Ligament reattachment with suture anchors
1. Principles
Introduction: Avulsion / ligamentous rupture
Ulnar collateral ligament injuries are also named skier’s, or gamekeeper’s, thumb. If undiagnosed it leads to chronic instability and weakness of pinch.
Ulnar collateral ligament tears are the result of abduction forces acting on the thumb, putting the ligament under sudden excessive tension.
Avulsion fractures of the thumb are treated in a fashion similar to the other proximal phalanges. Options for treatment are lag screw fixation, cerclage compression wiring, or anchor suture for comminuted fractures where the fragments will be excised.
Note: We now prefer the term “Cerclage compression wiring” to “Tension band wiring” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
Diagnosis
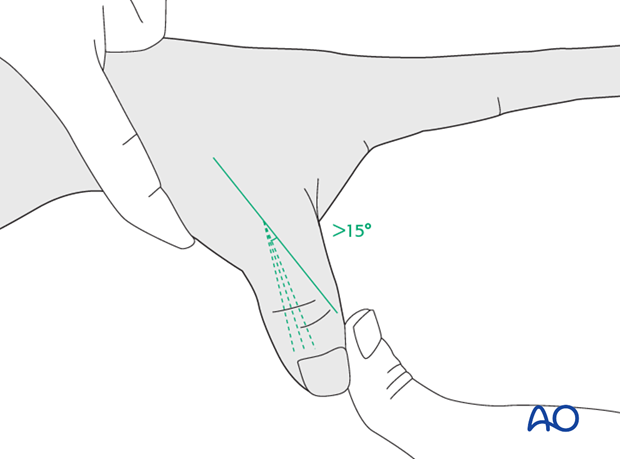
After injection of a local anesthetic into the metacarpo-phalangeal (MP) joint, stress testing is performed in 30 degrees of flexion. This is necessary in order to exclude any influence of the intact volar plate on stability when tested in full extension.
Compare the test with the uninjured side. More than 15 degrees difference and a soft end point indicate a complete rupture of the ligament.
Choice of treatment
Nonoperative treatment
If the stress test under local anesthesia shows less than 15 degrees difference compared with the opposite side, and a firm end point, the injury can be treated nonoperatively with a period in a protective cast for about 4-6 weeks.
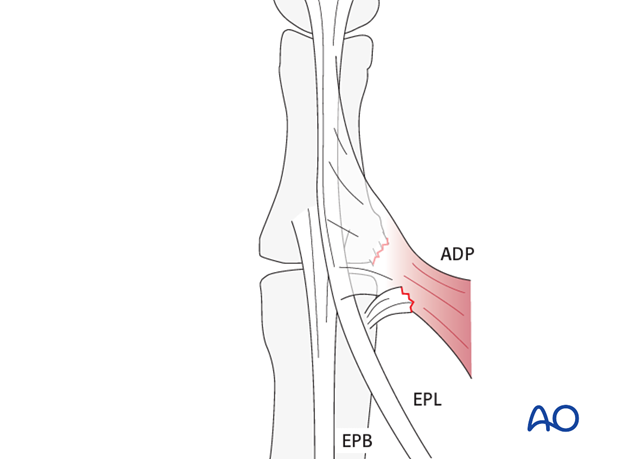
Anatomy: Stener’s lesion
The proximal edge of the adductor aponeurosis is responsible for Stener’s lesion. The ulnar collateral ligament stump is displaced dorsally to the aponeurosis, which prevents ligament healing.

Suture anchors or tunneling
Two alternative techniques are available for collateral ligament reattachment: suture anchors, or tunneling.
The advantage of suture anchors is the relative ease of the procedure.
Tunneling is the more demanding procedure, but it is significantly less expensive.
