Distal phalanx, distal and shaft, transverse
Comminuted fractures
Fractures of the distal phalanx are the most common fractures in the hand.
Most frequently, the thumb, the middle finger, or somewhat less often, the index finger is injured.
Common complications of these injuries are:
- altered sensibility (numbness, hyperesthesia, tenderness)
- cold hypersensitivity (cold intolerance)
- restriction of DIP joint movement
- nail growth abnormalities
The vast majority of these fractures result from crush injuries with associated soft-tissue (nail bed, or pulp) lacerations.
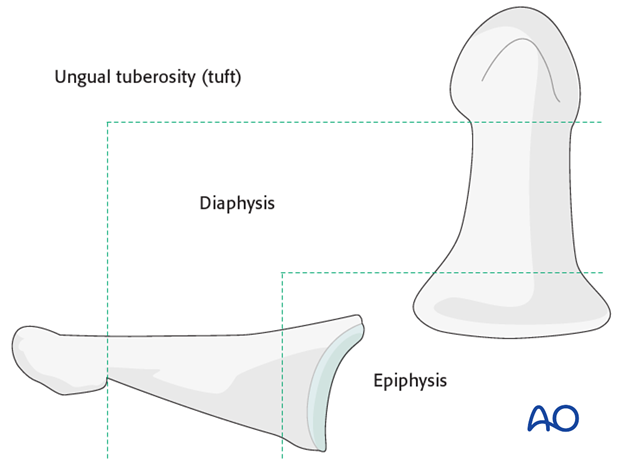
Anatomy
The distal phalanx is divided into three anatomical zones: most proximally the epiphyseal region (base), followed by the diaphysis (“waist”), and finally the ungual tuberosity (“tuft”).
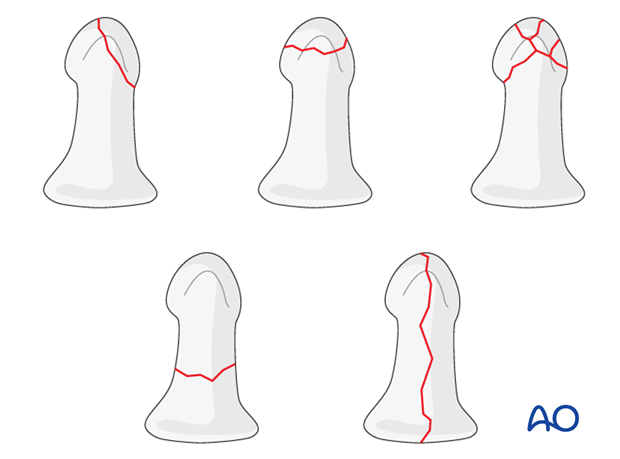
Classification of distal phalangeal fractures (after Schneider)
Schneider divides distal phalangeal fractures into tuft fractures, shaft fractures and articular fractures.
Tuft fractures include
- simple fractures
- comminuted fractures
Shaft fractures include
- transverse fractures
- longitudinal fractures (may extend to involve the DIP joint)
Articular fractures include
- palmar (flexor digitorum profundus avulsion fractures)
- (Epiphyseal (basal) separations –considered by Salter-Harris classification, to follow)
- dorsal (extensor avulsion, mallet fractures)
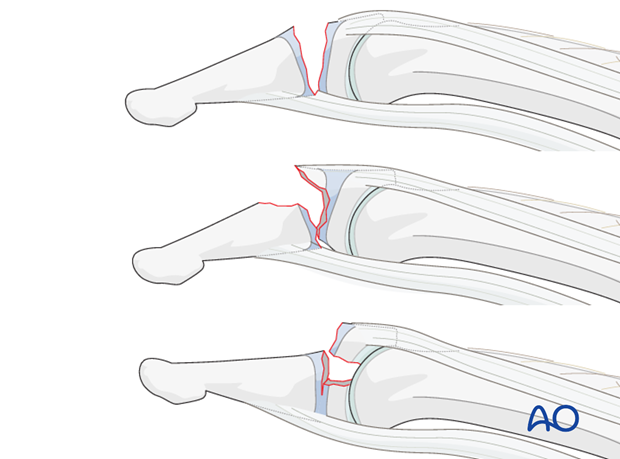
Intraarticular pediatric fractures after Salter-Harris
In children, three injury types are classified:
Type I: Shearing through the growth plate.
