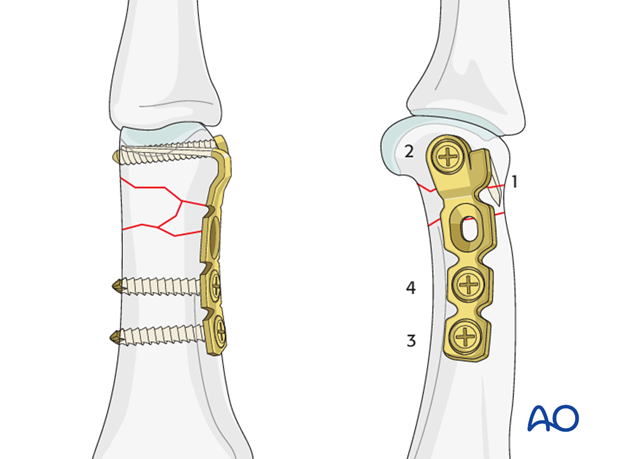
Minicondylar bridge plate fixation
1. Indications
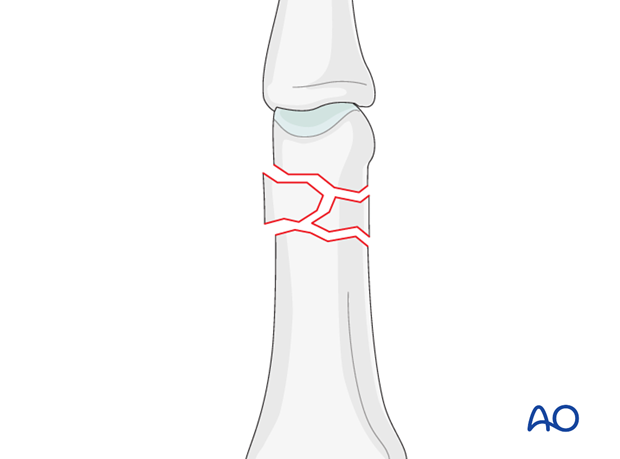
Fractures of the distal metaphysis can be transverse, oblique, or comminuted.
Always confirm the fracture configuration with views in both planes.
Irreducible and unstable fractures require ORIF.
Other indications for ORIF are open fractures, or soft-tissue lacerations.
2. Approach
For this procedure a midaxial approach to the proximal phalanx is normally used.

3. Reduction
Reduction principles
Indirect reduction is achieved by traction and manipulation.
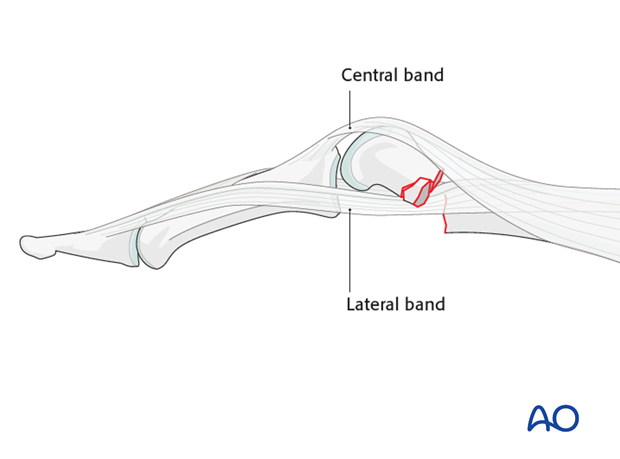
Sometimes indirect reduction may be prevented by interposition of the lateral band.
If the fracture is irreducible, ORIF is indicated.
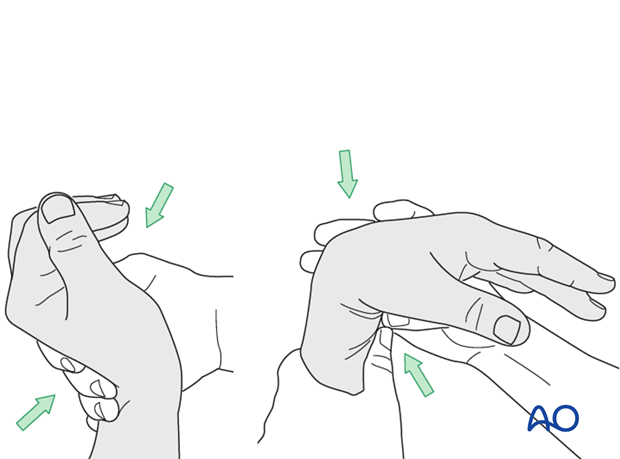
Indirect reduction by traction
Reduction can be achieved by traction and flexion exerted by the surgeon,...
