K-wire fixation
1. Principles
Fractures of the distal phalanx are the most common fractures in the hand.
Most frequently, the thumb, the middle finger, or somewhat less often, the index finger is injured.
Common complications of these injuries are:
- altered sensitivity (numbness, hyperesthesia, tenderness)
- cold sensitivity (cold intolerance)
- restriction of DIP joint movement
- nail growth abnormalities
The vast majority of fractures result from crush injuries with associated soft-tissue (nail bed, or pulp) lacerations.
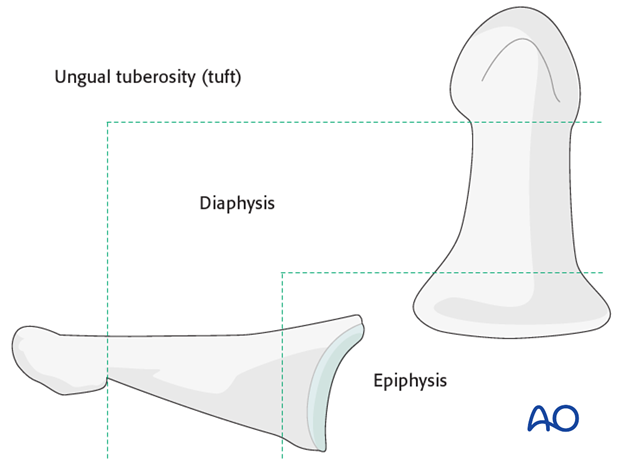
Anatomy
The distal phalanx is divided into three anatomical zones: most proximally the epiphysis, followed by the diaphysis (“waist”), and finally the ungual tuberosity (“tuft”).
Classification of distal phalangeal fractures (after Schneider)
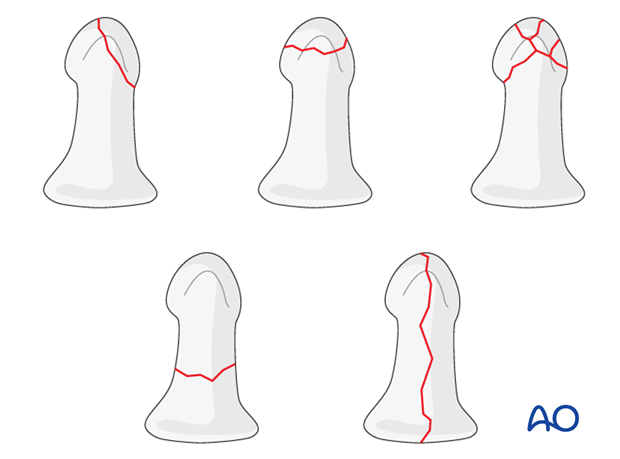
Schneider divides distal phalangeal fractures into tuft fractures, shaft fractures and articular fractures.
Tuft fractures include
- simple fractures
- comminuted fractures
Shaft fractures include
- transverse fractures
- longitudinal fractures
Articular fractures include
- palmar (flexor digitorum profundus avulsion fractures)
- dorsal (extensor avulsion, mallet fractures)
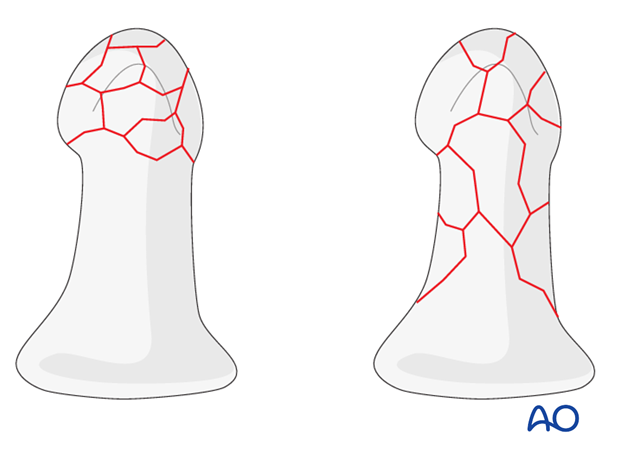
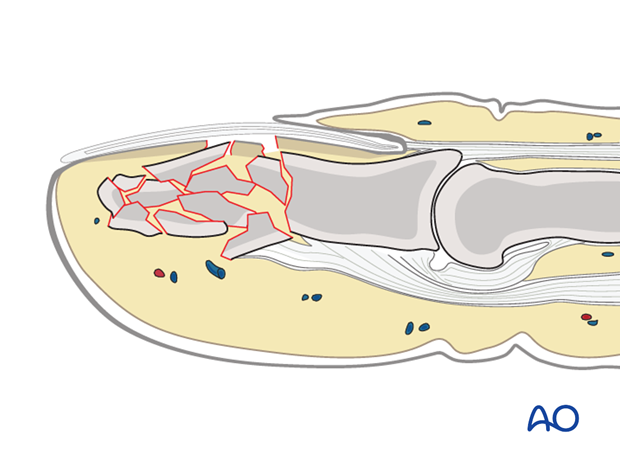
Multifragmentary fractures
In multifragmentary fractures, the comminution may be limited to the tuft, or it may extend into the diaphysis.
