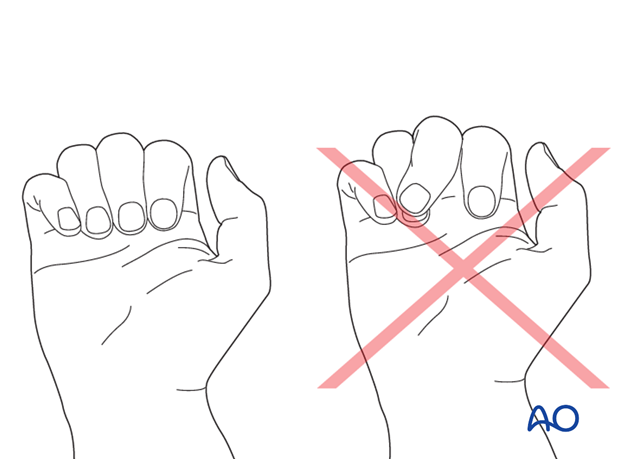
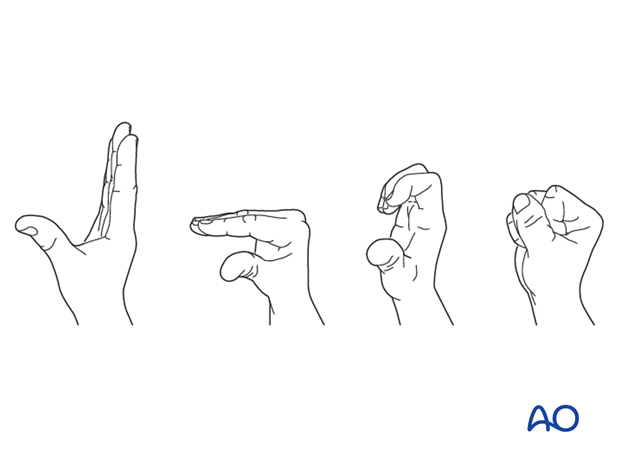
3. Check alignment
At this stage, after provisional fixation, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the fingers.
Under general anesthesia, the tenodesis effect is used, the surgeon fully flexing the wrist to produce extension of the fingers, and fully extending the wrist to cause flexion of the fingers.
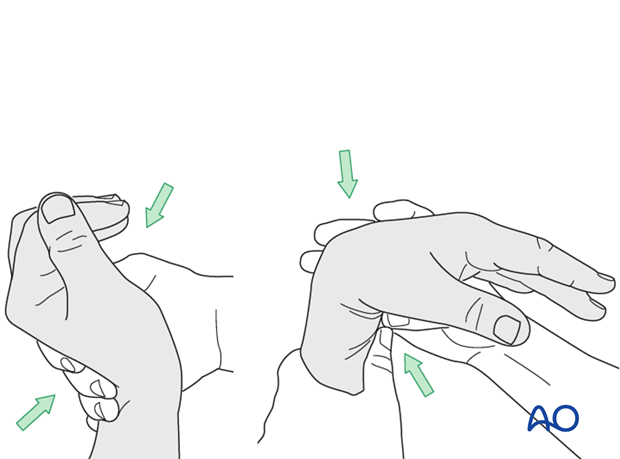
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
4. Planning
Plan correct screw placement
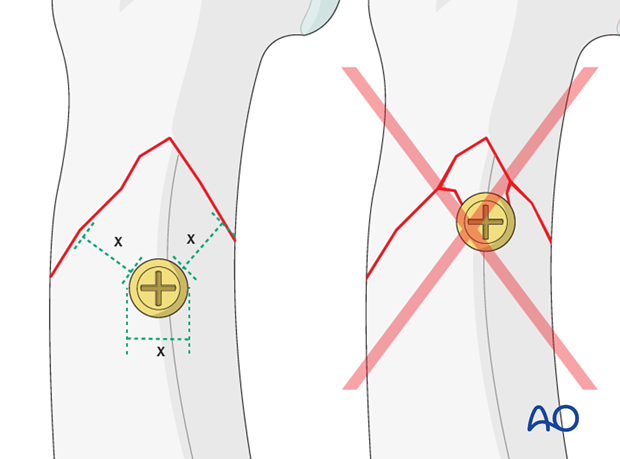
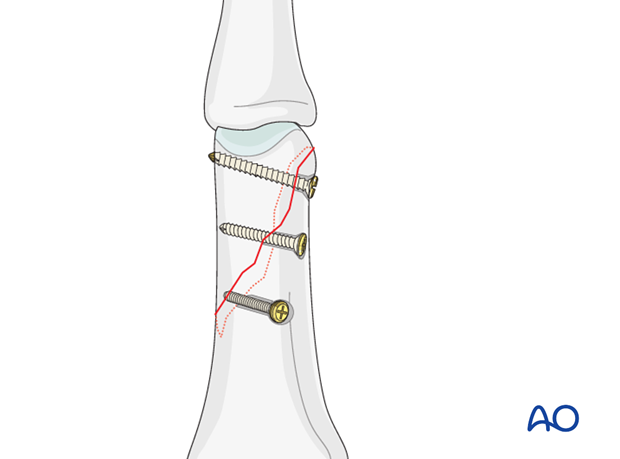
Lag screws should be inserted perpendicularly to the fracture plane, otherwise, screw tightening may lead to fracture displacement.