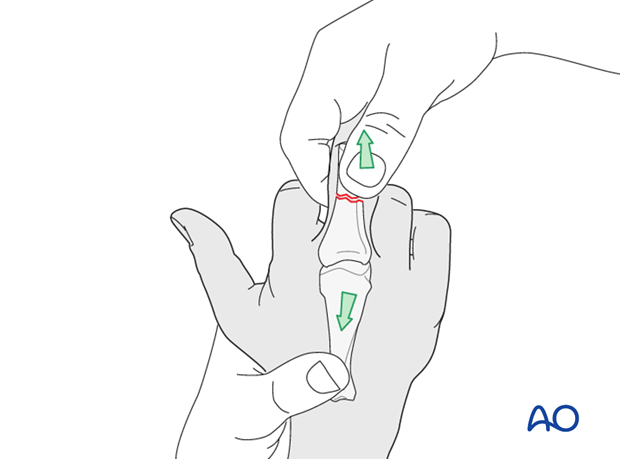
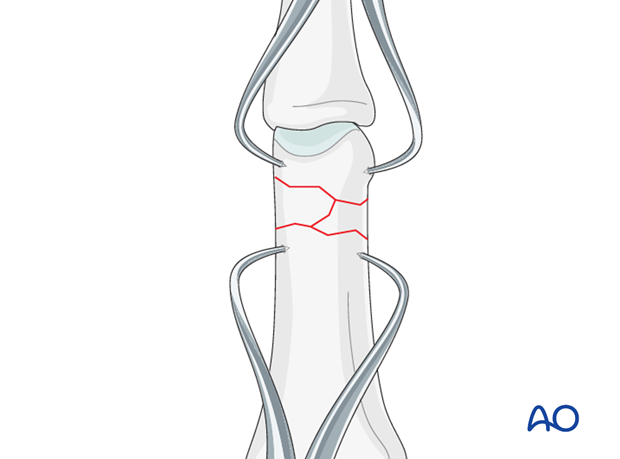
... or by two forceps. Confirm reduction using image intensification. Rarely are these fractures stable after reduction, but in those cases, nonoperative treatment can be used.
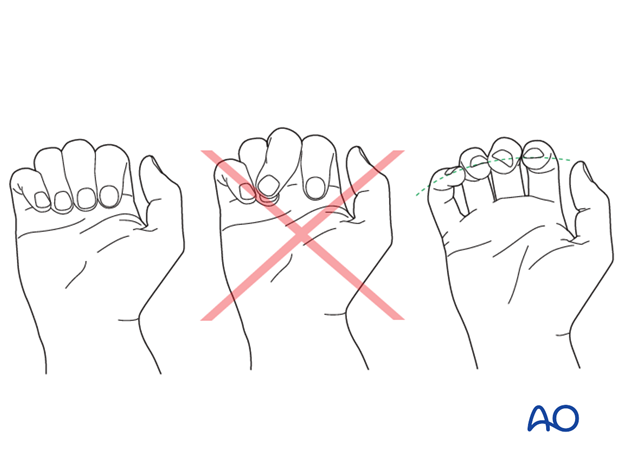
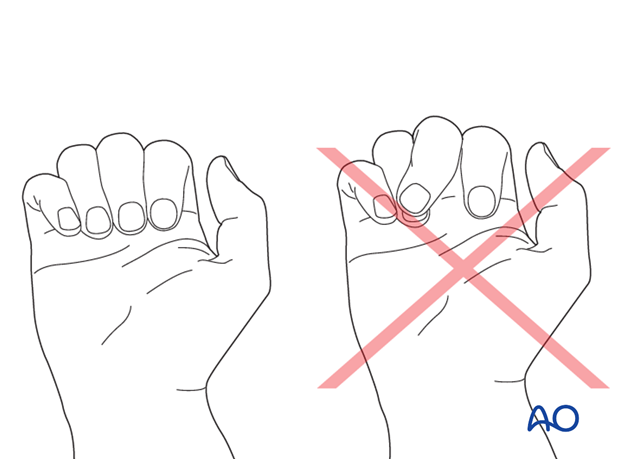
Identifying malrotation
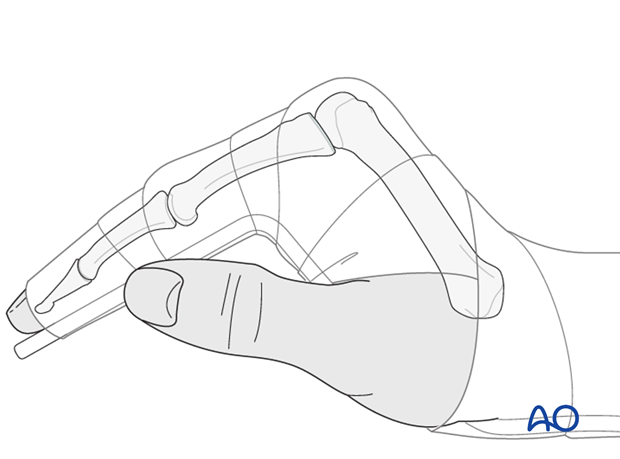
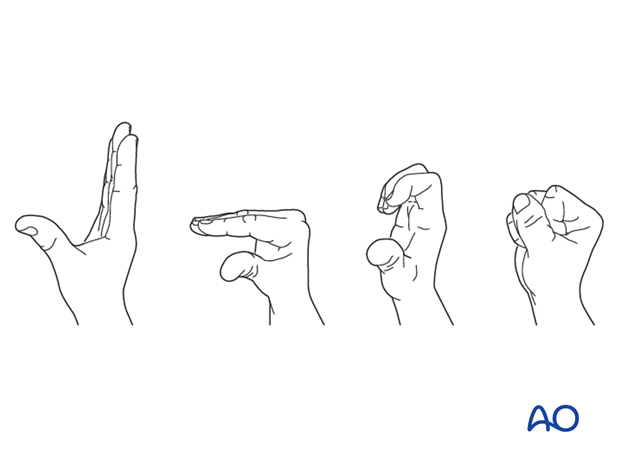
At this stage, after provisional fixation, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with