Open reduction, internal fixation (ORIF)
1. Principles
Introduction
Intraarticular fractures of the proximal phalanx of the thumb must be treated radically to avoid
- loss of motion
- post-traumatic arthrosis.
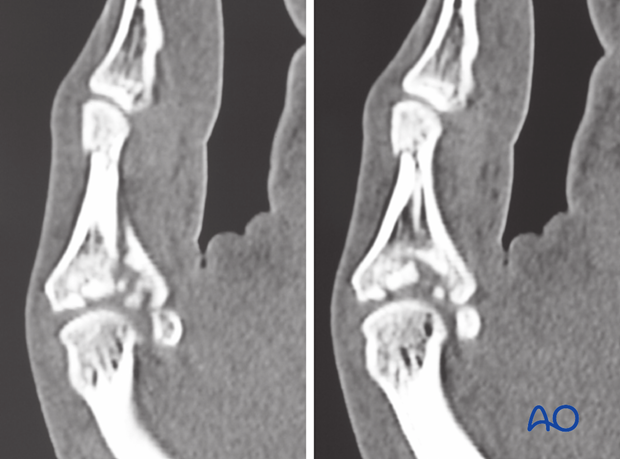
Articular congruity should be restored anatomically. In cases of comminuted impacted fractures (“pilon”), bone graft from the distal radius is needed to fill the metaphyseal defect.
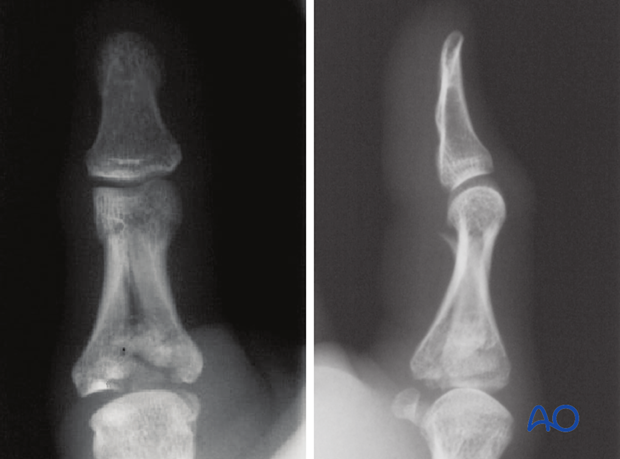
It is difficult to assess the extent of articular comminution from plain radiographs. A CT scan is advisable.
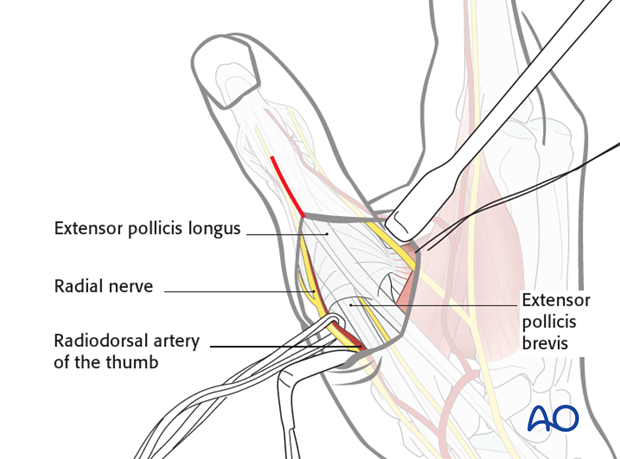
Choice of approach
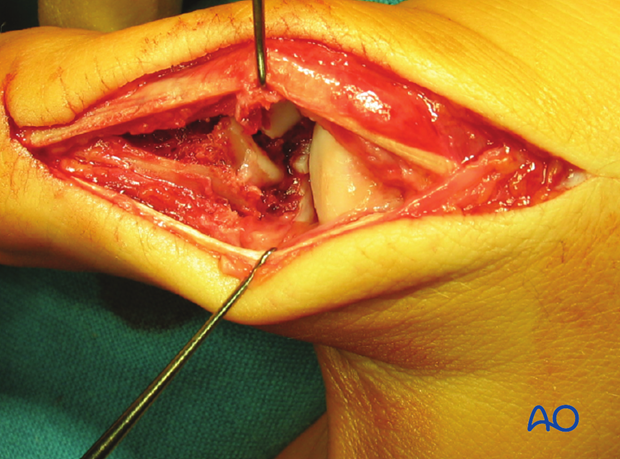
In the case of extension of the fracture into the diaphysis, the dorsal approach to the MCP joint is modified so that the distal incision extends as far as the interphalangeal (IP) joint. The IP joint itself will not be opened.