Treatment of crush injuries
In comminuted crush injuries, treatment of the fracture is of secondary importance. More important is soft-tissue management, i.e. of the pulp and of the nail matrix.
After repair of these structures and nail reinsertion, usually the fracture is already stable enough (with the soft-tissue repairs acting as a splint).
Bear in mind that crush injuries cause marked soft-tissue swelling and edema. Any suture repair should be a loose approximation of the edges only.
Fixation options
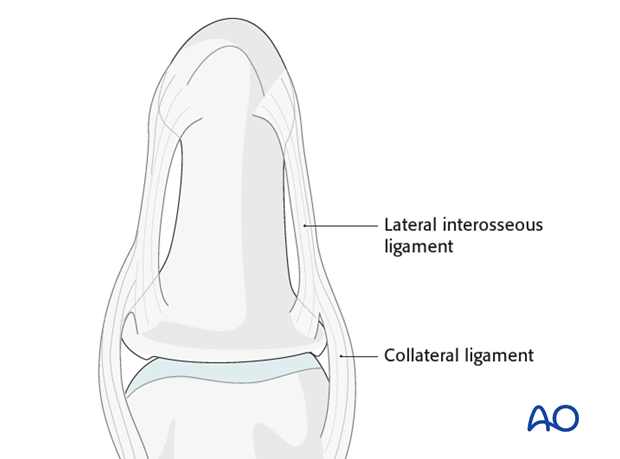
Multifragmentary fractures of the distal phalanx will often heal without complications due to the intrinsic stability provided by the soft tissues. The nail matrix, lateral interosseous ligaments and the fibrous septa are the main stabilizing structures. Therefore, simple splinting often provides adequate stability after soft-tissue repair.
Unstable, or displaced, fractures should be fixed internally with 1 or 2 K-wires, in order to prevent subsequent malunion, nonunion, or other complications such as nail deformity.
2. Diagnosis
The majority of comminuted fractures of the distal phalanx are crush injuries.
Crush injuries often have associated soft-tissue lacerations. Some of these are open fractures.
Diagnosis is based on
- the clinical history of the trauma and mechanism of the injury
- the clinical examination of the patient
- the x-rays
AP and lateral x-rays are necessary for diagnosis. Be careful to avoid overlap of other fingers in the x-rays.
Recognizing nail-bed injuries
Closed fractures may look harmless on x-rays, but in the majority of cases, the nail bed has been torn.
Flexor and extensor tendons displace the fracture with a typical palmar angulation of the tuft fragment.
Open fractures
Open fractures present in two ways: with an avulsed nail plate, or with a fractured nail.
In both types, the fracture opens dorsally, and the nail bed is also injured.
It is mandatory precisely to repair the nail bed. Otherwise, permanent deformity of the nail growth can result.
These procedures are very difficult to conduct successfully without the help of magnifying loupes.
The general principles for treating all open fractures apply. As the majority of these injuries are due to crushing, edema of the soft tissues is most likely to develop and primary closure of any associated skin lacerations is not advisable.
