K-wire fixation
1. Introduction
Bennett’s injury is a fracture subluxation of the first carpo-metacarpal joint. The causative mechanism is axial overload along the first metacarpal with simultaneous flexion. The palmar oblique ligament holds the palmar marginal fragment in its anatomical position.
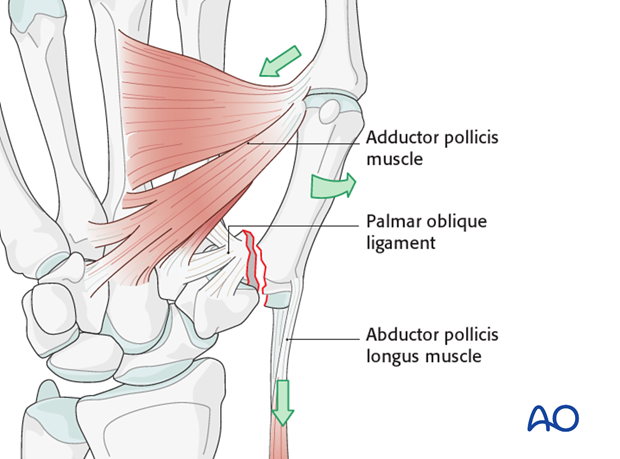
The distal part of the first metacarpal is adducted and supinated by adductor pollicis. The metacarpal as a whole is also displaced proximally by the abductor pollicis longus muscle. The treatment goals are to reposition the first metacarpal in the carpo-metacarpal joint, and to restore the articular surface.

Treatment options
- Conservative treatment
Indicated for undisplaced fractures. - Closed reduction and internal fixation
Indicated for reducible fractures. - Open reduction internal fixation (ORIF)
Indicated for fractures which are not reducible in a closed manner.
ORIF is also indicated in high-demand patients and those who need immediate restoration of a full range of motion. However, ORIF is possible only if the anterior marginal fragment is large enough for internal fixation (>20% of the articular surface).
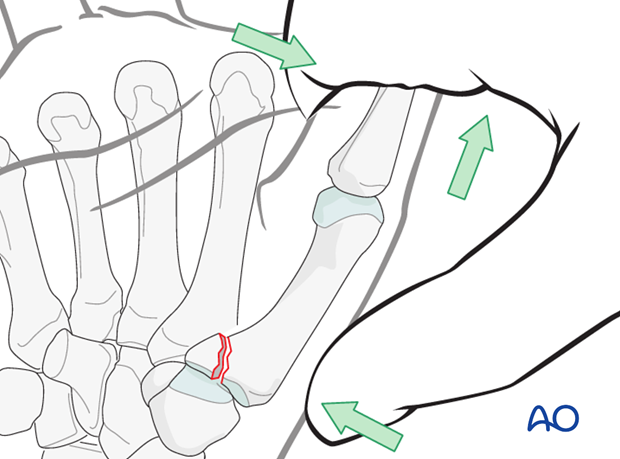
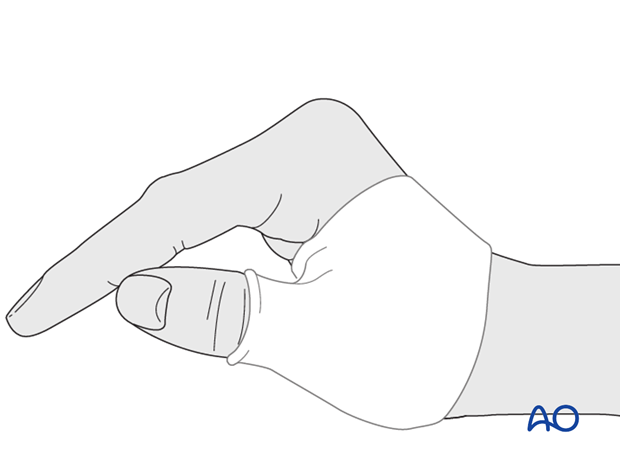
2. Closed reduction
Reduction is performed by a combination of
- longitudinal traction
- pronation of the metacarpal
- pressure at the thumb metacarpal base.
Confirm correct restoration of the articular surface using image intensification.
3. Internal fixation
Closed reduction and internal fixation comprise the treatment of choice for most of Bennett’s fractures.
There is a number of possibilities for internal fixation. The most common are:
- transfixion of the base of the first metacarpal to the trapezium
- transfixion of the thumb base to the second metacarpal
- combination of both
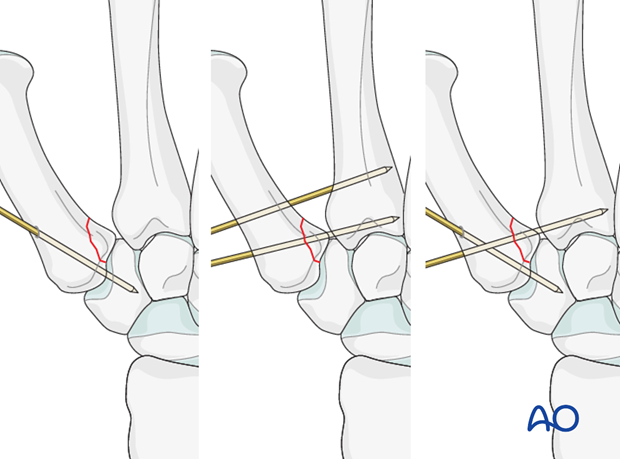
1.6 mm K-wires are used. They may be cut off below the skin, or left protruding through the skin.

