Nonoperative treatment
1. Introduction
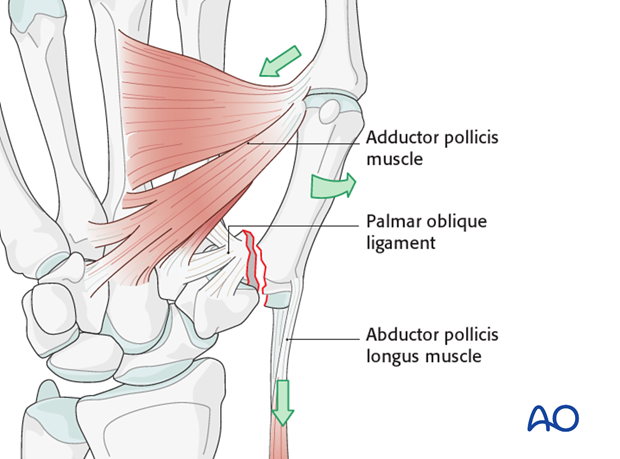
Bennett’s injury is a fracture subluxation of the first carpo-metacarpal joint. The causative mechanism is axial overload along the first metacarpal, combined with simultaneous flexion. The palmar oblique ligament holds the palmar marginal fragment in its anatomical position.
The first metacarpal is adducted and supinated by adductor pollicis. The metacarpal as a whole is also displaced proximally by the abductor pollicis longus muscle.
The treatment goals are to reposition the first metacarpal in the carpo-metacarpal joint, and to restore the articular surface.

Teaching video
AO teaching video: Application of the thumb spica
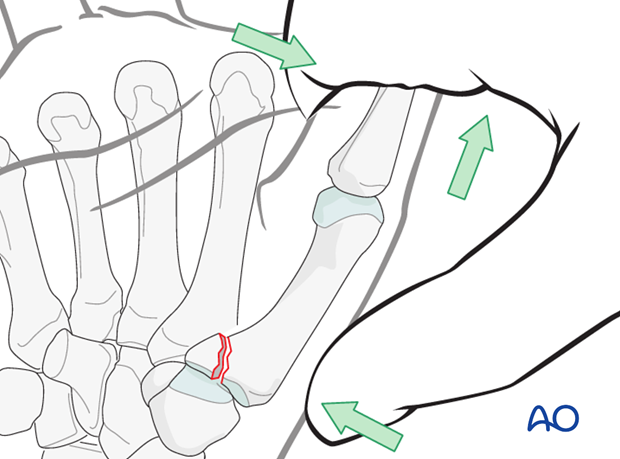
2. Closed reduction
Reduction is performed by a combination of
- longitudinal traction
- pronation of the metacarpal
- pressure at the thumb metacarpal base.
Confirm correct restoration of the articular surface using image intensification.
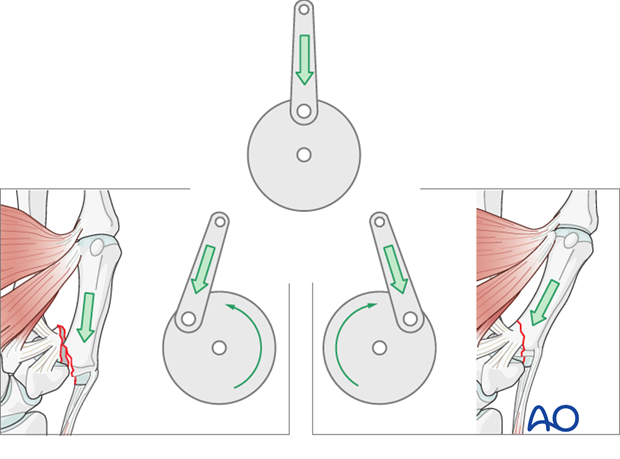
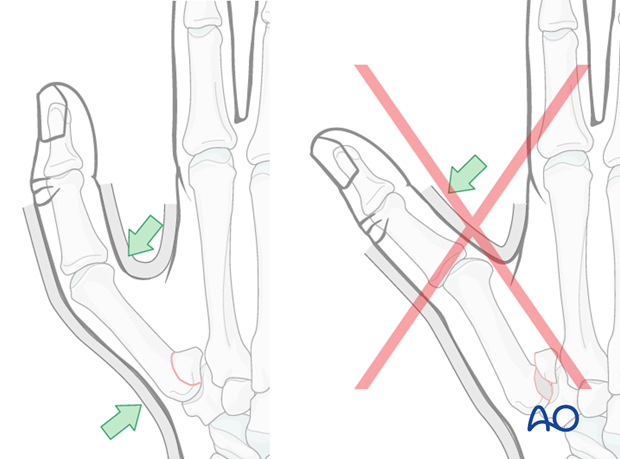
3. Reduction principles
Bennett’s fracture possesses considerable potential stability. If the carpo-metacarpal joint is held in extension, thus tightening the palmar ligaments, the reduction will be stable and dorsal redisplacement is unlikely to occur.
