Lag screw fixation
1. Principles
Indications
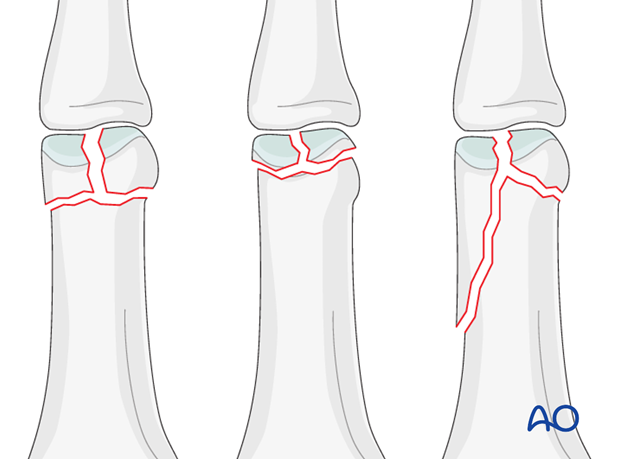
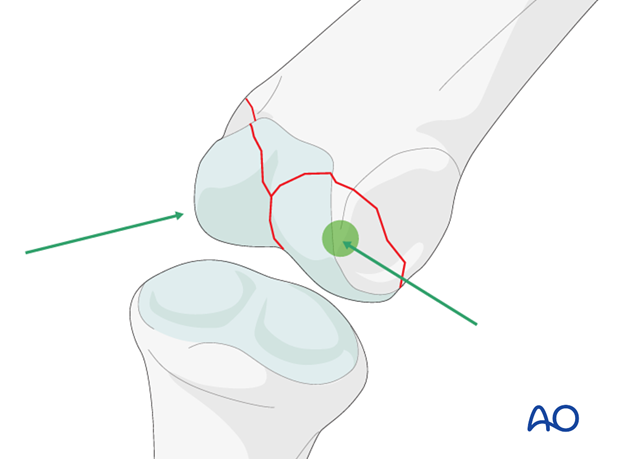
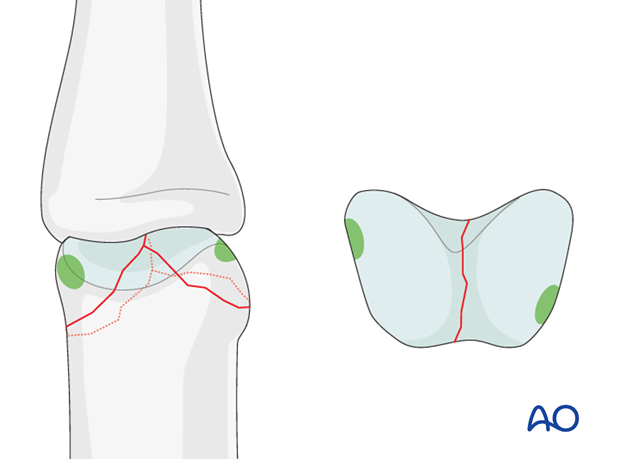
Bicondylar fractures of the head of the proximal phalanx may be T-shaped, with a long or a short T.
Another pattern of fracture is a combination of a long oblique fracture separating one condyle, together with a short oblique, or transverse, fracture separating the other condyle (sometimes called “lambda” fractures, because of their resemblance to the Greek letter “λ“).
Lag screw fixation is indicated both for the short T-shaped and the lambda fractures.
Typically these fractures are the results of sports injuries, due to axial load combined with lateral angulation of the finger.
Condylar fractures tend to be very unstable and should be treated operatively. If nonoperative treatment is attempted, secondary displacement is likely, leading to angulation of the finger.
Caveat
These fractures are rare, but difficult to treat. There is an increased risk of joint stiffness resulting from these fractures.
It is wise to use magnifying loupes in these procedures. Gentle and precise handling throughout the procedure is mandatory.
