Distal phalanx, distal and shaft, multifragmentary
Fractures of the distal phalanx
Fractures of the distal phalanx are the most common fractures in the hand.
Most frequently, the thumb, the middle finger, or somewhat less often, the index finger is injured.
Common complications of these injuries are:
- altered sensibility (numbness, hyperesthesia, tenderness)
- cold hypersensitivity (cold intolerance)
- restriction of DIP joint movement
- nail growth abnormalities
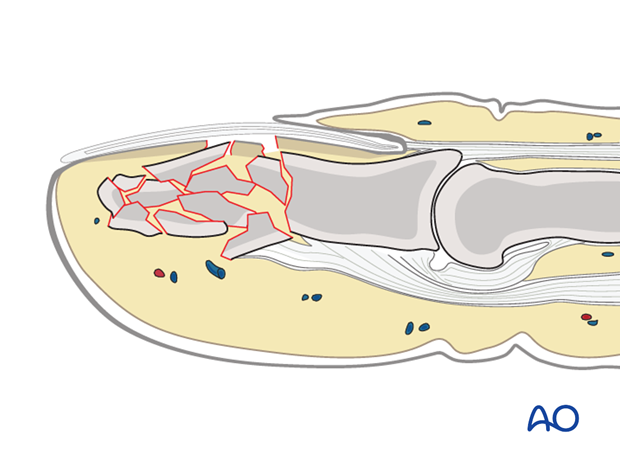
The vast majority of these fractures result from crush injuries with associated soft-tissue (nail bed, or pulp) lacerations.
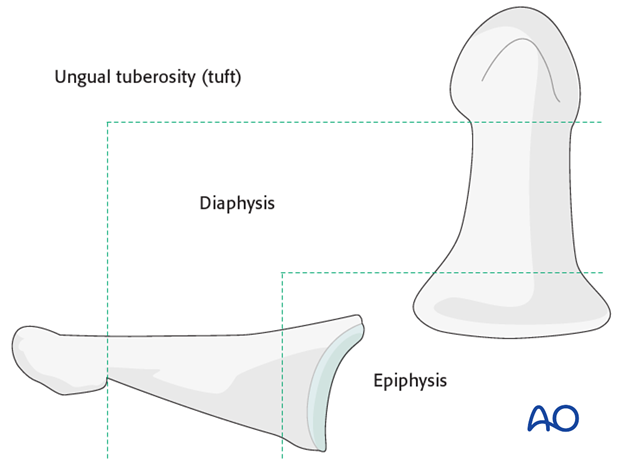
Anatomy
The distal phalanx is divided into three anatomical zones: most proximally the epiphyseal region (base), followed by the diaphysis (“waist”), and finally the ungual tuberosity (“tuft”).
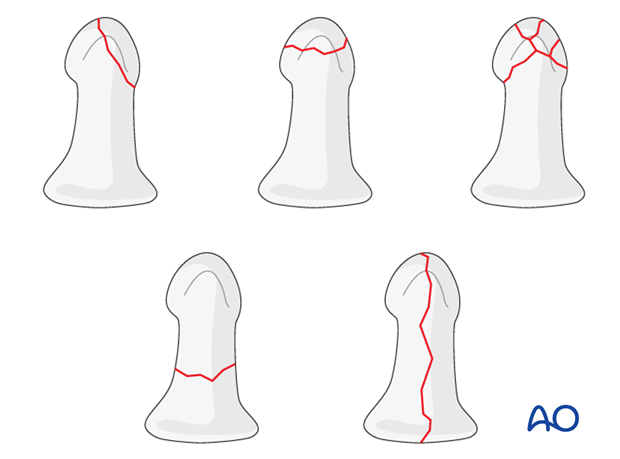
Classification of distal phalangeal fractures (after Schneider)
Schneider divides distal phalangeal fractures into tuft fractures, shaft fractures and articular fractures.