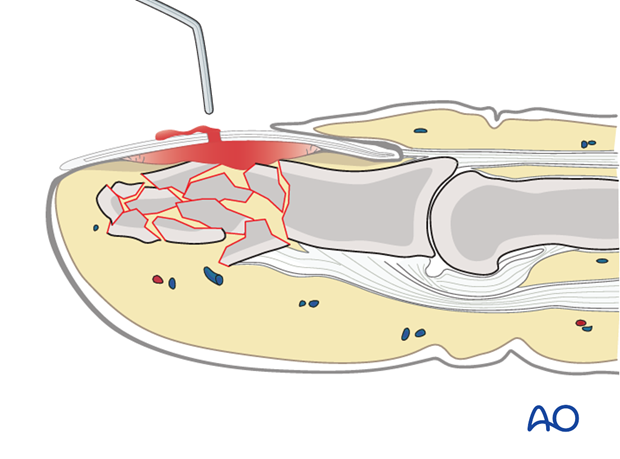
3. Release of subungual hematoma
Closed crush injuries are often accompanied by subungual hematoma which can be exceedingly painful, due to the pressure within the closed space.
The hematoma can easily be released by puncturing the nail with a red-hot needle, or paperclip.
If no further treatment is indicated, apply a simple splint and cool the finger with judicious use of an ice pack.
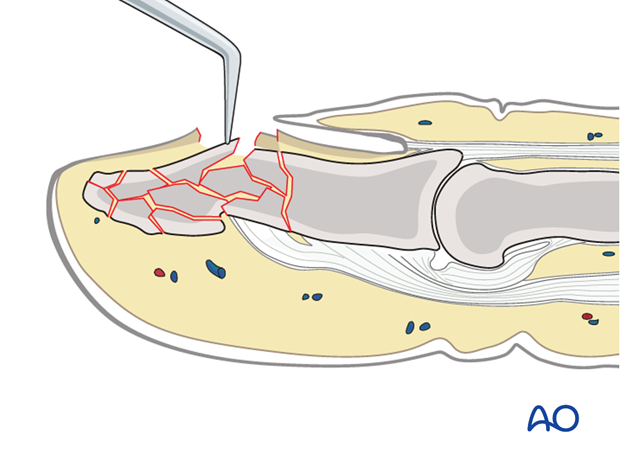
4. Open reduction
In cases of open fracture, clear the fracture site of blood clot and debris.
Use a dental pick carefully to reduce any displaced fracture fragments.
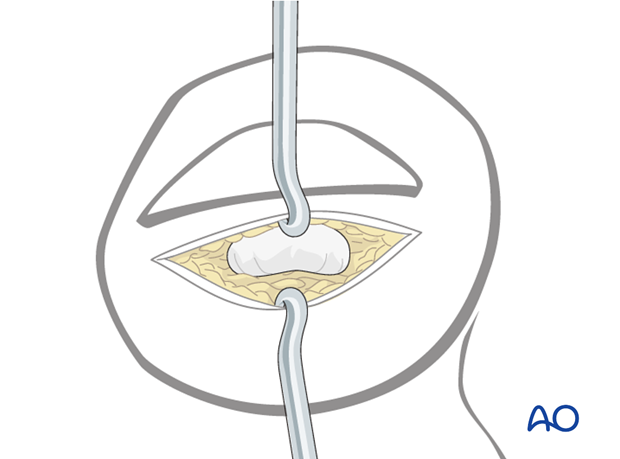
5. Repair of the nail bed
It is advisable precisely to repair the nail bed or the germinal zone, otherwise, permanent deformity of the nail growth can result.
These procedures are difficult to conduct successfully without the help of magnifying loupes. In many cases, an operating microscope is a good choice.
Separate stitches using 8.0 absorbable suture material should be used.