2. Approach
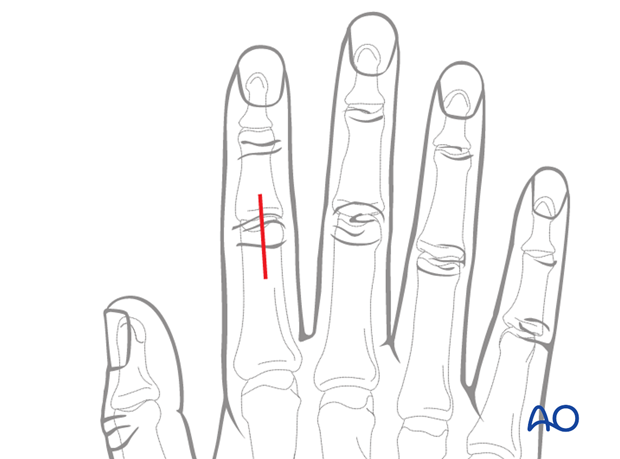
For this procedure dorsal approaches to the PIP joint are normally used.
3. Reduction
Anatomical reduction mandatory
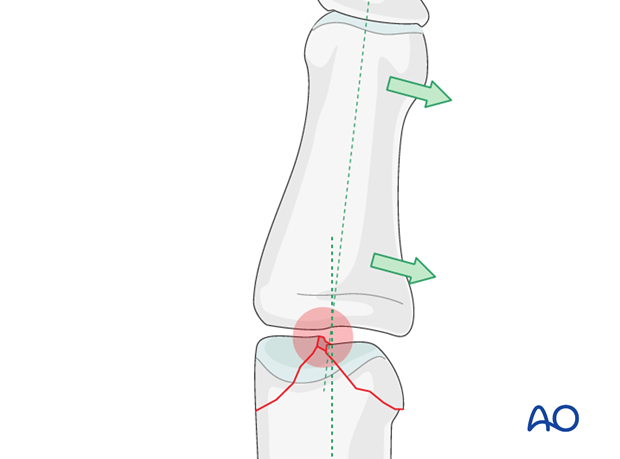
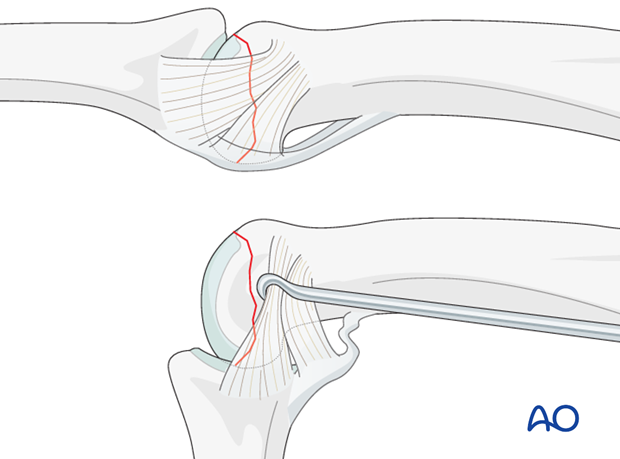
Articular fractures must be reduced anatomically. Otherwise, the articular cartilage may be damaged, leading to painful degenerative joint disease and digital deformity.
This illustration shows how even slight unicondylar depression may lead to angulation of the finger.
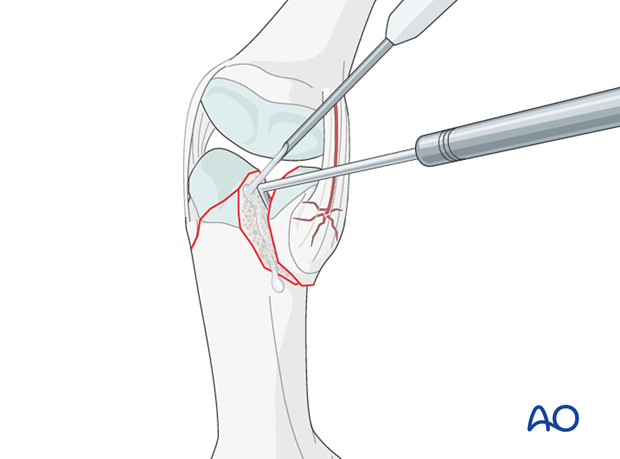
Visualization of the fracture
In order to gain a better view of the fracture, use a syringe to irrigate out blood clot with a jet of Ringer lactate.
