Nonoperative treatment
1. Principles
Most fractures of the distal phalanx can be treated nonoperatively.
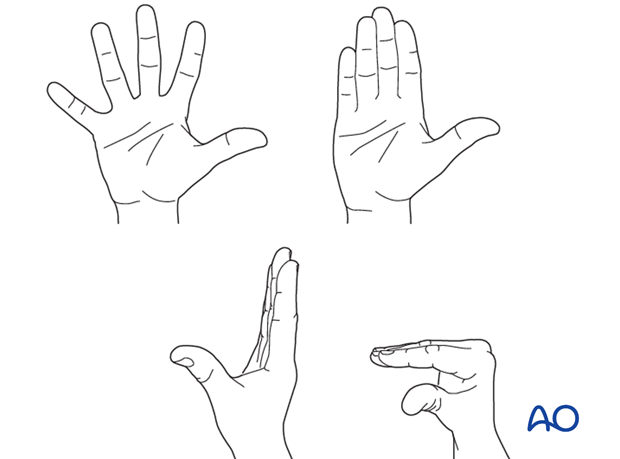
Nonoperative treatment is based on immobilization of the DIP joint in extension, leaving the PIP joint free.
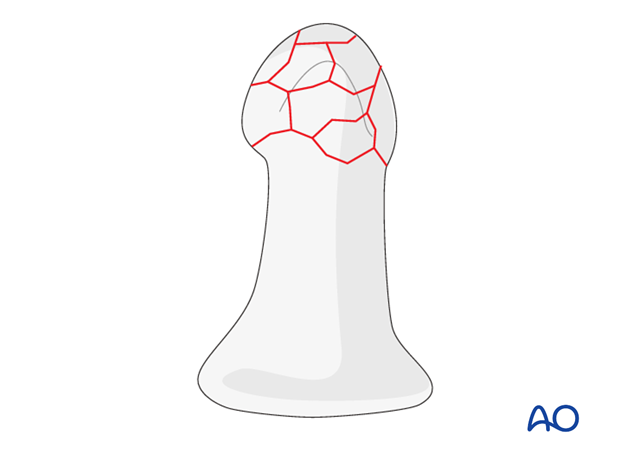
Fractures of the distal phalanx are often the result of direct impact, or crush injuries. Most frequently, there is a comminuted tuft fracture.
Nail bed injuries may need repair and reduction of the nail plate into the nail fold.
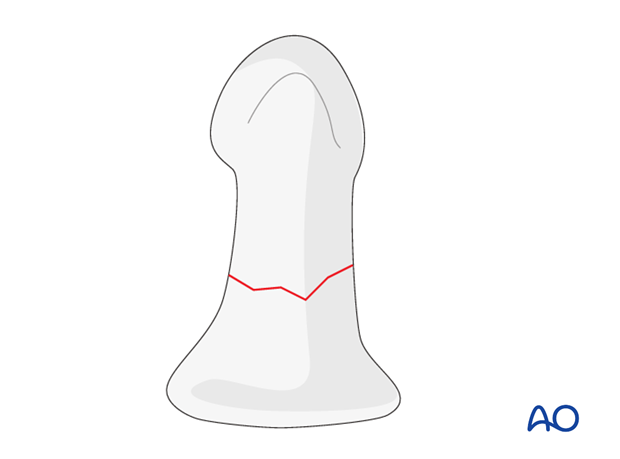
Transverse fractures of the proximal half of the distal phalanx are not well-suited to nonoperative treatment when there is no direct contact between the fragments. These fractures are often unstable and, in open fractures, the nail bed is often folded into the fracture. In these cases, open reduction and internal fixation are indicated.