Be careful not to detach the insertion of the extensor pollicis brevis (EPB) into one of the basal fragments.
2. Reduction
Restoration of the articular surface
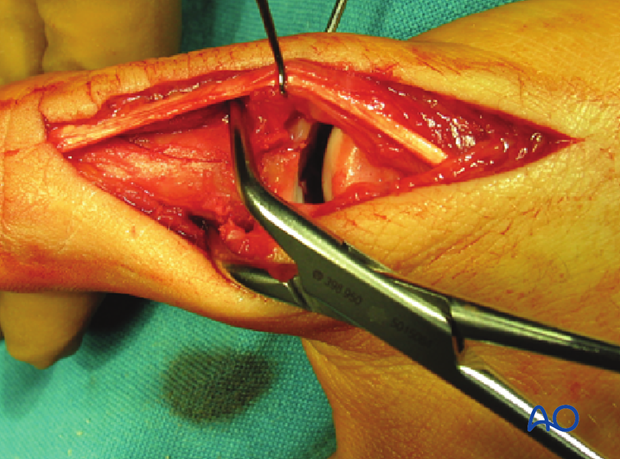
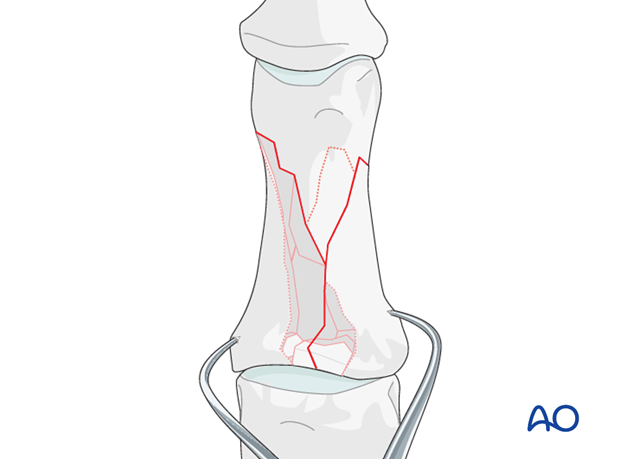
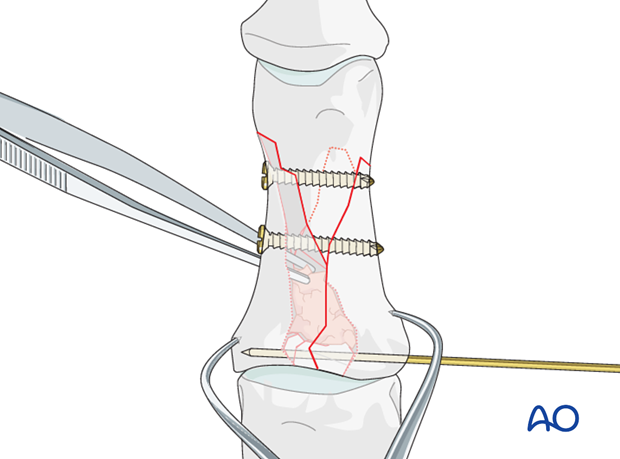
With a periosteal elevator, reduce the articular fragments, ...

... using the head of the first metacarpal as a template.
Reduction of diaphyseal fragments
Use a pointed reduction forceps to reduce and hold the diaphyseal fragments.
During the diaphyseal reduction, check under direct vision that no displacement of articular fragments occurs.
