Nonoperative treatment
1. Principles
Undisplaced, or minimally displaced, fractures of the diaphysis of the proximal phalanx can be treated nonoperatively.
Most of these fractures produce an extension deformity and minimal shortening. If the extension deformity exceeds 15-20 degrees, operative treatment is recommended. More than 2 mm shortening can not be accepted.
Undisplaced metaphyseal and articular fractures may also be treated nonoperatively.

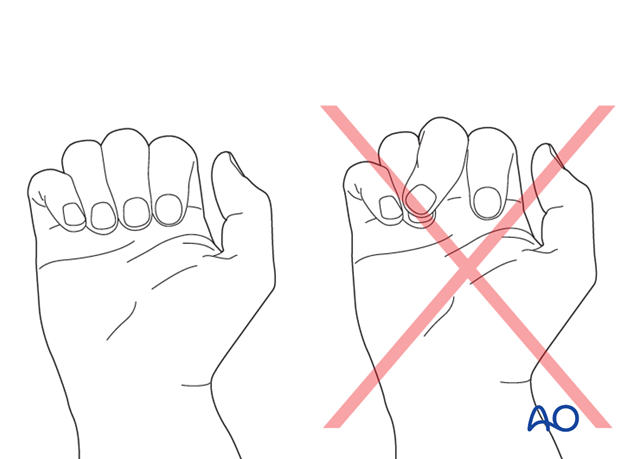
Irreducible rotational malalignment is an indication for operative treatment.
Teaching video
AO teaching video: Extension block splint (Burke Halter)
2. Reduction
Displacement usually occurs as an extension deformity.

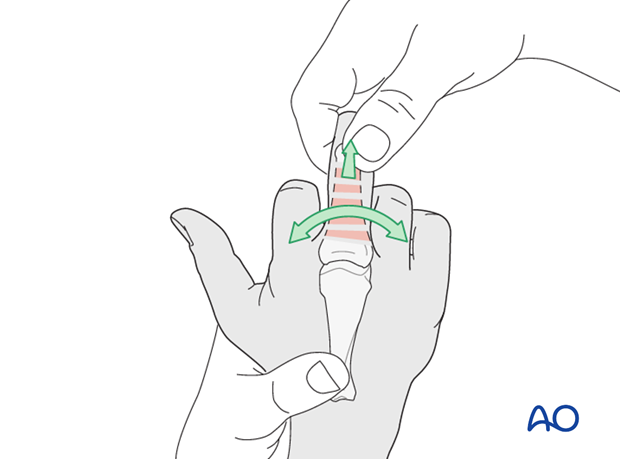
Reduction is achieved by applying longitudinal traction to the finger and flexing the MCP joint.
Rotational malalignment is also corrected.
Any lateral angulation can be checked by comparison with the adjacent fingers, and must be reduced.
Check angular reduction using image intensification.
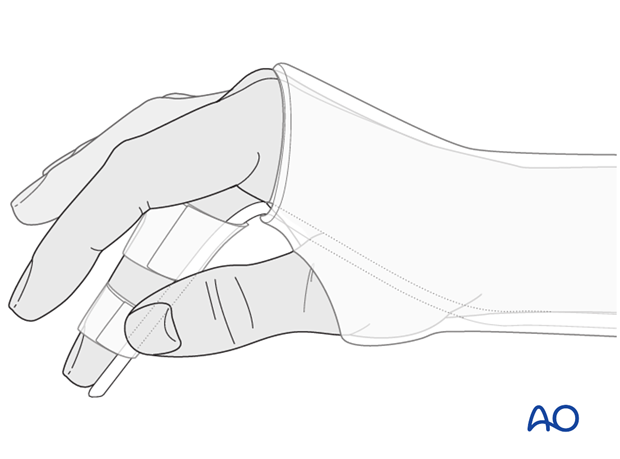
3. Option 1: Immobilization with palmar splint
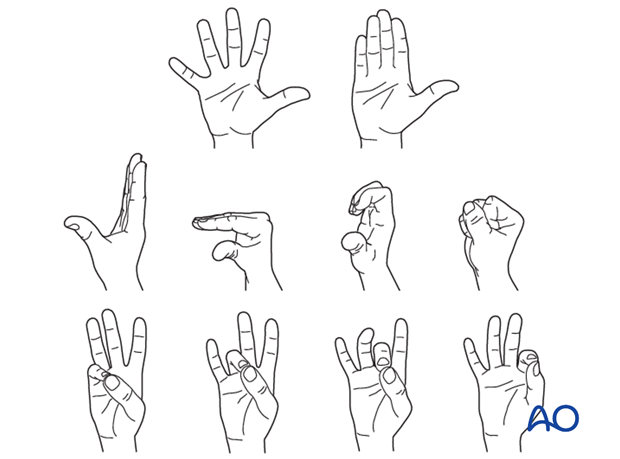
In undisplaced fractures, a splint may be applied with the hand in an intrinsic plus (Edinburgh) position and the wrist in slight extension of 20-30 degrees.
In compliant patients, only the fractured finger ray and the two adjacent rays are included in the splint.
The splint is held in place with an elastic bandage. The bandage should not be overtightened at the level of the wrist joint, in order to avoid excessive swelling of the hand.