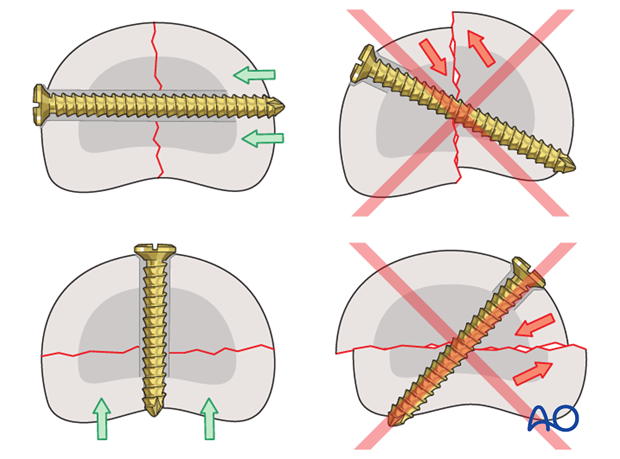
Each lag screw must be inserted perpendicularly to the fracture plane.
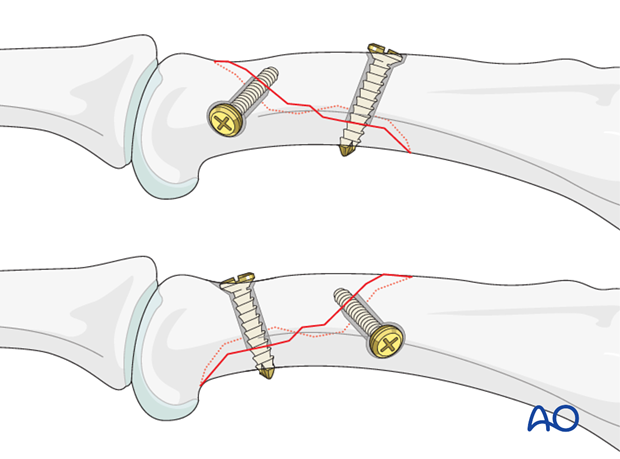
In spiral fractures, the result is that the screws follow a helical disposition.