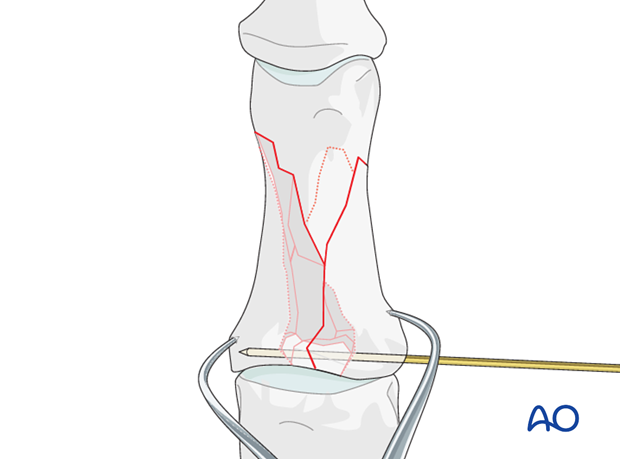
Fixation of articular fragments
In case the fragments are too small for screw fixation, carefully insert a K-wire to fix the articular fragments.
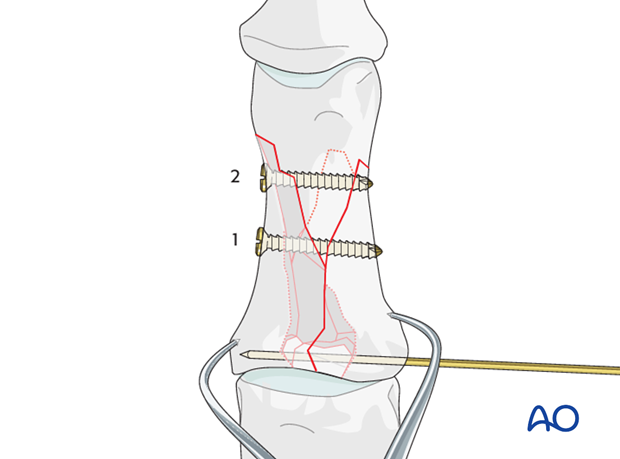
3. Lag screw fixation
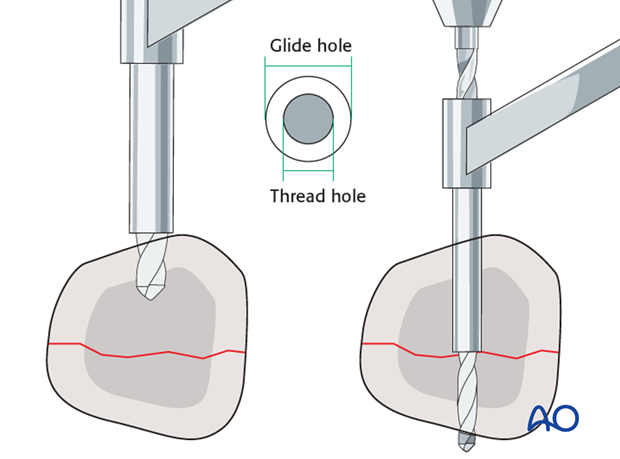
First lag screw in the middle of the shaft
A first lag screw will be inserted into the middle of the shaft.
Drill the gliding hole in the near cortex. Ensure and hold a perfect fracture reduction and then insert a drill guide. Drill the thread hole in the far (trans) cortex through the drill guide.
This method ensures that the threaded hole is perfectly in line with the gliding hole.
Countersink the near cortex as necessary.
Measure for correct screw length.
Insert the lag screw and tighten it.
Second lag screw
Repeat the above procedure for a second lag screw to be inserted into the distal part of the diaphysis.
4. Bone graft
After diaphyseal fixation, the metaphyseal void must be filled with bone graft to support the reduced articular fragments, and to prevent secondary displacement.