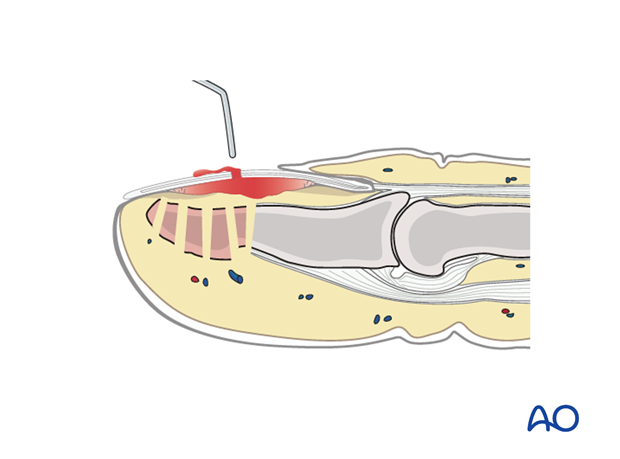
2. Release of subungual hematoma
Closed crush injuries are often accompanied by a tense subungual hematoma, which can be exceedingly painful, due to the pressure within the closed space.
The hematoma can easily be released by puncturing the nail with a red-hot needle, or paperclip end.
If no further treatment is indicated, apply a simple splint and cool the finger with the judicious use of an ice pack.
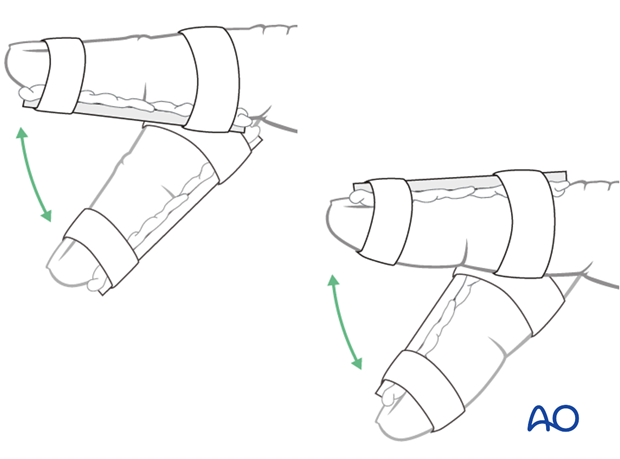
3. Splinting options
Dorsal splint versus palmar splint
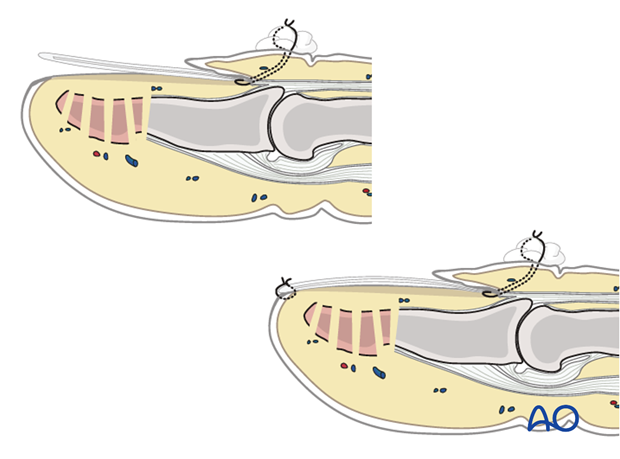
Using a dorsal splint has the advantage of leaving the patient with the ability to pinch while the digit is immobilized.
However, proponents of palmar splintage argue that the palmar aspect is better cushioned than the dorsal and, thereby, can tolerate the splint better.
Contoured custom thermoplastic splint
The advantage of a custom thermoplastic splint is that it is adapted better to the shape of the finger, and easier to change.