the fingers in a degree of flexion, and never in full extension. Malrotation may manifest itself by overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by tilting of the leading edge of the fingernail, when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
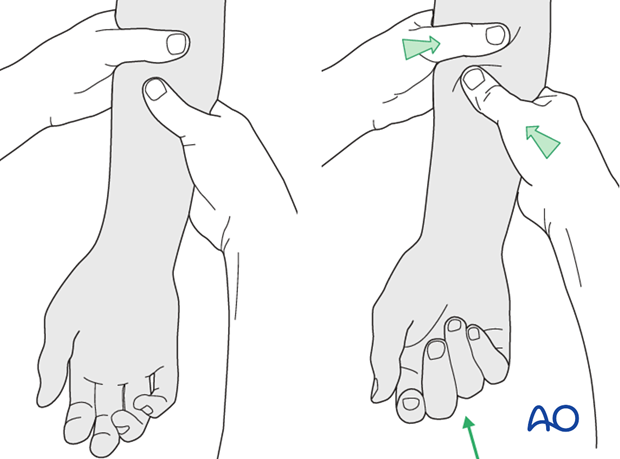
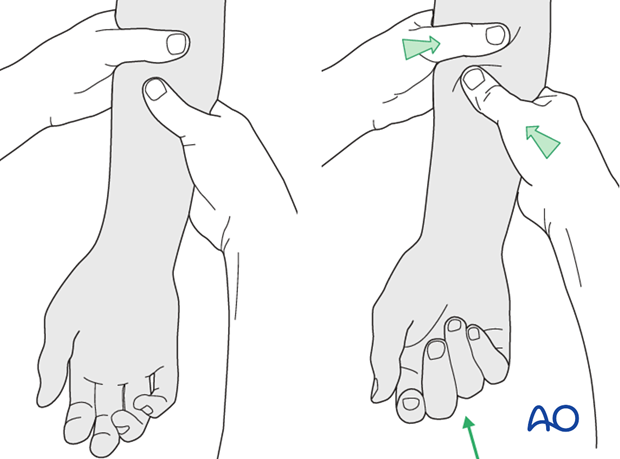
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, the surgeon fully flexing the wrist to produce extension of the fingers, and fully extending the wrist to cause flexion of the fingers.