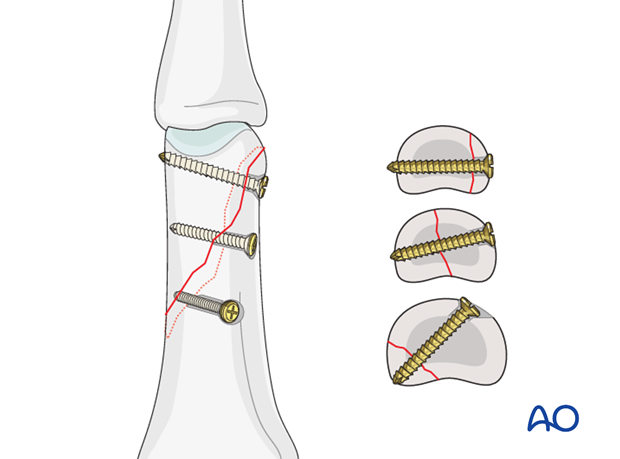
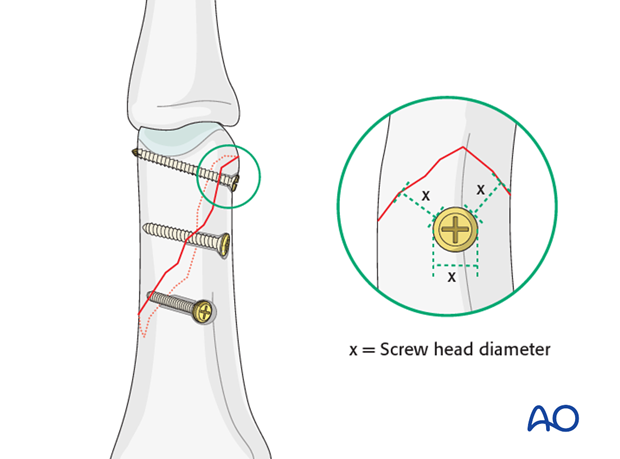
Screw location
If possible, 3 lag screws should be inserted. Generally, they should be inserted at equal intervals.
In general, 1.5 mm screws are used for internal fixation of phalangeal fractures.
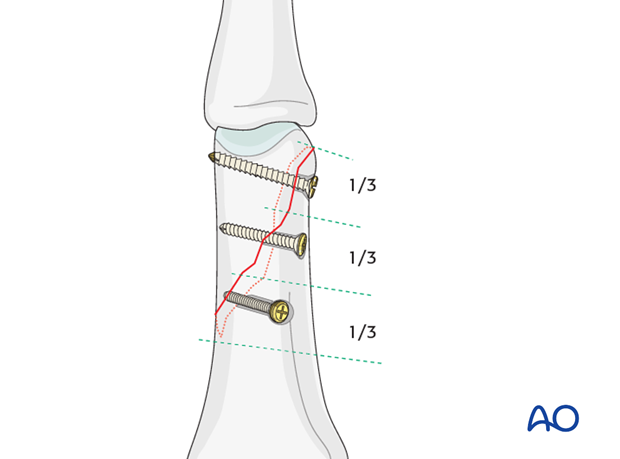
2 screws in shorter fragment
If the fragment is too short to allow for the insertion of 3 screws, use 2 screws, but recognize that this is a less stable construct. If in doubt, add a protection plate.
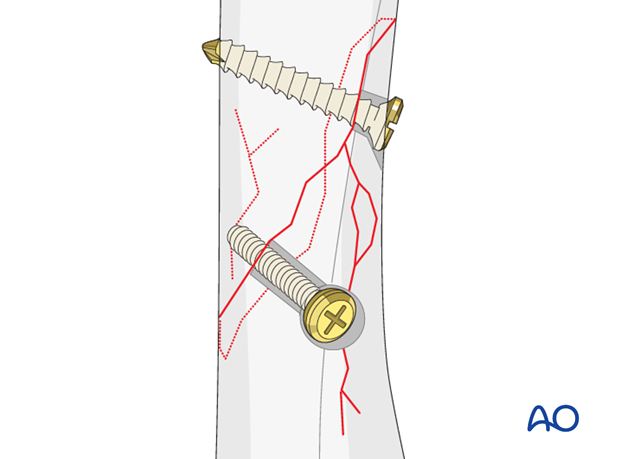
Pitfall: Beware of fissure lines
Often there are short fissure lines that are not apparent on the x-rays. Check for these under direct vision and make sure that the screws are not inserted through these fissure lines.

Pitfall: Screw too close to fracture
Do not insert screws too close to the fracture apex. A minimal distance from the fracture line, equal to the screw head diameter, must be observed.
5. Planning for fractures in the sagittal plane
If the obliquity of the fracture is seen in the lateral view, follow the same principles as described for fractures seen in the AP view.
The approach will be determined by the exact fracture configuration.
Screws perpendicular to fracture plane
The lag screws must be inserted as perpendicularly to the fracture plane as possible.