Direct skin contact of adjacent fingers should be prevented by placing gauze pads between them.
This splint is easy to apply and needs no hand therapy during the period of immobilization. A potential disadvantage of this technique is the complete immobilization of uninjured fingers and joints.
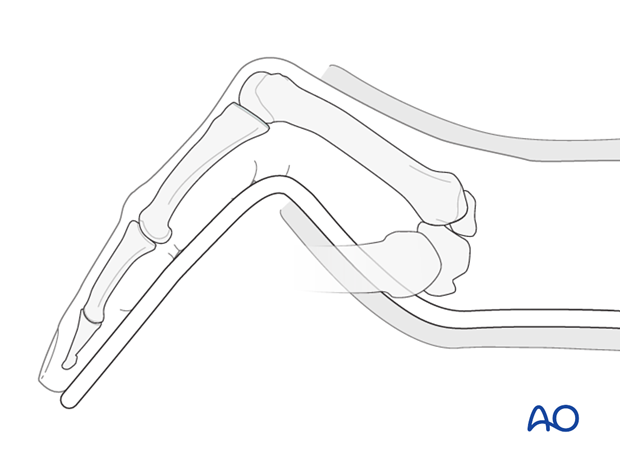
4. Option 2: Immobilization with a forearm cast and finger splint
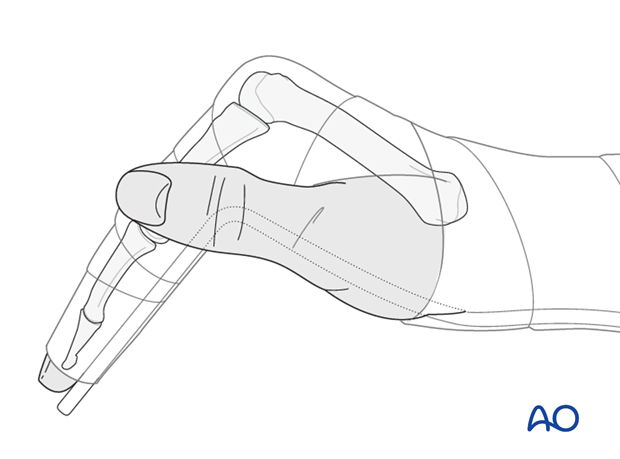
A standard forearm cast is applied, including the wrist joint in 30 degrees of extension, and the aluminium splint is incorporated in the cast. This aluminium splint must be pre-bent to 90 degrees proximal to the level of the MCP joint of the injured finger. The finger is taped to this splint in an intrinsic plus position. Correct rotational alignment must be checked. The other fingers are not immobilized.
The cast must only be applied once the initial swelling has abated, usually a few days after the injury.
Correct bending of the aluminium splint and correct fixation of the splint in the cast are difficult but essential. The bend for the flexion of the MCP joint is more proximal than often perceived. There is a risk of excessive pressure and later ulceration of the soft tissues at the level of the bend if it is too distal.
The advantage of this technique is that only the injured finger is immobilized. Usually hand therapy is not necessary.
Another advantage is that this technique helps maintain length in shortened fractures, but there is less control over rotation than with immobilisation of the adjacent rays (Option 1).
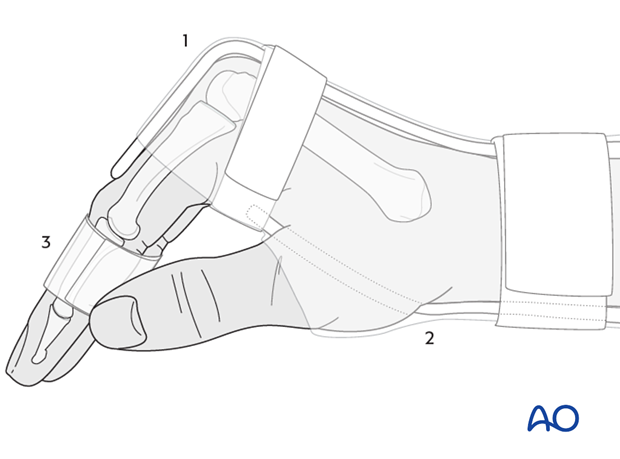
5. Option 3: Attelle fonctionelle
This splint comprises 3 parts:
- A dorsal splint maintaining the wrist in 30 degrees of extension and the MCP joints in full flexion, reaching distally to the PIP joints
- A palmar splint supporting the wrist in 30 degrees of extension, reaching the distal flexion crease of the palm
- A “buddy splintage,” or strapping (syndactylisation), applied at the middle phalanges II-V.
This technique allows immediate mobilization of the interphalangeal joints of all fingers. Its application, however, is difficult, and correct exercising must be supervised by a hand therapist. “Buddy splintage,” prevents rotational malalignment.
6. Aftertreatment
Follow-up
X-ray controls have to be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week, and possibly after 2 weeks.
Immobilization is continued until about 4 weeks after the injury. At that time an x-ray without the splint is taken to confirm healing.
Mobilization
Splinting can then usually be discontinued and active mobilization is initiated. Functional exercises are recommended.
If after 8 weeks radiographs confirm healing, full loading can be permitted.