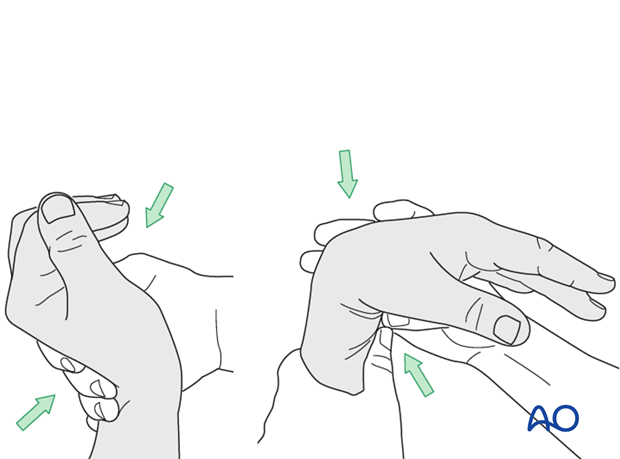
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
4. Plate preparation
Planning plate position
It is wise to use magnifying loupes for this step.
Plan the blade position as dorsal as possible, in order not to injure the collateral ligament.
Make sure that the plate will be perfectly aligned with the long axis of the proximal phalanx in the lateral view.
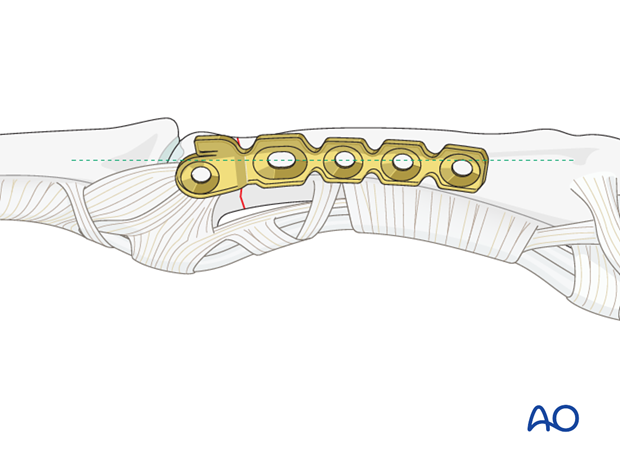
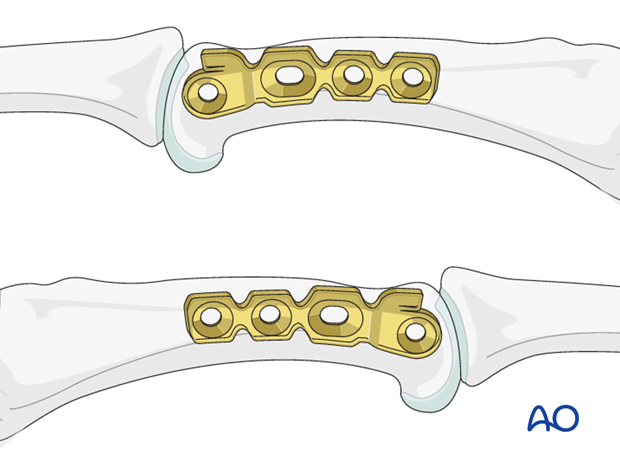
Corresponding flare
The position of the plate should be distal enough to ensure that the metaphyseal flare fits to the shape of the shoulder of the plate.
The minicondylar blade plates are available in two forms. One fits on the ulnar aspect of the bone, and the other on the radial aspect. It is a common mistake to choose the wrong one. The correct implant will have the blade dorsal and the distal screw hole palmar.
Trim the plate
Adapt the plate length to fit the length of the proximal phalanx. Avoid sharp edges which may be injurious to the tendons. There should be at least 3 plate holes proximal of the fracture available for fixation in the diaphysis. At least two screws need to be inserted into the diaphysis.
Prepare the blade
Measure the length of the drill hole.
Cut the blade to the determined length, so that it just fills the drill hole.