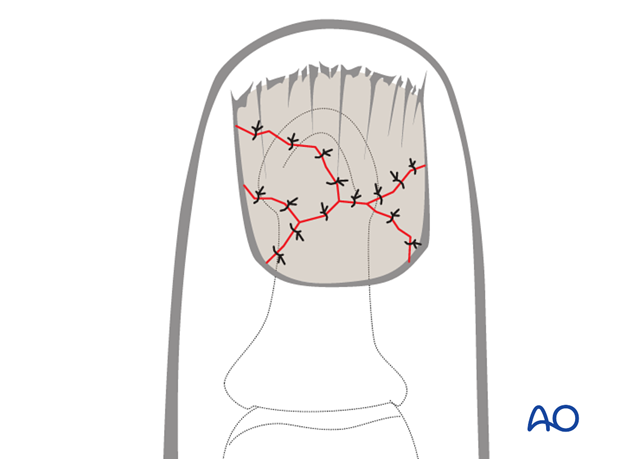
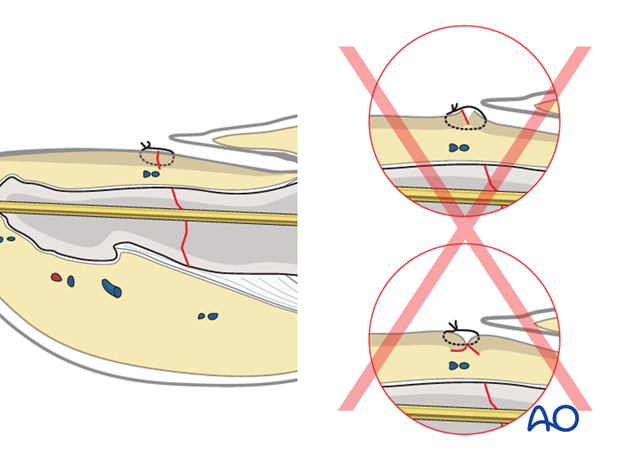
Pitfall: Eversion or inversion of nail bed edges
Be careful to suture the edges of the nail bed, avoiding eversion or inversion, otherwise, permanent deformity of nail growth can result.
Reinsertion of the nail
Now reinsert the nail.
There are 4 main reasons for nail reinsertion:
- to prevent scarring between the eponychium and the nail matrix
- to stabilize the fracture
- the nail acts a biological barrier and protection
- it acts as a template for the growth of a new nail

If sinus is damaged
In some patients, the sinus is injured in such a way that it can not retain the nail plate in position and the nail plate is gently drawn into the sinus using a suture.
Insert a needle with a 5 (0) nonresorbable nylon suture from dorsal into the sinus, exiting the sinus distally to the eponychium.
Pass the needle through the proximal edge of the nail plate.
Then pass the needle back through the nail plate and the sinus of the nail, so that it exits parallel to the first pass of the stitch, separated from it by approximately 5 mm.
Draw the nail plate back into the sinus by gentle traction on both ends of the suture.
Tie the suture over a cotton, or foam, ball to avoid skin pressure injury.
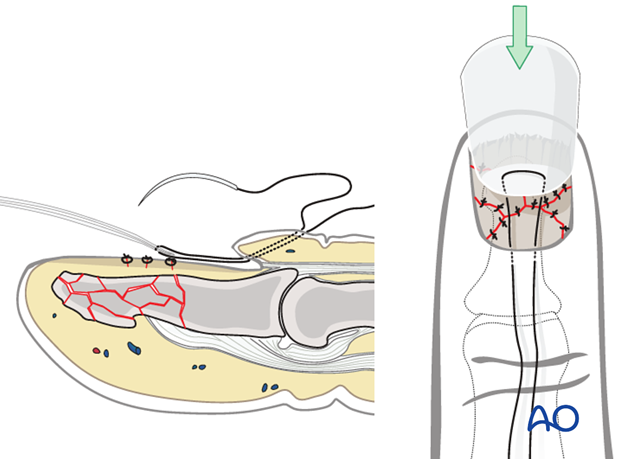
Secure distal nail tip
After reinsertion, the nail has a tendency to tilt upwards distally.
To prevent this, use a small suture at the nail’s distal tip to secure it to the nail bed.