6. Drilling
Drilling for lag screws
There are two options to prepare the gliding hole and the threaded hole:
1) Gliding hole first
Drill the gliding hole in the near cortex. Ensure perfect fracture reduction and then insert a drill guide. Drill the threaded hole in the far (trans) cortex through the drill guide.
This method ensures that the threaded hole is perfectly in line with the gliding hole.
This is the preferred method.
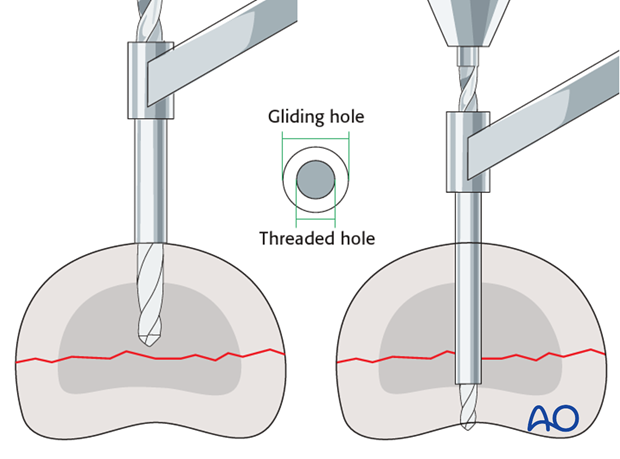
2) Threaded hole first
Drill a hole through both cortices, using the drill for the threaded hole. Then use the corresponding larger drill bit to overdrill the near cortex to create the gliding hole.
This technique is useful for small fragments. The disadvantage, however, is that the holes may not be centered in relation to each other.
Pearl
If the near cortex is tapped prior to overdrilling for the gliding hole, eccentric passage of the second drill is less likely. This can be achieved by inserting the chosen self-tapping screw through the near (cis) cortex and then removing it. The drill will now follow exactly the threaded axis.
No countersinking in the metaphysis
Do not countersink the screws in the metaphysis as its cortex is very thin.
If countersinking is attempted, all purchase and compression may be lost due to screw breakthrough.
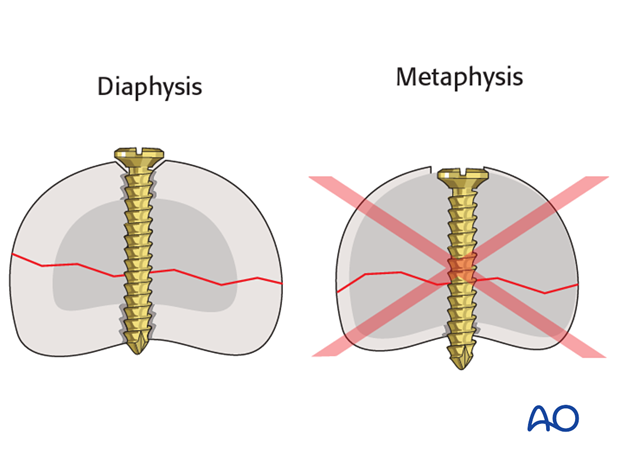
Countersinking in diaphyseal bone
There are two important reasons for countersinking:
- The risk of soft-tissue irritation is greatly reduced by ensuring that the the screw head protrudes only minimally from the bone surface.
- Countersinking ensures that the screw head has a maximal contact area with the bone, distributing the forces from the screw head more widely and more biodynamically than an unsunk head.
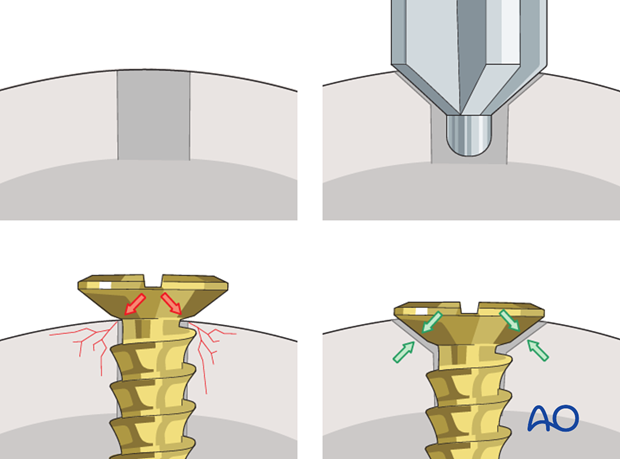
Pitfall: breaking the cortex in diaphyseal bone
Do not advance the countersink too deeply into the cortex: the cortical thickness will determine the depth of countersinking. Excess penetration risks break-through of the screw head when tightened and loss of fixation. Countersinking is, therefore, done by hand and not with a power tool.