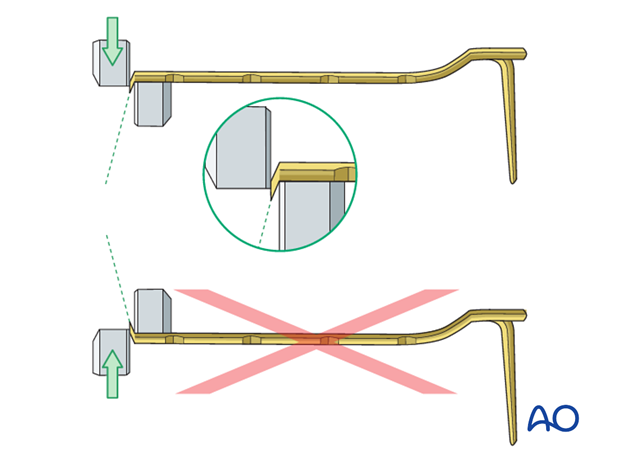
Pearl: Cut the blade transversely
If you cut the blade on the flat, it will compress and widen very slightly as it is cut. This makes its maximal width very slightly larger than 1.5 mm. It may not fit in the 1.5 mm hole that you have drilled.
Therefore, cut the blade on edge (to deform it through its narrower dimension) to the correct length. The resultant tip is somewhat arrow-shaped.
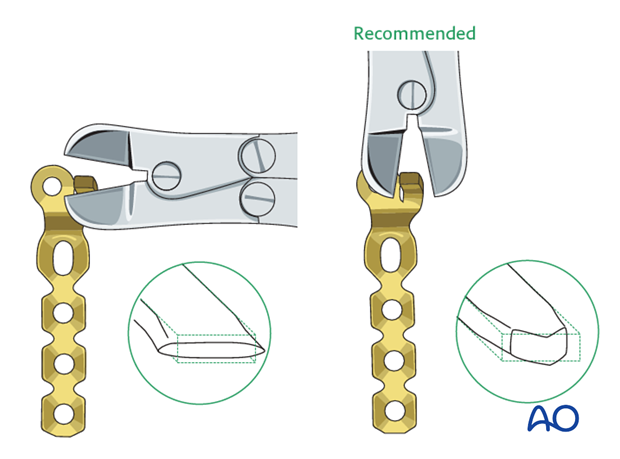
Pitfall: avoid dangerous edge
If you are using a dedicated minicondylar plate cutter which trims the plate by a shearing action, be very careful not to create a sharp dorsal edge that will endanger the extensor apparatus. Correct cutting will produce the sharp edge on the bone side of the plate.
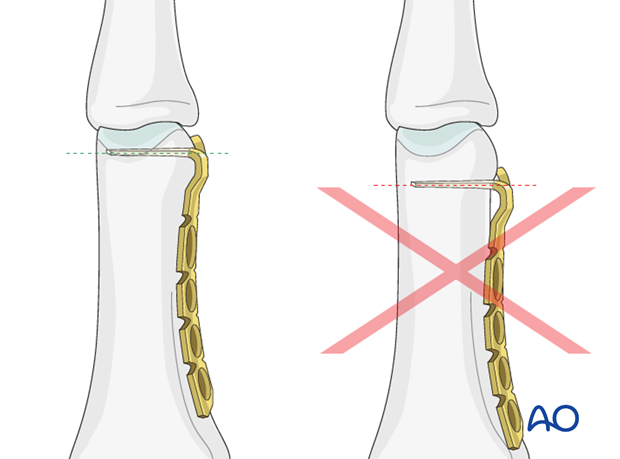
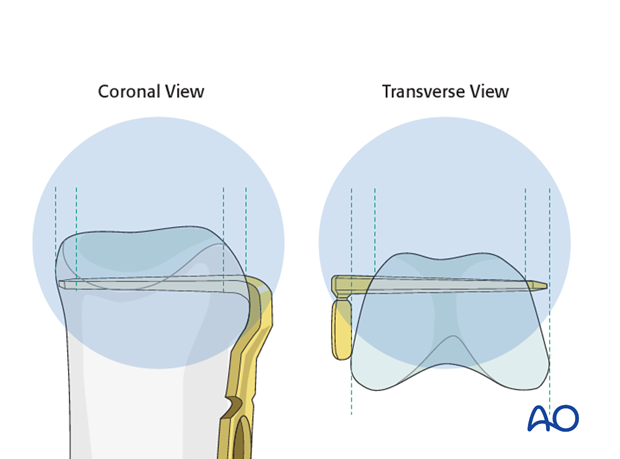
Pitfall: Protrusion of the blade
Avoid protrusion of the blade through the opposite cortex, as friction during movement and eventual ligament injury may result.