6. Preparation and approach
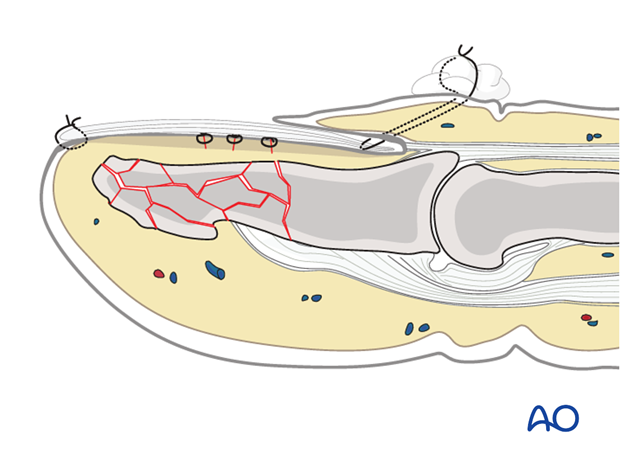
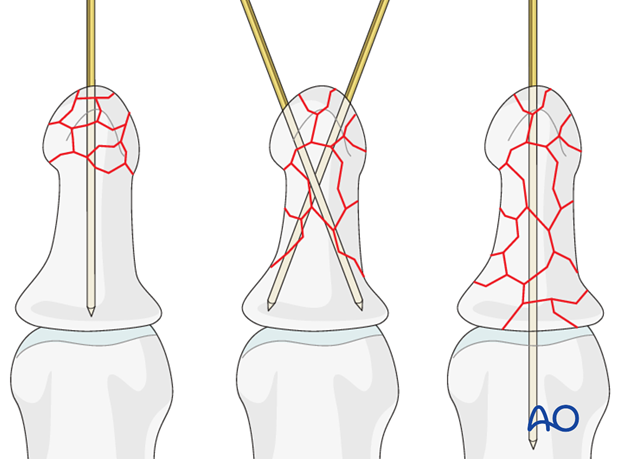
Planning for K-wires
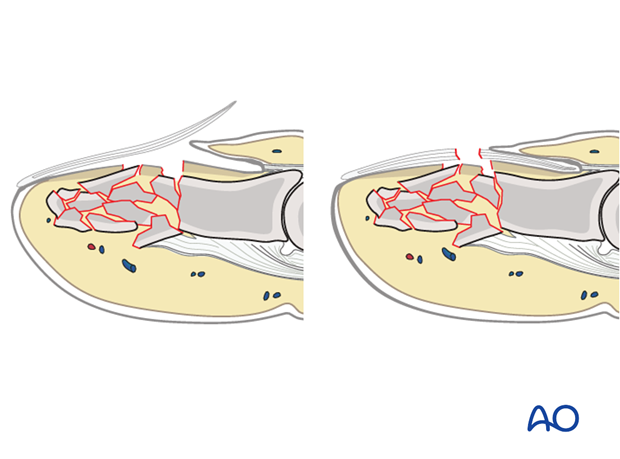
(1) Comminution only in tuft
In many of these cases, K-wire fixation is often unnecessary. In unstable fractures, a single K-wire is inserted as far as the DIP joint.
(2) Comminution extends into diaphysis
Use 2 crossed K-wires extending to the base.
(3) Comminution extends to proximal metaphysis
Use a single K-wire which passes across the DIP joint as far as the base of the middle phalanx.
Marking K-wire track
In order to avoid unnecessary radiation from image intensification, mark the planned track of the K-wire with a skin marker (or methylene blue) on the distal phalanx in both the AP and the lateral aspects.