2. Approaches
For this procedure the following approaches may be used:
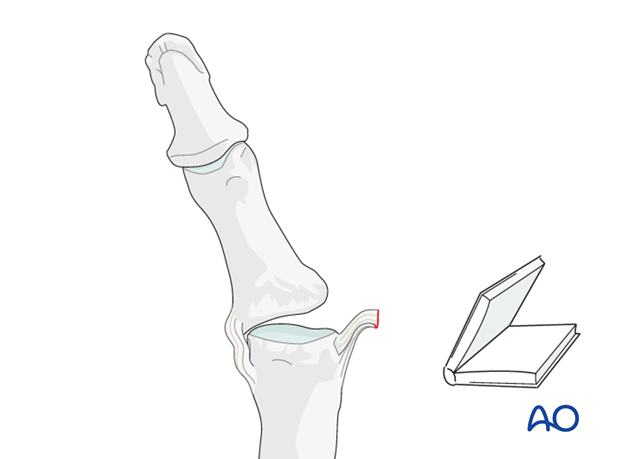
3. Visualize the joint
Abduct the phalanx to gain maximal visualization of the joint (open book).
Irrigate the joint. Check for additional lesions (e.g. volar plate injury).
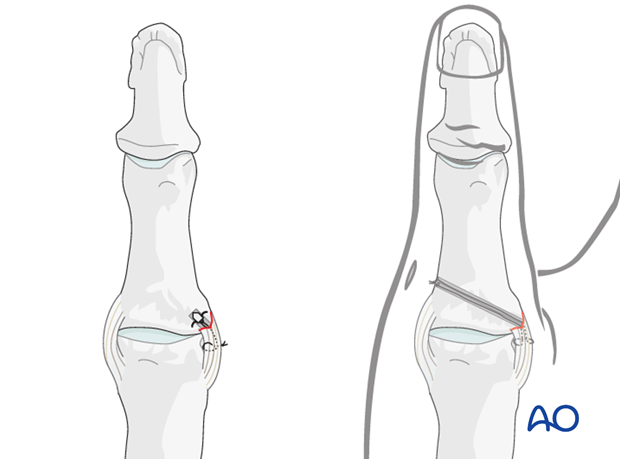
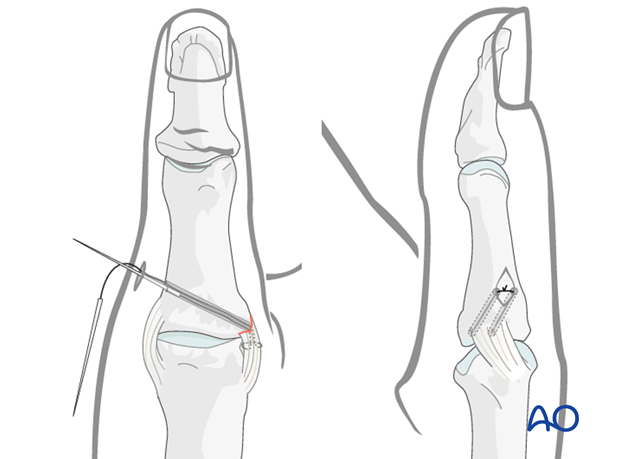
4. Option 1: suture anchor fixation
Drill anchor hole
Keep the phalanx abducted to expose maximally the area of the avulsion from the base of the phalanx.
Make a perforation of the same diameter as the anchor to be used, at the site of ligament insertion. The anchor should be placed sufficiently palmarly to prevent rotatory subluxation of the joint.
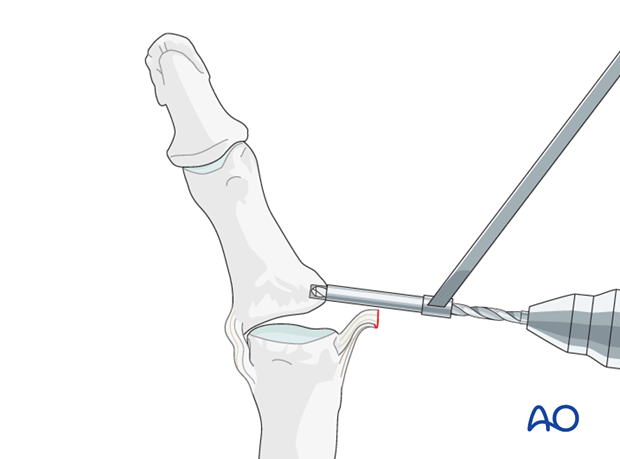
Insert anchor
Insert the anchor according to the manufacturer’s instructions. Ensure that the whole anchor is completely buried in the bone.