Due to the fact that the phalanx is wider on the palmar side that on the dorsal side, an AP or PA x-ray view may suggest that the blade is fully contained within the bone, whereas in transverse section, it actually protrudes.
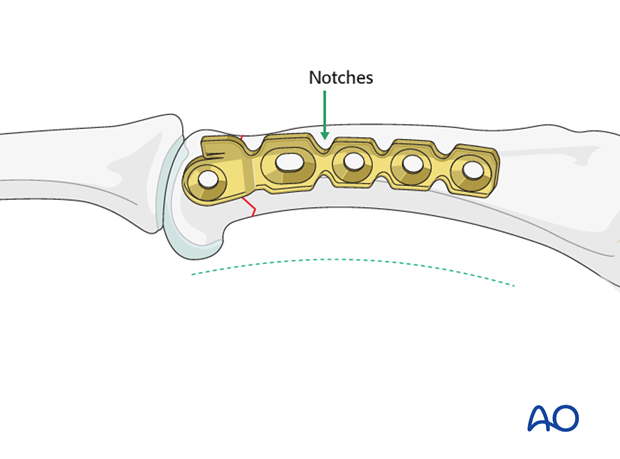
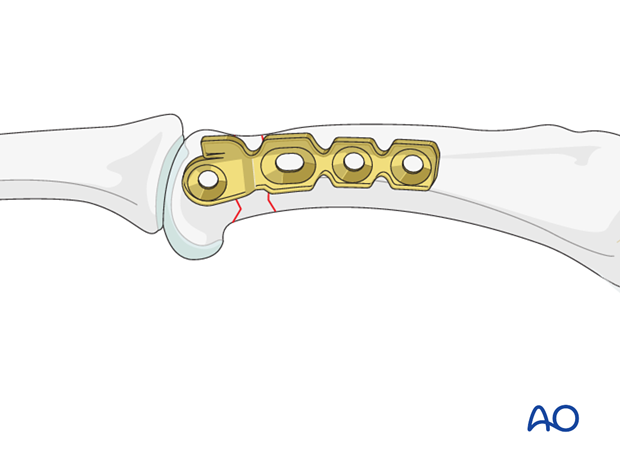
Contouring of the plate
Twist and bend the plate to follow exactly the shape of the phalangeal diaphysis.
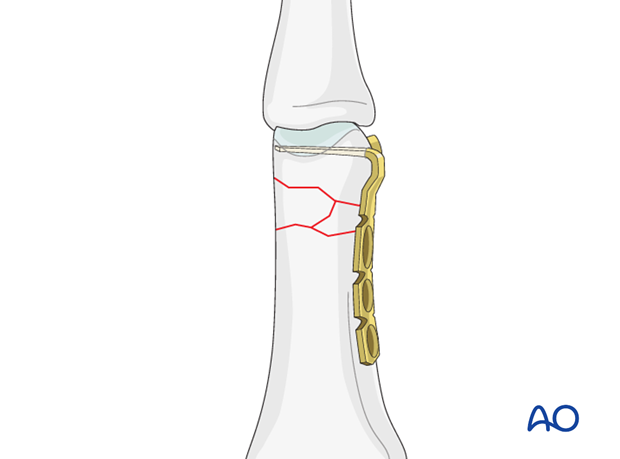
As the minicondylar plate has notches (like a reconstruction plate), it can also be curved on the flat to fit the curve of the phalanx.
Note
It is worth investing time in the precise contouring of the plate to the phalanx. Any imperfection in contouring will result in fracture displacement when the diaphyseal screws are tightened.