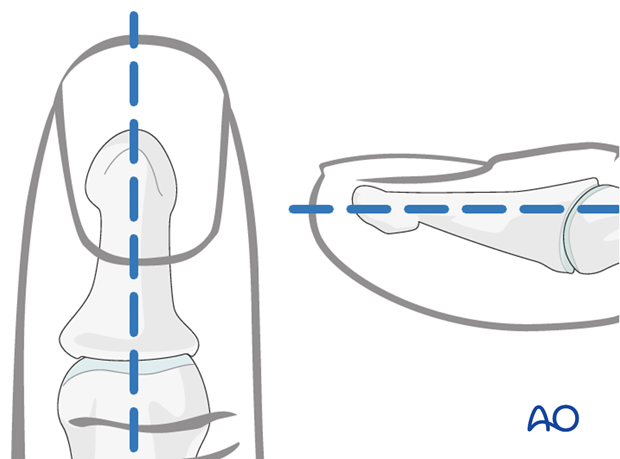
Approach
For this procedure a percutaneous approach through the finger tip is normally used.
7. Inserting the K-wire
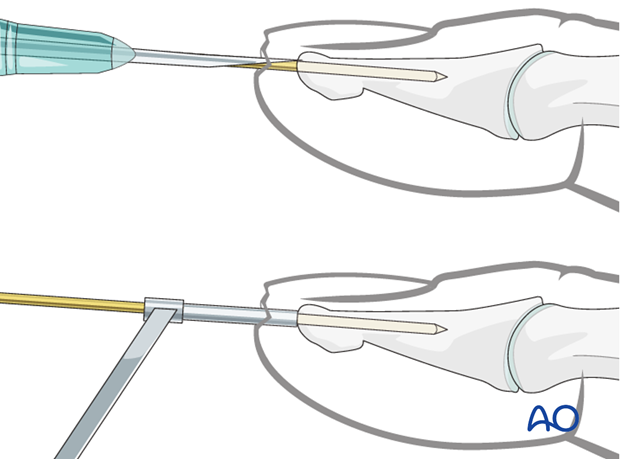
Pitfall: slipping K-wire
Due to the conical shape of the tip of the distal phalanx, there is a risk of slippage of the K-wire, either in a lateral, palmar, or dorsal direction.
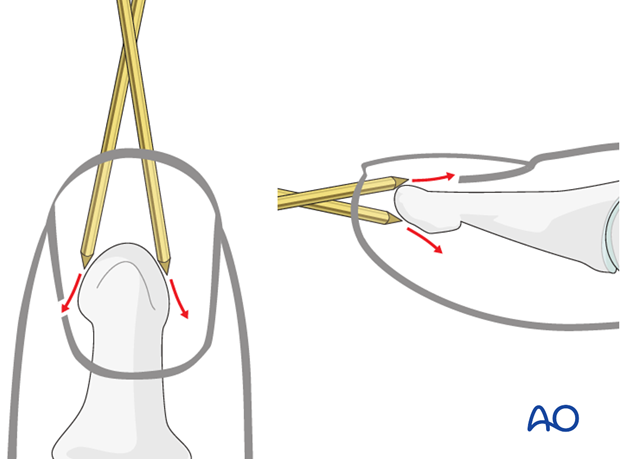
Pearl: preventing slippage
To prevent the K-wire from slipping during introduction, either a 16 gauge hypodermic needle or a 1.0 mm drill guide can be used. Either finds good purchase on the tip of the distal phalanx and will ensure that the K-wire is inserted in the center and along the longitudinal axis of the phalanx.
Pitfall: K-wire in wrong plane
If a K-wire is mistakenly inserted at an angle to the axis of the phalanx, we recommend leaving it in until a second K-wire has been inserted in the correct orientation. This will prevent the wire from going unintentionally along the wrong track.
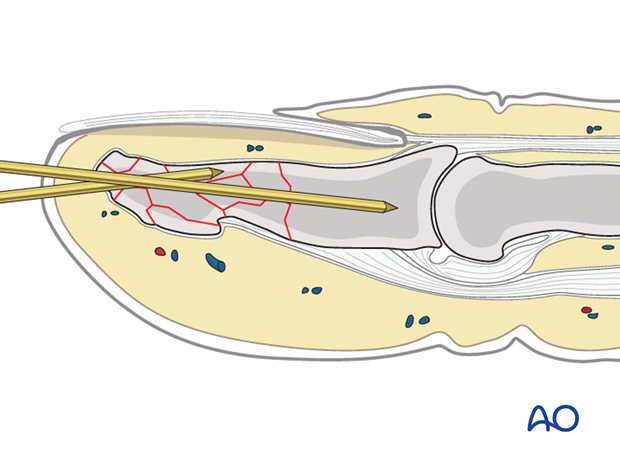
Fully insert the K-wire
The K-wire is advanced through the distal phalanx up to the DIP joint.