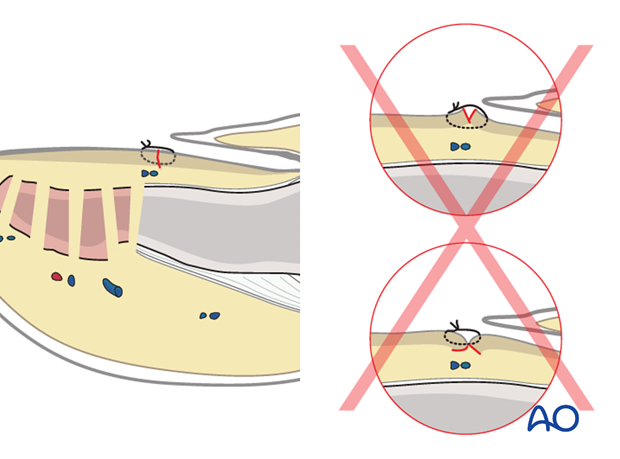
Pitfall: immobilization of the PIP joint
Do not immobilize the PIP joint.

4. Repair of the nail bed
It is advisable precisely to repair the nail bed, or the germinal matrix, lest permanent deformity of nail growth occur.
Such procedures are difficult, without the help of magnifying loupes. In many cases, an operating microscope is an even better choice, if available.
Separate fine absorbable sutures should be used.
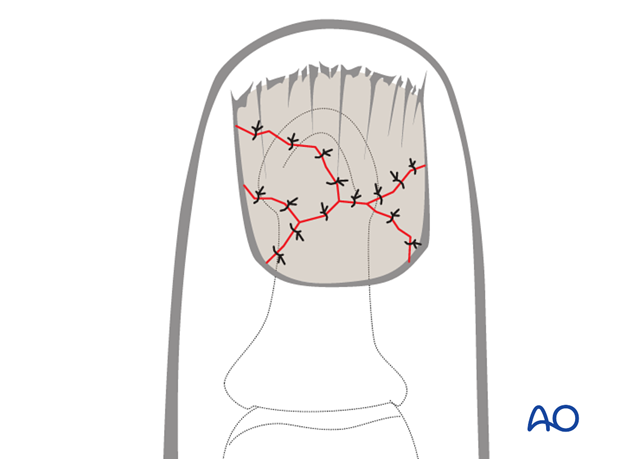
In simple transverse, or oblique, lacerations of the nail bed, a running suture may be used.
Pitfall: Eversion or inversion of nail bed edges
Be careful to suture the edges of the nail bed, avoiding eversion or inversion, otherwise, permanent deformity of nail growth can result.
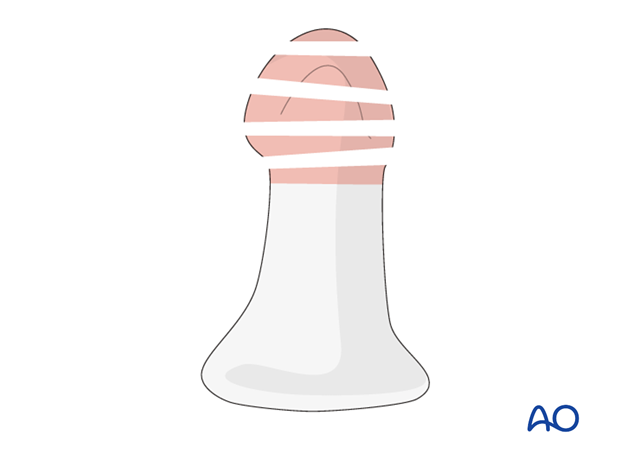
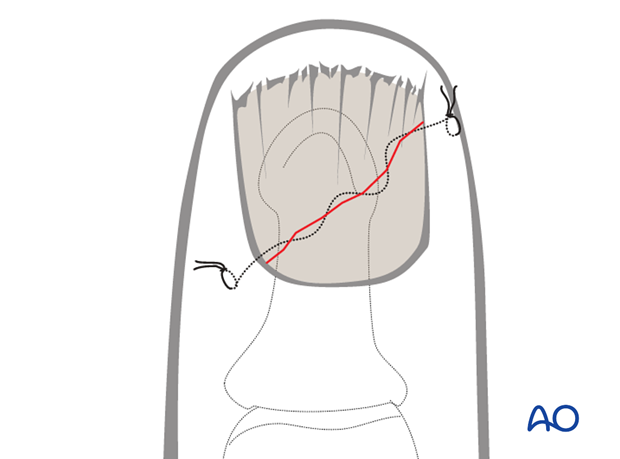
5. Reinsertion of the nail
There are 4 main reasons for nail reinsertion:
- to prevent scarring between the eponychium and the germinal matrix
- to stabilize the fracture
- the nail acts a biological barrier and protection
- it acts as a template for the growth of a new nail.