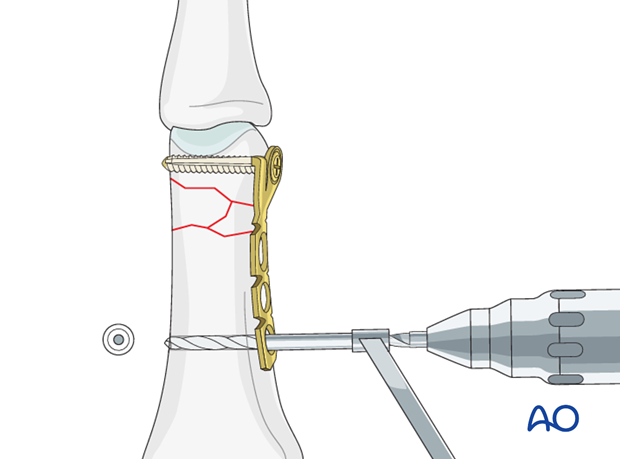
5. Drilling
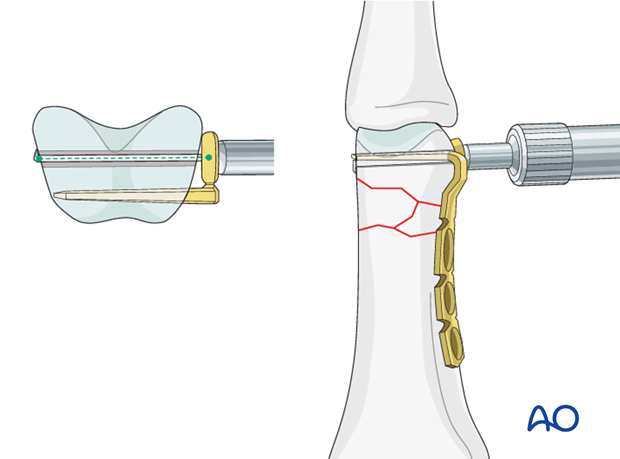
Determine location of drill hole
In order to determine the position of the first drill hole (for the blade), it is helpful to turn the plate over and use it as a template.
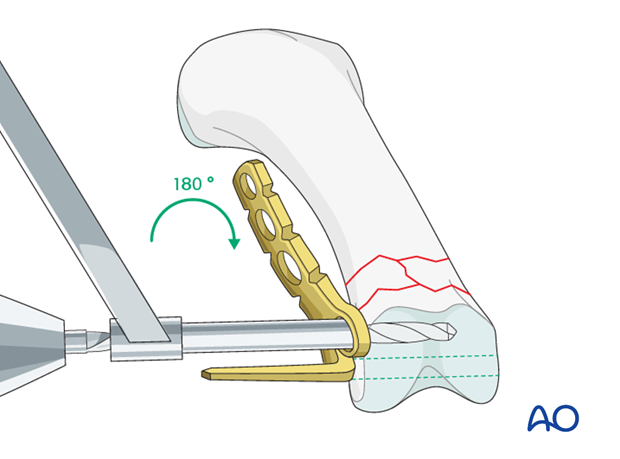
Drill a 1.5 mm transverse hole through the condylar metaphysis of the proximal phalanx adjacent to the subchondral bone, to create a track for the blade.
This drill hole needs to be sufficiently dorsal to leave enough space for the plate’s most distal hole, adjacent to the blade.
6. Plate application
Blade introduction
Introduce the blade into the drill hole. Gently push with the thumb until the blade is fully seated.
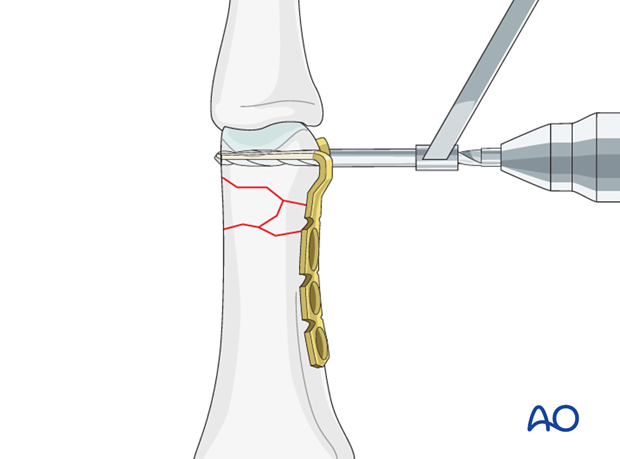
Align the plate with the diaphysis
Before inserting distal screw adjacent to the blade, ensure that the plate is in line with the phalangeal diaphysis in the lateral view by rotating it around the long axis of the blade.
Insert distal screw
The distal screw is then inserted in a neutral position.
The screw should just engage the far cortex.
Note
Be careful to avoid screw protrusion, as ligament injury may result from friction during movement.