John Charnley* likened the mechanics of this situation to the crank and connecting rod of an engine: treatment by traction is comparable to the crank standing at “top dead center”. This leaves the bone in in a state of “uncertain equilibrium”.
Without traction (as represented on the bottom left of our illustration), muscular tone can induce complete dislocation if the thumb is allowed to flex.
However, when the thumb is in extension (bottom right of our illustration), the muscle tone will increase the stability of the reduction by generating pressure against the undisplaced fragment and thrusting the bone deeper into the carpo-metacarpal socket.
* Charnley, J. (1957) The closed treatment of common fractures. Edinburgh, London: Churchill Livingstone, 144
4. Applying cast
Maintaining reduction
During the application of the plaster, it is important to exert pressure from the dorsal aspect onto the first metacarpal base, and from the palmar aspect over the first metacarpal head.
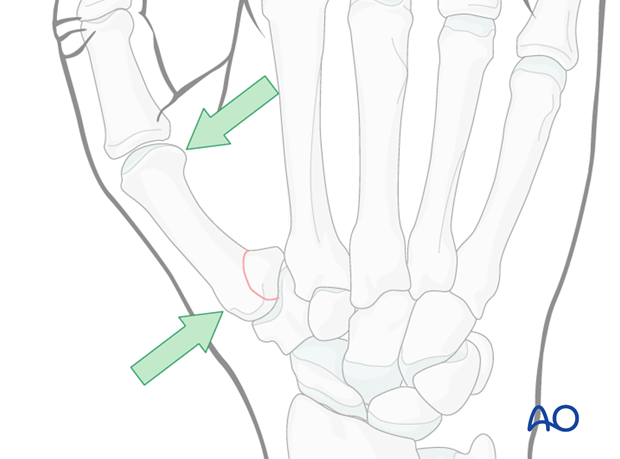
Pitfall: palmar pressure
Avoid pressing from the palmar side onto the base of the proximal phalanx. This results in redisplacement of the fracture and hyperextension of the MCP joint.
Apply the cast
Immobilize the wrist in a well-padded below-elbow cast with the wrist slightly extended, and the thumb immobilized in a position of slight abduction, with appropriate moulding of the cast.
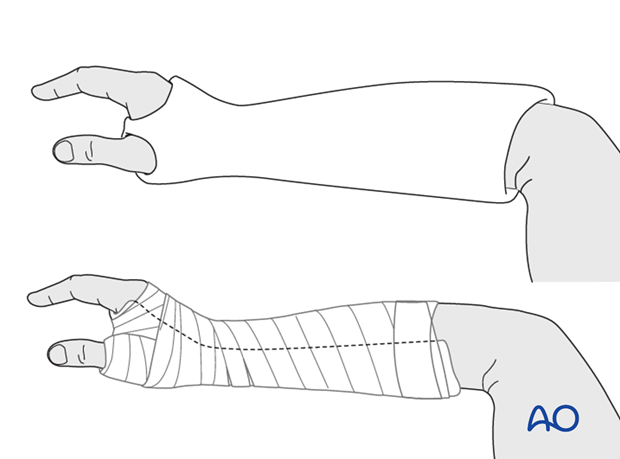
Make sure that the cast does not extend too far distally, either at the level of the finger metacarpophalangeal joints (MCP) or the interphalangeal joint of the thumb. The cast must not limit complete flexion of these joints.
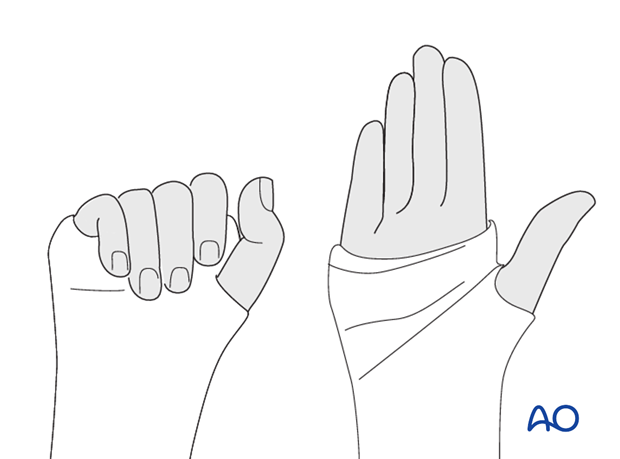
5. Aftertreatment
Confirm reduction by radiographs after the cast has been applied. Repeat radiographs at weekly intervals to check the fracture reduction. Usually, immobilization for a 6 week period is sufficient.
The patient is instructed to exercise the MCP joints and interphalangeal joints regularly.