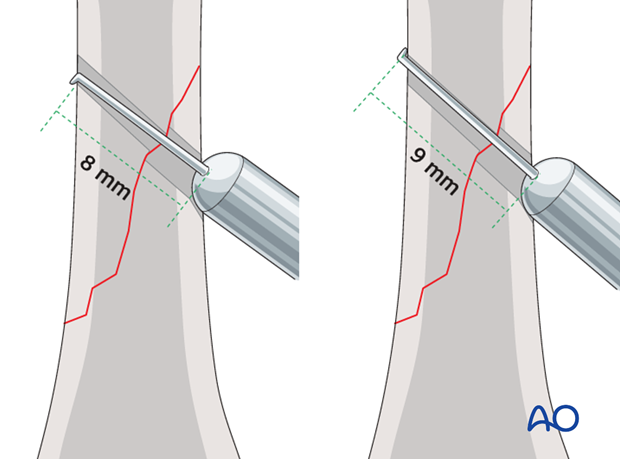
Pitfall: Oblique measurement
When measuring for screw length in oblique drill holes, the measurement to the acute angle is different from the measurement to the obtuse angle. This problem increases with the degree of obliquity.
Always measure both angles and use the longer measurement. However, keep in mind that too long a screw can protrude to the extent that it puts the soft tissues at risk.
Screw length pitfalls
Ensure that a screw of the correct length is used.
- Too short screws do not have enough threads to engage the cortex properly. This problem increases when self-tapping screws are used due to the geometry of their tip.
- Too long screws endanger the soft tissues, especially tendons and neurovascular structures. With self-tapping screws, the cutting flutes are especially dangerous, and great care has to be taken that the flutes do not protrude beyond the cortical surface.
7. Fixation
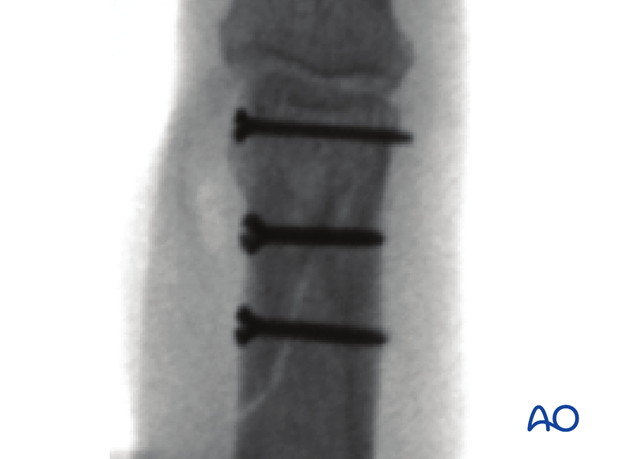
Insert first screw
As discussed in the preparation section, insert the first of the 3 lag screws through the center of the fracture surface and carefully tighten this screw.
The fracture is now compressed. The reduction forceps may be removed.
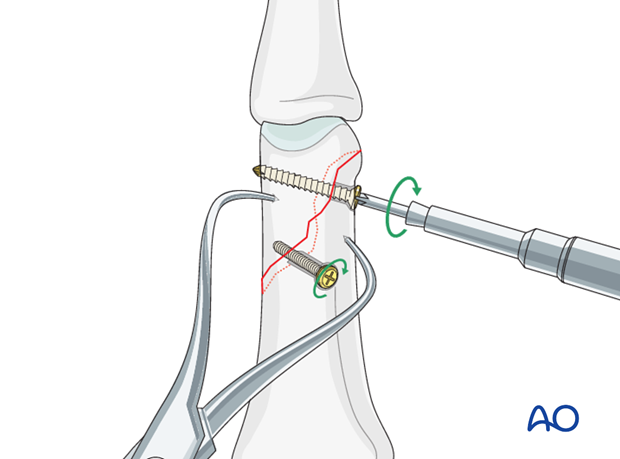
In short fragment
Insert both screws before fully tightening them.