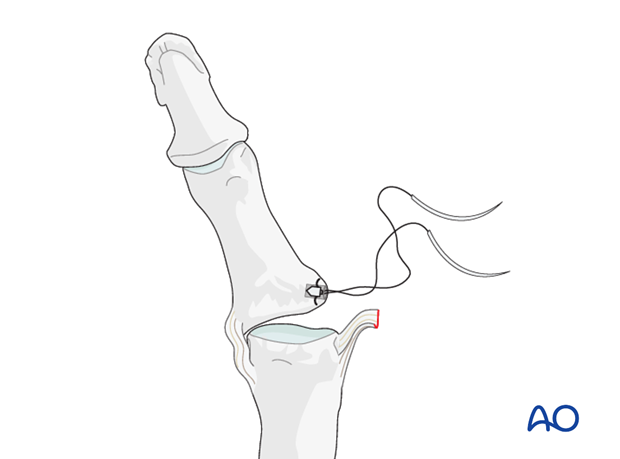
Insert the sutures
Insert the sutures into the free end of the ligament.
Reapproximate the ligament to the phalanx and make a loop in each end of the thread as an anchoring pass. Tie the suture to secure the ligament to the phalanx.
5. Option 2: tunneling
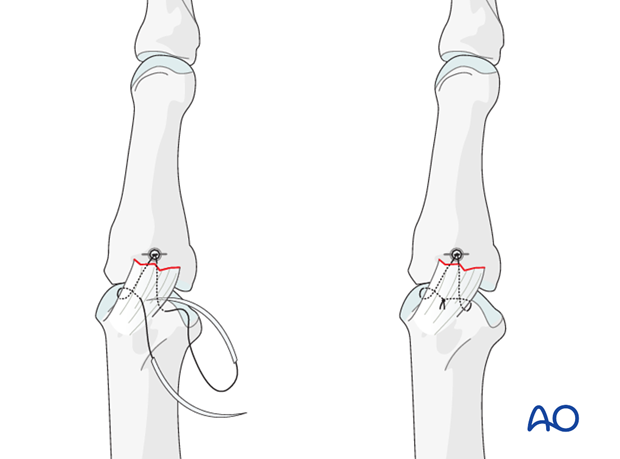
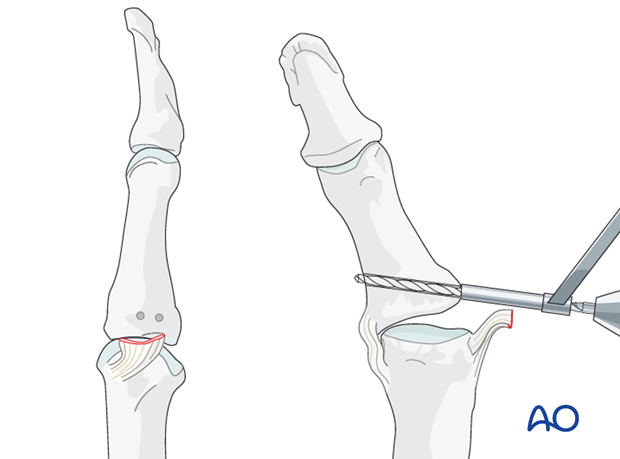
Drill holes
A pair of parallel perforations can be made at the site of ligament insertion, using a 1.0 mm drill or a K-wire, angled from proximal to distal, and from palmar to dorsal, penetrating the opposite cortex.
Always use a drill sleeve for soft-tissue protection.