Drill neutral proximal hole
Use a 1.1 mm drill bit to prepare the first neutral thread hole for the screw at the proximal end of the plate.
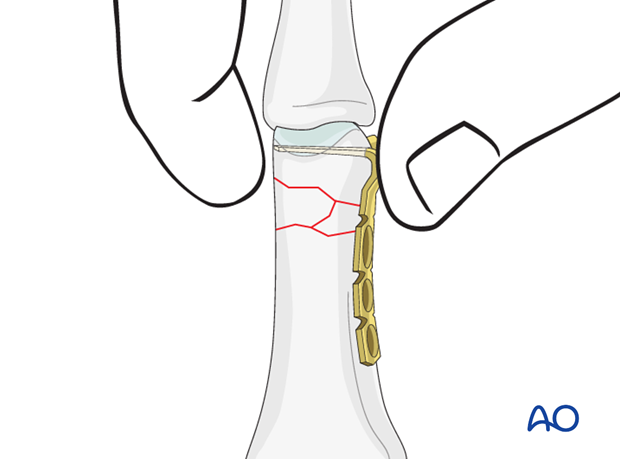
Rotation check
At this stage, after provisional fixation, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the fingers.
Under general anesthesia, the tenodesis effect is used, the surgeon fully flexing the wrist to produce extension of the fingers, and the full extension of the wrist to cause flexion of the fingers.
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
Insert remaining screws
Insert the remaining diaphyseal screws in neutral positions.
7. Aftertreatment
Postoperatively
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
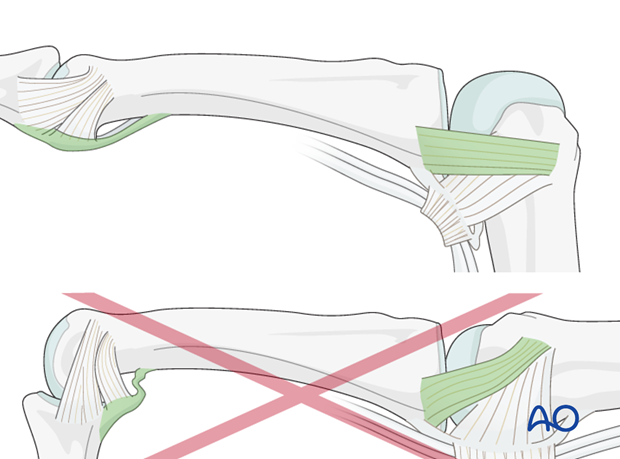
Postoperative splint
A removable splint should be applied at the end of the operation, with the hand in an intrinsic plus position (“safe” or “Edinburgh” position).
Immobilize the hand in a safe position for 2-3 weeks.
Keep ligament extended
The reason of immobilization of the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains length of the volar plate.
Pitfall: scarring
If the collateral ligament develops scarring when not out to length, full extension will become impossible.
Similarly, immobilizing the PIP joint in flexion, can result in scar contraction of the volar plate, also limiting joint extension.
Follow-up
See patient 5 days after surgery to check the wound, clean and change the dressing. After 10 days, remove the sutures. Check x-rays.
Functional exercises
The fixation will be vulnerable for the first 2-3 weeks.
At this stage, remove the splint, and apply buddy strapping.
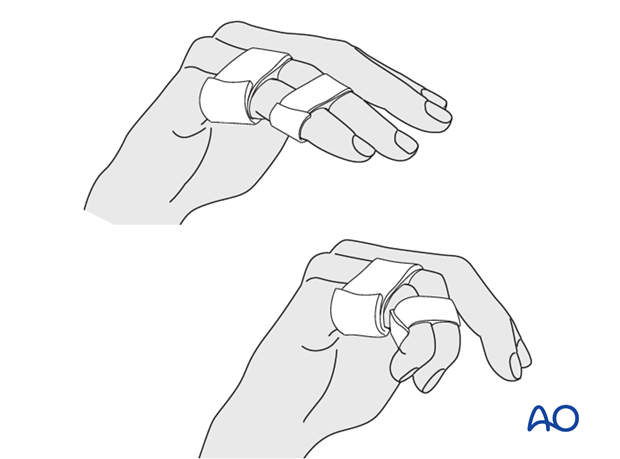
Then begin with active motion exercises.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.