Gently explore the fracture site to assess its geometry, using a dental pick. The pick can also be used carefully to reduce small fragments. Take great care to avoid comminution of any fragment.
It is important to maintain the vascularity of tiny fragments attached to the collateral ligament, in order to avoid osteonecrosis.
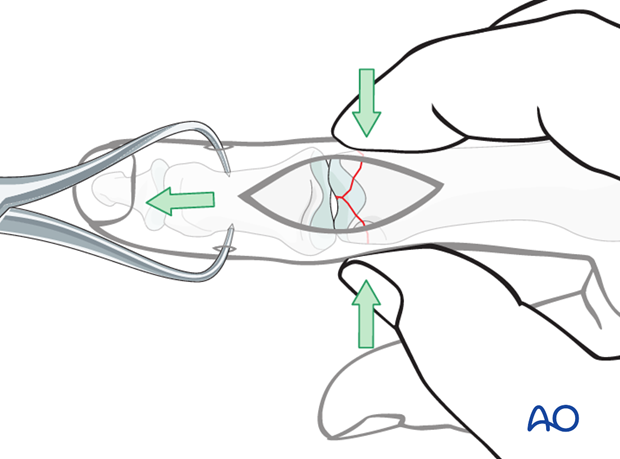
Indirect reduction
Reduction starts with traction in order to restore length.
Lateral pressure, exerted by the surgeon’s thumb and index finger, will then reduce the fracture.
Confirm reduction using image intensification.
4. Preparation
Most of the fracture line on the lateral aspect of the head is covered by the collateral ligament.
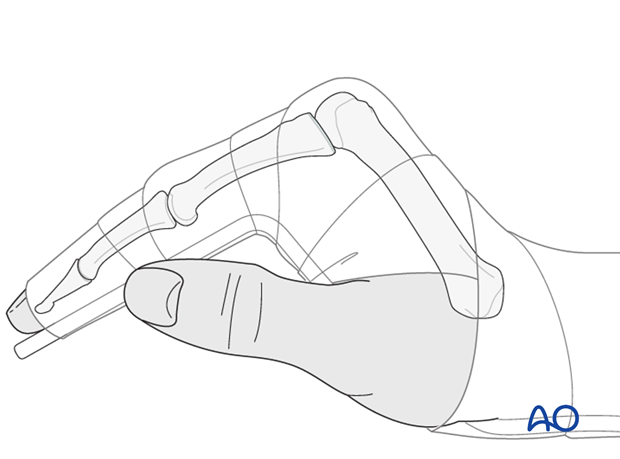
Flexing the PIP joint will draw back the collateral ligament, which can be further retracted with a hook to expose the intraarticular lateral aspects of the condyles.
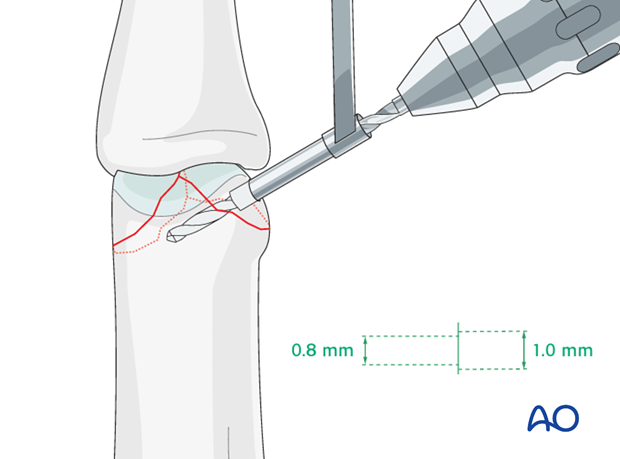
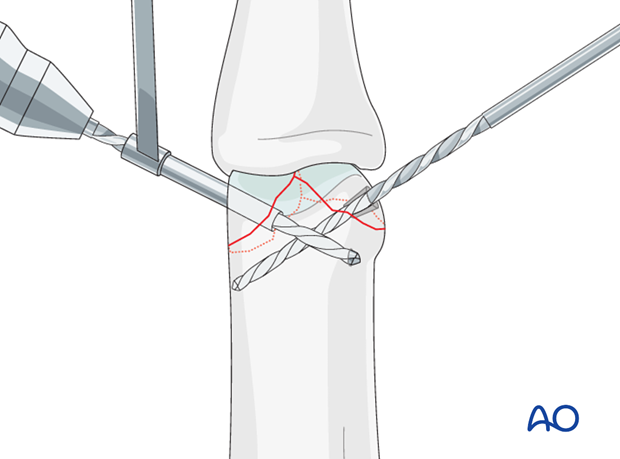
5. Drilling
Location of the drill holes
On the lateral intraarticular aspects of the condyles, there is a small ridge on each side. These are uniquely suited for screw placement, as the screws can be buried deep to the edge of the cartilage without violating the joint surface and avoiding causing irritation.