4. Pearls
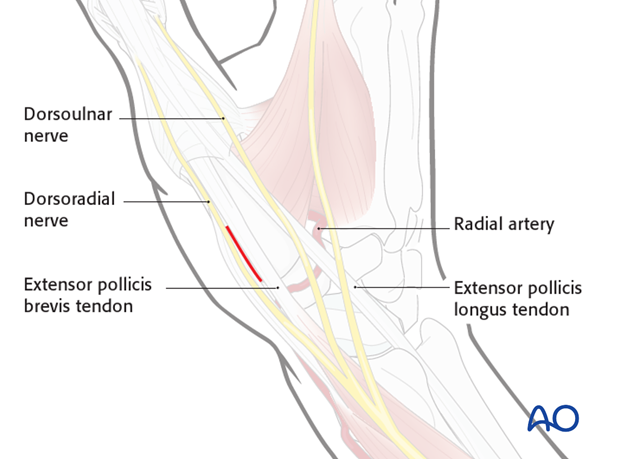
Protect soft tissues by blunt dissection
Make a 1 cm long dorsal skin incision over the base of the thumb before insertion of the K-wire.
Using blunt dissection, protect the cutaneous branch of the radial nerve and the tendons. Damage to the cutaneous nerve can cause a painful neuroma.
X-rays are necessary before the end of the operation to check that the articular surface is anatomically reduced. Fluoroscopy is inadequate for a final evaluation.
If reduction is not anatomical, proceed to an open operation.
5. Aftertreatment
Orthoplast splint
In compliant patients, a well-padded orthoplast splint is sufficient for immobilization. This has the advantage of leaving the wrist free.
Thumb spica
In noncompliant patients, a more restrictive well-padded thumb spica may be a wiser choice.
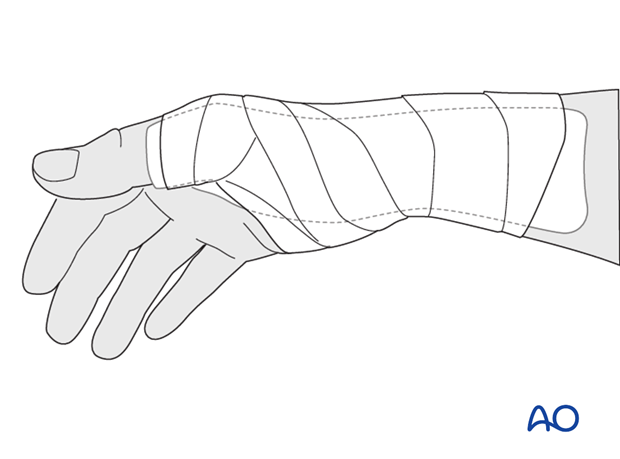
Protruding K-wires: cleaning
In the case of protruding K-wires, instruct the patient how to clean the wound every second day. For this, a window must be cut in the cast, or splint, at the sites of the K-wires.
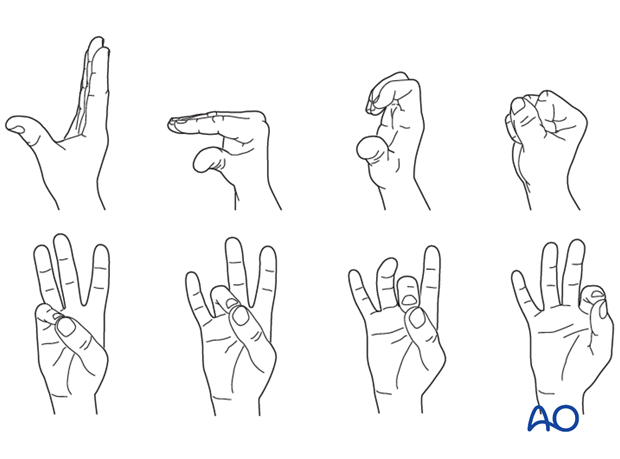
Immobilization and functional exercises
4-6 weeks of immobilization are necessary.
During this time, flexion and extension exercises of the MP, PIP and DIP joints of the phalanges are performed.
After 4-6 weeks, the K-wires are removed as an outpatient procedure.
Opposition of thumb to the other fingers is now performed.
Heavy manual demand and all activities involving a strong grip are not permitted until complete fracture healing (usually after 3 months).
Teaching video
AO teaching video: Application of the thumb spica