Tuft fractures include
- simple fractures
- comminuted fractures
Shaft fractures include
- transverse fractures
- longitudinal fractures (may extend to involve the DIP joint)
Articular fractures include
- palmar (flexor digitorum profundus avulsion fractures)
- dorsal (extensor avulsion, mallet fractures)
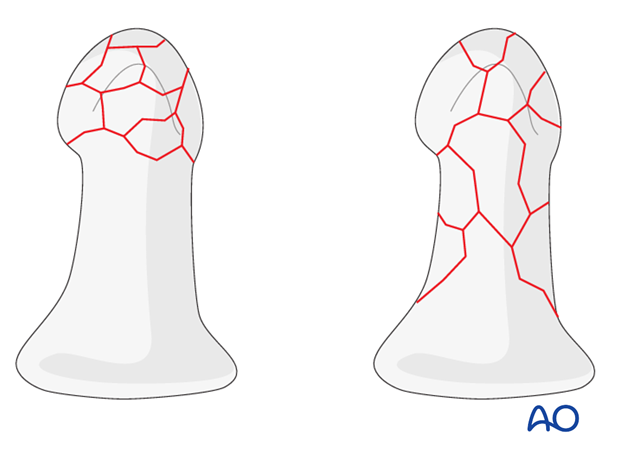
Multifragmentary fractures
In multifragmentary fractures, the comminution may be limited to the tuft, or it may extend into the diaphysis.
Treatment of crush injuries
In comminuted crush injuries, treatment of the fracture is of secondary importance. More important is soft-tissue management, i.e. of the pulp and of the nail matrix.
After repair of these structures and nail reinsertion, usually the fracture is already stable enough (with the soft-tissue repairs acting as a splint).
Bear in mind that crush injuries cause marked soft-tissue swelling and edema. Any suture repair should be a loose approximation of the edges only.
Fixation options
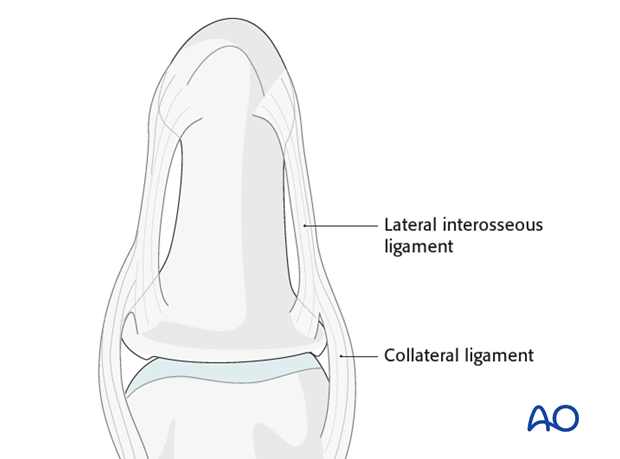
Multifragmentary fractures of the distal phalanx will often heal without complications due to the intrinsic stability provided by the soft tissues. The nail matrix, lateral interosseous ligaments and the fibrous septa are the main stabilizing structures. Therefore, simple splinting often provides adequate stability after soft-tissue repair.
Unstable, or displaced, fractures should be fixed internally with 1 or 2 K-wires, in order to prevent subsequent malunion, nonunion, or other complications such as nail deformity. A nail plate base, if avulsed, should be replaced deep to the eponychium – this helps to hold the fracture in reduction.
Diagnosis
The majority of comminuted fractures of the distal phalanx are crush injuries.
Crush injuries often have associated soft-tissue lacerations. Some of these are open fractures.
Diagnosis is based on
- clinical history of the trauma and mechanism of the injury
- clinical examination of the patient
- x-rays
AP and lateral x-rays are necessary for diagnosis. Be careful to avoid superimposition of other fingers in the x-rays.
Recognizing nail-bed injuries
Closed fractures may look harmless on x-rays, but in the majority of cases, the nail bed has been torn.
Flexor and extensor tendons displace the fracture with a typical palmar angulation of the tuft fragment.