Hold the condyle in the reduced position with a dental pick. Some surgeons use pressure from the drill guide to hold the reduction during drilling.
Drill a gliding hole as perpendicularly to the fracture plane as possible at the site of this ridge, using a 1.0 mm drill bit for a 1.0 mm screw.
Use a 0.8 mm drill bit to drill a thread hole in the opposite fragment, just through the far (trans) cortex.
With very small fragments, it may be advisable to drill with manual rotation of the bit, rather than a powered driver.
Pearl: use drill bit for temporary fixation
Leave the drill bit in the drill hole to preliminarily hold the fragment in place.
Planning the second screw track
Be careful to drill the screw track in the other condyle at a different level from the track in the opposite condyle. This way the screws will not conflict with each other.
Drill the second condyle
In the second condyle, drill a gliding hole as perpendicularly to the fracture plane as possible, using a 1.0 mm drill bit for a 1.0 mm screw.
Use a 0.8 mm drill bit to drill a threaded hole in the opposite fragment, up to the far (trans) cortex.
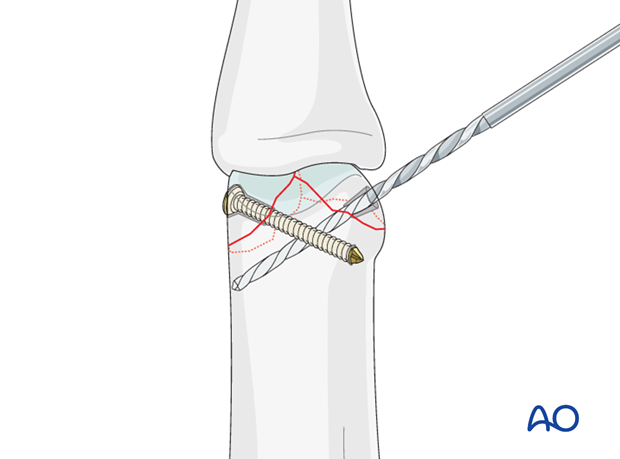
6. Fixation
Insert first lag screw
Remove the drill bit and insert the first lag screw. Carefully tighten the screw to achieve interfragmentary compression.
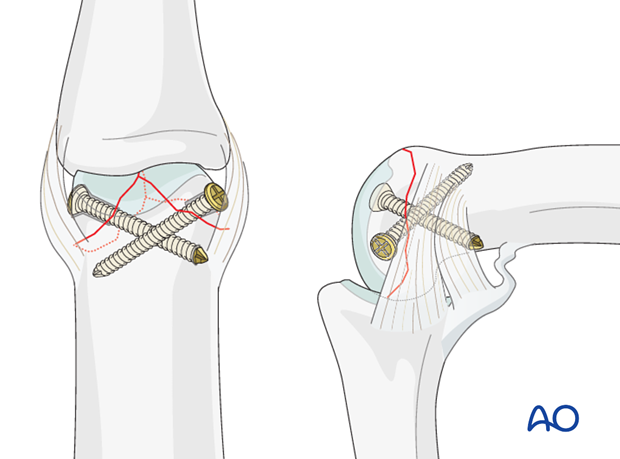
Insert second lag screw
Insert the second lag screw and tighten it.