Type II: Shearing through most of the growth plate with tiny, triangular-shaped fracture fragment from the dorsal aspect of the distal phalangeal metaphysis.
Type III: Fracture across the epiphysis, exiting through the growth plate.
Diagnosis
The majority of fractures of the distal phalangeal diaphysis are closed and either undisplaced, or minimally displaced.
If these fractures are stable, they can be treated nonoperatively with splintage.
Crush injuries often have associated soft-tissue lacerations. Some of these are open fractures.
Fractures of the diaphysis can be transverse, oblique, or comminuted.
Obliquity of the fracture may occur either in the plane visible in the AP view, or in the plane visible in the lateral view. Always confirm the fracture configuration with views in both planes.
Diagnosis is based on:
- linical history of the trauma and mechanism of the injury
- clinical examination of the patient
- x-rays
AP and lateral x-rays are necessary for diagnosis. Be careful to avoid superimposition of other fingers in the x-rays.
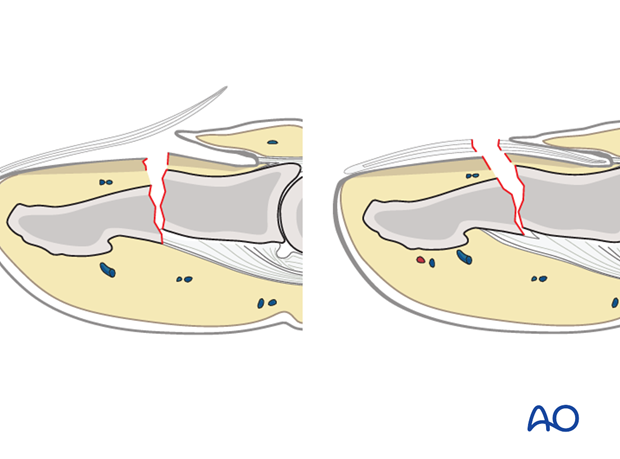
Recognizing nail-bed injuries
Closed fractures may look harmless on x-rays, but in the majority of cases, the nail bed has been torn.
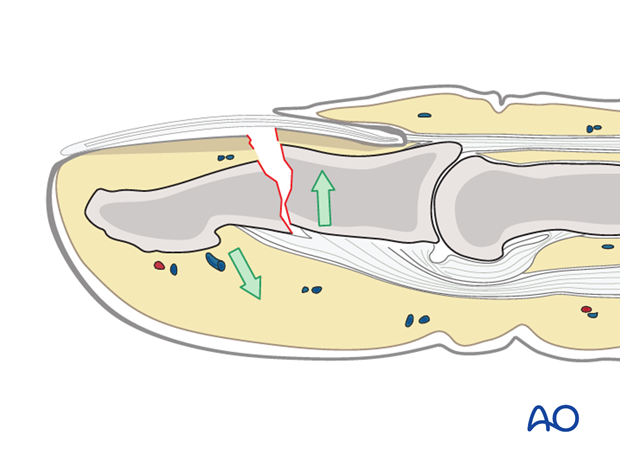
Flexor and extensor tendons displace the fracture with a typical palmar angulation of the tuft fragment.
Open fractures
Open fractures present in two ways: with an avulsed nail plate, or with a fractured nail.
In both types, the fracture opens dorsally, and the nail bed is also injured.
It is mandatory precisely to repair the nail bed. Otherwise, permanent deformity of the nail growth can result.
These procedures are very difficult to conduct successfully without the help of magnifying loupes.
The general principles for treating all open fractures apply. As the majority of these injuries are due to crushing, edema of the soft tissues is most likely to develop and primary closure of any associated skin lacerations is not advisable.