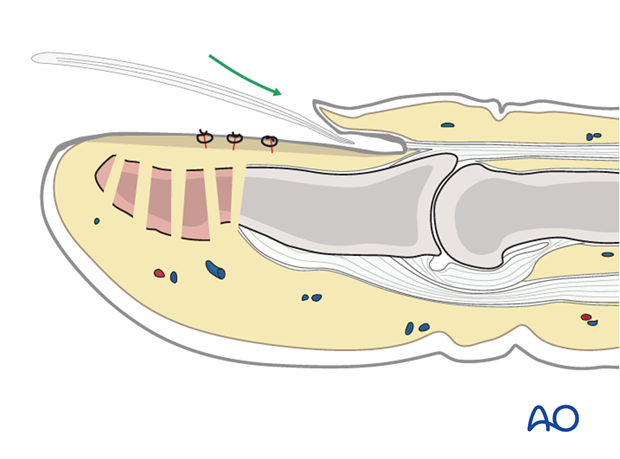
Insert a needle with a 5-0 nonresorbable nylon suture from the dorsal aspect into the sinus, exiting the sinus distally to the eponychium.
Pass the needle through the proximal edge of the nail plate.
Then pass the needle back through the nail plate and the sinus of the nail, so that it exits level with the first pass of the suture, separated from it by approximately 5 mm.
Draw the nail plate back into the sinus by gentle traction on both ends of the suture.
Tie the suture over a cotton, or foam, ball to avoid skin pressure injury.
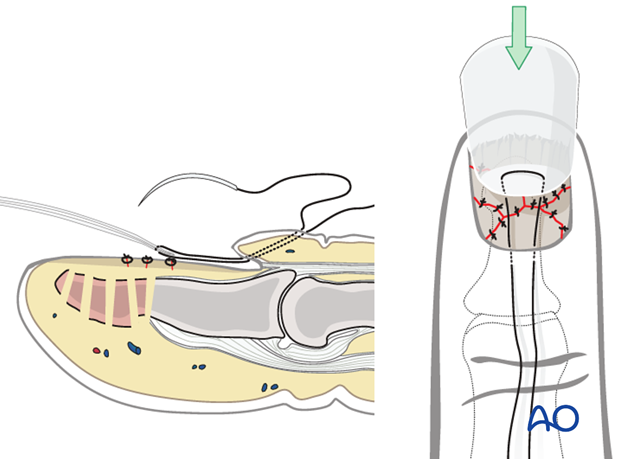
After reinsertion and proximal fixation, the nail has a tendency to tilt upwards distally.
To prevent this, use a small suture at the nail’s distal tip to secure it to the nail bed.
6. Aftertreatment
Cleaning
Removal of the splint and skin care must be performed by the patient in 1-2 day intervals.
Functional exercises of the nonimmobilized joints can be started immediately.
Duration of immobilization
X-ray controls have to be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week, and possibly after 2 weeks. Immobilization is continued until about 4 weeks after the injury. At that time an x-ray without the splint is taken to confirm healing. Splinting can then usually be discontinued and active mobilization is initiated.
If after 8 weeks radiographs confirm healing, full loading can be permitted.
Tuft fractures
In tuft fractures, splinting is mainly performed for pain treatment, and usually after 3 weeks, the splint can be discontinued. These injuries do not necessarily need x-ray control.