Proximal or comminuted fractures
In very proximal or comminuted fractures, the K-wire is advanced through the DIP joint into the middle phalanx, as far as its base, in order to achieve more stable fixation. Be careful not to penetrate the PIP joint.
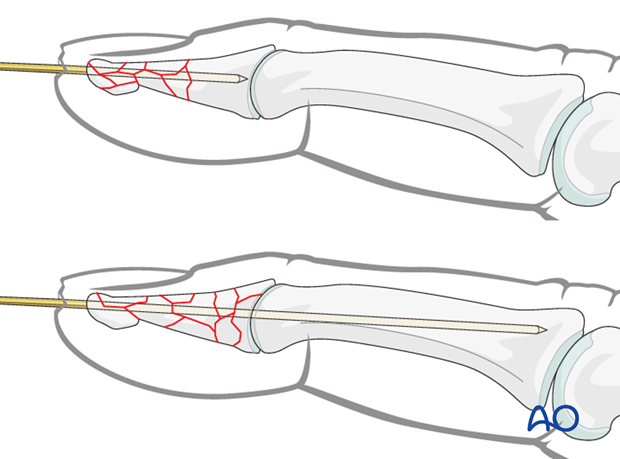
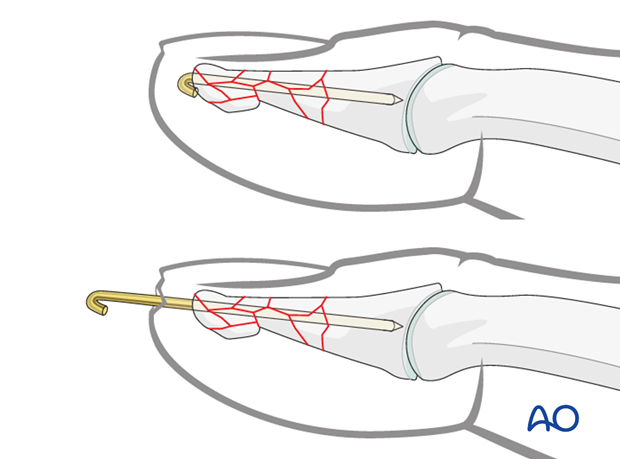
Cut the K-wire
There are two methods for completing K-wire fixation. Each method has its advantages and disadvantages.
K-wire beneath the skin
Cut the K-wire just distal of the tip of the distal phalanx. Retract it by about 5 mm (be careful not to pull the tip of the wire back through the fracture plane), bend it through 180 degrees and then bury it in the bone to avoid soft-tissue irritation.
This method has the advantage that the patient may speedily regain full use of the finger.
However, removal of the K-wire requires another minor surgical procedure under local anesthesia.
K-wire protrusion through the skin
Cut the K-wire so that it protrudes through the skin, about 1 cm from the tip of the finger. Bend its end to form a tight U-configuration to prevent catching on clothing, etc.
Leaving the K-wire to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and risk of pin-track infection.
8. Aftertreatment
Postoperatively
After K-wire fixation, the DIP joint has to be immobilized in extension, leaving the PIP joint free. Either a malleable aluminium splint, or a custom-made thermoplastic splint can be used.

While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Follow up
See the patient 5 days and 10 days after surgery.
Implant removal
If K-wire crosses the DIP joint
Radiological healing will take between 6 months and 1 year. However, after 8 weeks, the majority of the fractures are intrinsically stable. The K-wire can then be removed.
If the K-wire is in the distal phalanx only
If the distal tip of the K-wire was buried in the bone, does not protrude through the skin and is causing no problems, there is no need for its removal.
However, if the K-wire protrudes through the skin, about 6 weeks is the maximal time it can be left in place.