7. Aftertreatment
Postoperatively
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
Postoperative splint
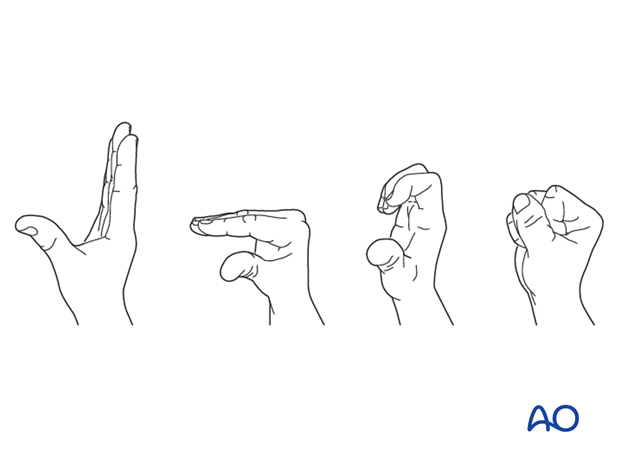
A removable splint may be applied at the end of the operation, with the hand in an intrinsic plus position (“safe” or “Edinburgh” position).
Immobilize the hand in a safe position for 2 weeks.
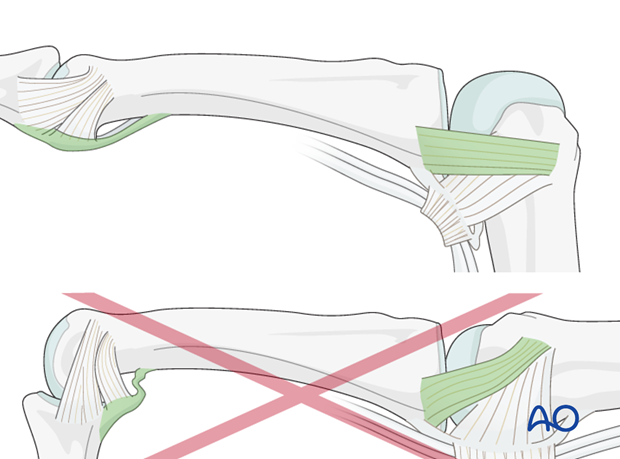
Keep ligament extended
The reason of immobilization of the MP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains length of the volar plate.
Pitfall: scarring
If the collateral ligament develops scarring when not out to length, full extension will become impossible.
Similarly, immobilizing the PIP joint in flexion, can result in scar contraction of the volar plate, also limiting joint extension.
Follow-up
See patient 5 days after surgery to check the wound, clean and change the dressing. After 10 days, remove the sutures. Check x-rays.
Functional exercises
The fixation will be vulnerable for the first 2 weeks.
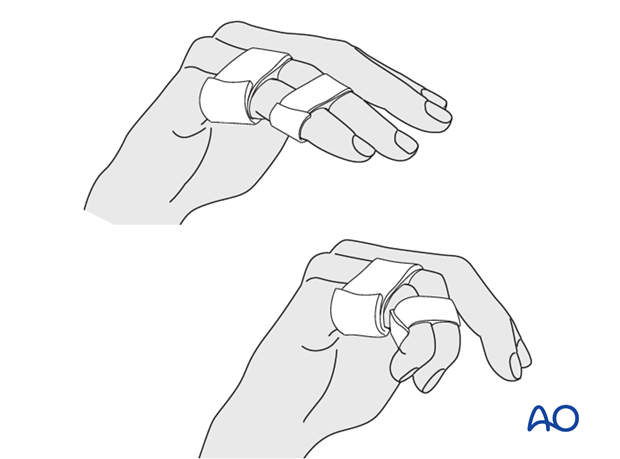
At this stage, remove the splint, and apply buddy strapping. Then begin with active motion exercises.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesion’s restricting finger movement, tenolysis, or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.