Insert sutures
Nonresorbable 4.0 thread sutures, with straight needles, are used.
Insert the sutures as illustrated, through the end of the ligament. Thread each needle through a drill hole.
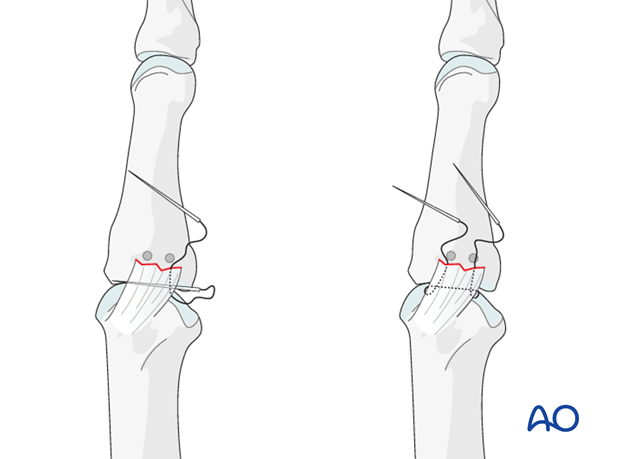
Reapproximate the ligament
Make a small incision on the opposite side of the thumb to retrieve the sutures. Cut off the needles, pull the sutures to approximate the ligament, and tie a knot over the cortical bone.
6. Aftertreatment
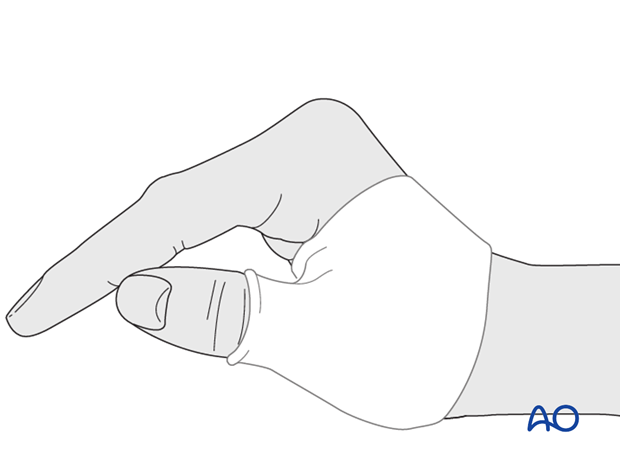
Orthoplast splint
In compliant patients, a well-padded orthoplast splint is sufficient for immobilization. This has the advantage of leaving the wrist free.
Thumb spica
In noncompliant patients, a more restrictive well-padded thumb spica may be a wiser choice.
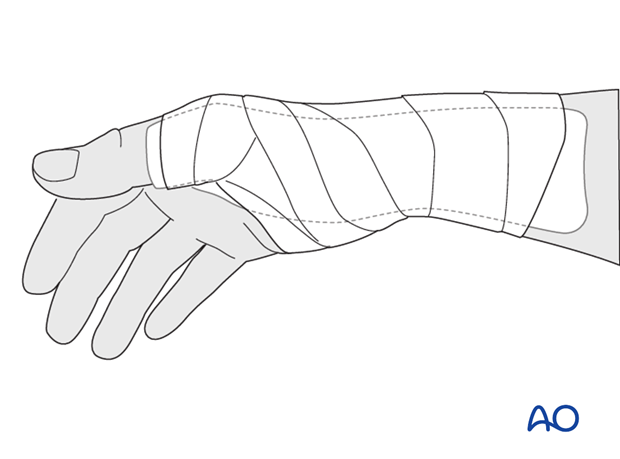
Immobilization and functional exercises
4-6 weeks of immobilization are necessary.
After that time, motion of the MP joint of the thumb starts without protection.
Heavy manual demand and all activities involving a strong pinch grip are not permitted until complete ligament healing (usually after 3 months).
Teaching video
AO teaching video: Application of the thumb spica