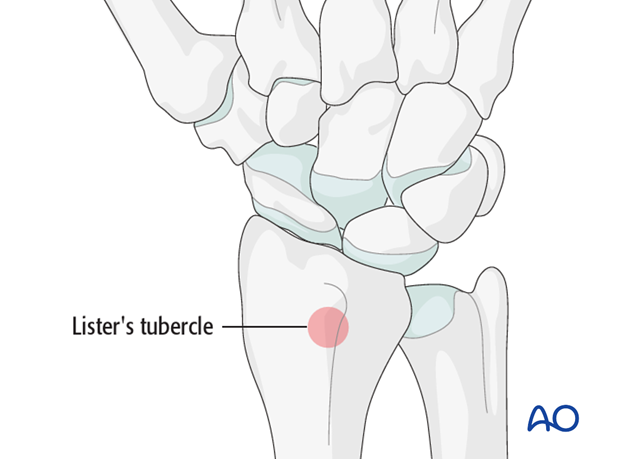
Harvest site
Harvest the graft material from the distal radius. A good and safe place for this is just proximal to Lister’s tubercle.
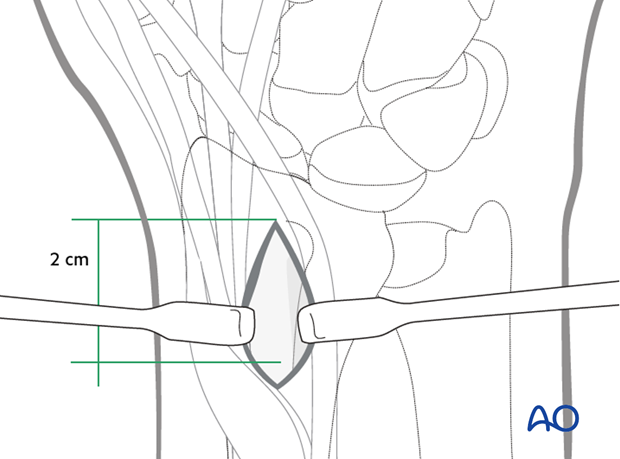
Harvesting
Make a 2 cm long incision proximal to Lister’s tubercle. Retract the tendons of the second compartment radially, and the EPL in an ulnar direction.
Use a chisel to cut three sides of a square. Hinge up the dorsal cortical flap. After harvesting cancellous bone, replace the “lid” and suture the periosteum and the skin incision.
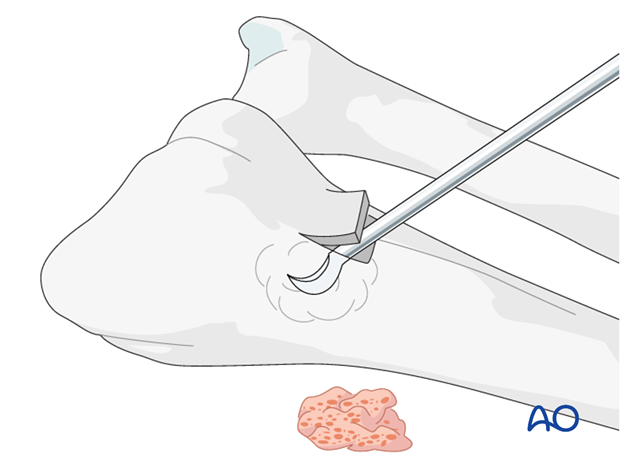
The bone graft is now inserted through a window of the metaphyseal cortex above the articular surface.
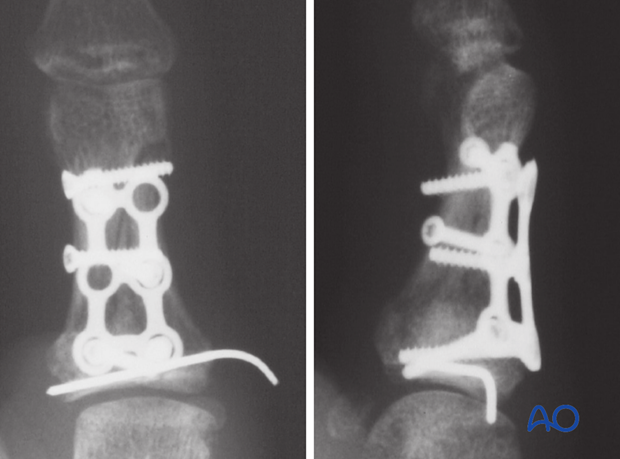
5. Plate fixation
Angularly stable plates are the preferred implants to use for protection. This kind of plate protects the reduced articular fragments and improves the stability of the fixation. Thereby they enable immediate postoperative mobilization.