It is important to tighten the two screws alternately in order not to displace the fragment.
Pearl: smaller peripheral screws
In cases where a peripheral screw has to be inserted close to the apex of a fragment, use a smaller diameter screw. Keep in mind that the minimal distance to the fracture line must be equal to the diameter of the screw head.
Insert remaining screws
Prepare for the remaining screws in a similar fashion to the first.
Insert the screws and carefully tighten them alternately.
Confirm fixation using image intensification.
8. Aftertreatment
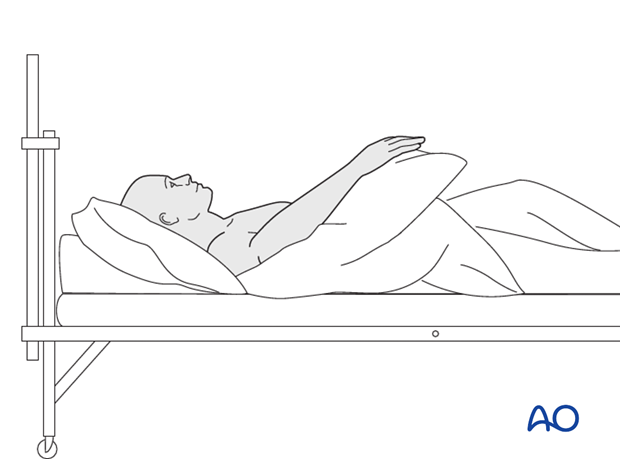
Postoperatively
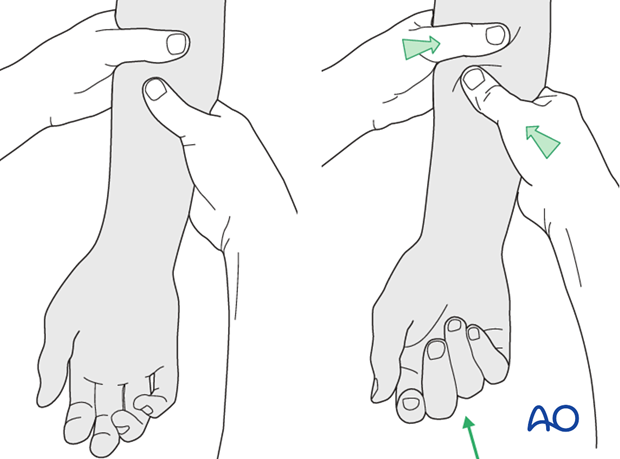
Protect the digit with buddy strapping to the adjacent finger, to neutralize lateral forces on the finger.
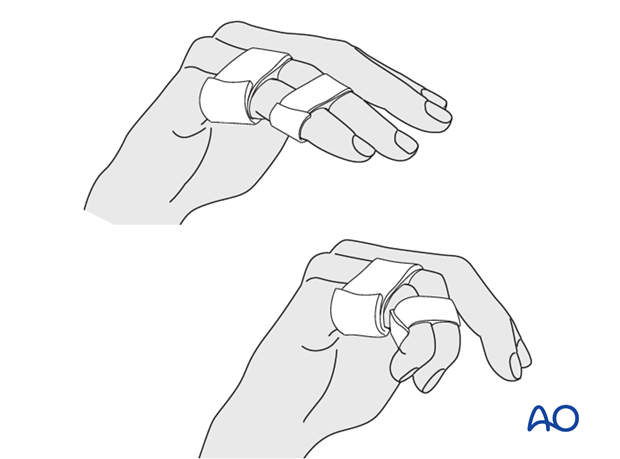
Functional exercises
The patient can begin active motion (flexion and extension) immediately after surgery.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Follow-up
See the patient 5 days and 10 days after surgery.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.