Apply the plate to the bone and insert the screws according to the fracture pattern.
Test the stability of the fixation intraoperatively.
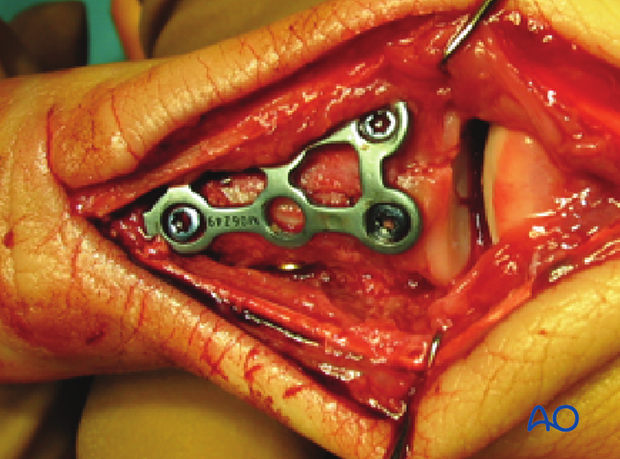
Completed ostesynthesis
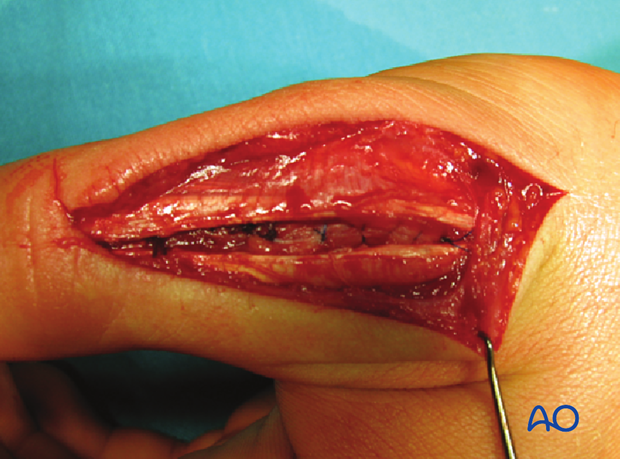
6. Closure
Suture the articular capsule proximally with nonabsorbable sutures. Distally cover the plate with periosteum, also with nonabsorbable sutures. This will protect the tendons from irritation as they glide over the plate.
7. Aftertreatment
Follow up
See the patient after 2 days for a change of dressing. After 10-12 days remove the sutures and confirm with x-rays that no secondary displacement has occurred.
Additional x-rays are taken 4 weeks after internal fixation to evaluate healing progress. Usually, the fracture line will still be visible.
X-rays are repeated after 8 weeks.
Strengthening exercises progressing to manual work are allowed according to the progress of bone healing.
If a K-wire was left protruding through the skin, the patient has to be instructed in cleaning the site every second day.
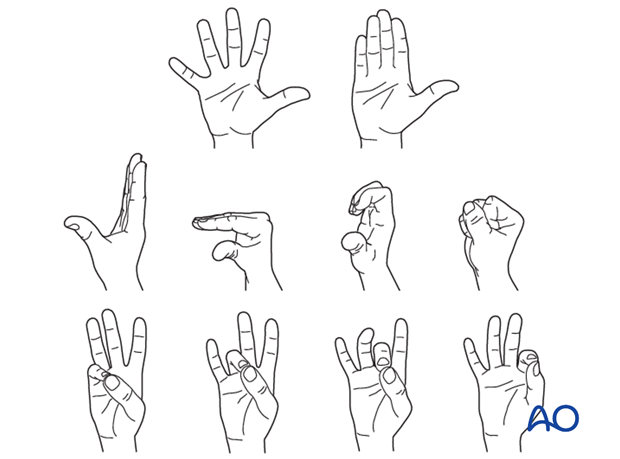
Functional exercises
As pain and swelling recede, early, active, controlled digital range of motion exercises, as illustrated, gently progress.
The importance of mobilization must be emphasized to the patient and rehabilitation should be supervised by a physical therapist.
Implant removal
Remove the K-wire after 4 weeks.
The other implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.













