K-wire fixation
1. Principles
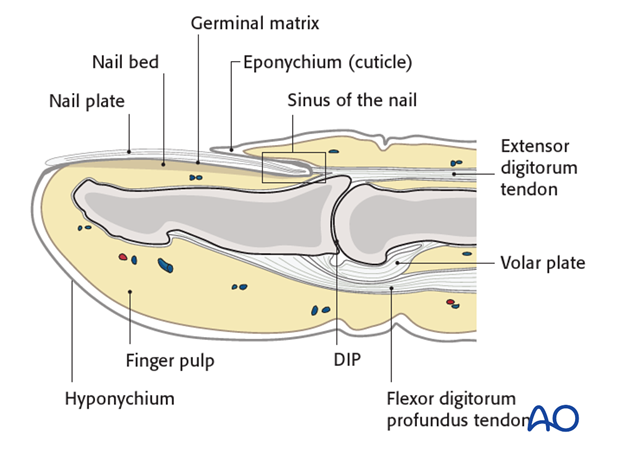
Anatomy
The distal phalanx is divided into three anatomical parts: most proximally, the metaphysis, followed by the diaphysis (“shaft”), and finally the ungual tuberosity (“tuft”).
The base of the distal phalanx has a prominent dorsal crest at the insertion of the extensor tendon. The tendon is also adherent to the distal interphalangeal (DIP) joint capsule.
On the palmar surface is the insertion of the flexor digitorum profundus tendon. This is also adherent to the volar plate.
The flexor tendon inserts into the whole width of the base of the distal phalanx.
The volar plate is very flexible, allowing hyperextension of the DIP joint and pulp-to-pulp pinch.
The vascularity of the extensor tendons is more precarious than that of the flexor tendons. This prolongs extensor tendon healing time.
Diagnosis
Discontinuities of the extensor insertion are often referred to as “mallet injury” or “baseball finger”. They can be purely tendinous, or bony avulsion fractures.
Diagnosis is based on
- the clinical history of the trauma,
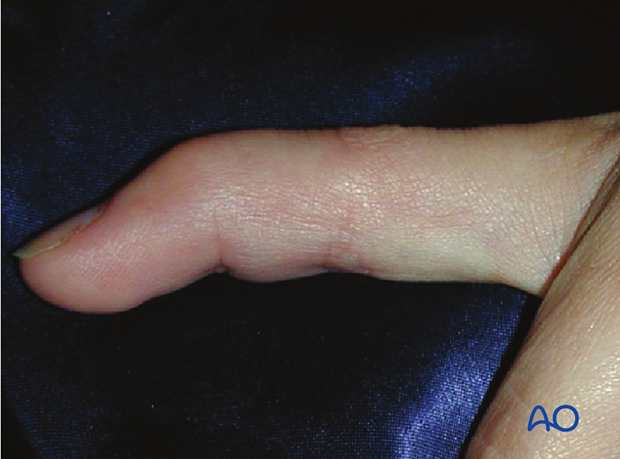
- deformity, pain and swelling located in the dorsal aspect of the DIP joint,
- inability actively and fully to extend the DIP joint,
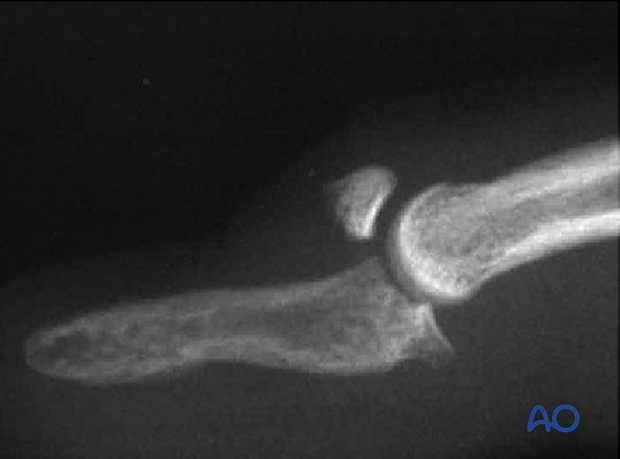
- x-rays.
AP and true lateral x-rays of the DIP joint are necessary for the diagnosis of fracture avulsions.
Low-energy radiographs, as used to visualize soft tissues, can be useful in identifying small flakes of bone.
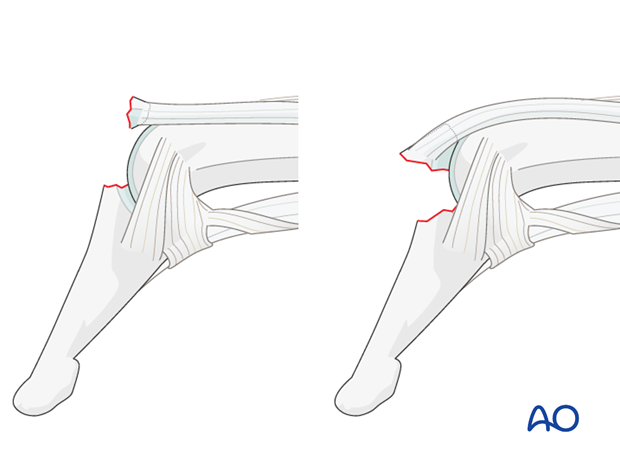
Flexion injury
The commonest cause of these injuries is forcible flexion of the actively extended DIP joint, as when stubbing a straight finger against resistance.
Axial compression injury
Occasionally, the injury is the result of an axial overload of the terminal segment of the finger, causing joint impaction and a dorsal marginal fracture, which is retracted by the pull of the extensor tendon.
Fracture subluxation of DIP joint
An obliquely orientated axial compression force sometimes results in a dorsal marginal fracture, involving approximately half the articular surface, and can disrupt the collateral ligaments.
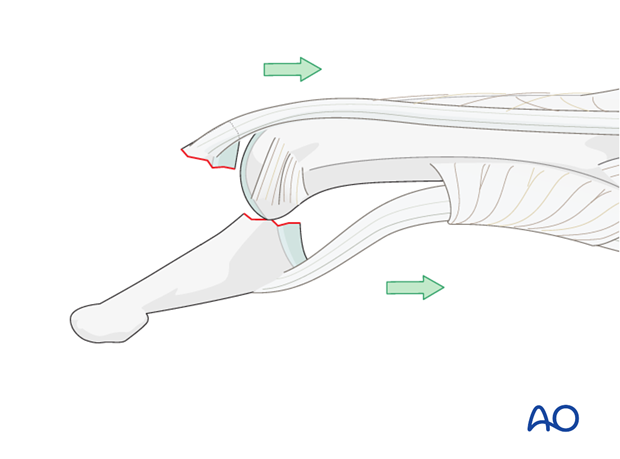
In such instances the pull of the flexor digitorum profundus results in palmar subluxation of the distal phalanx.
This injury represents a strong indication for ORIF.
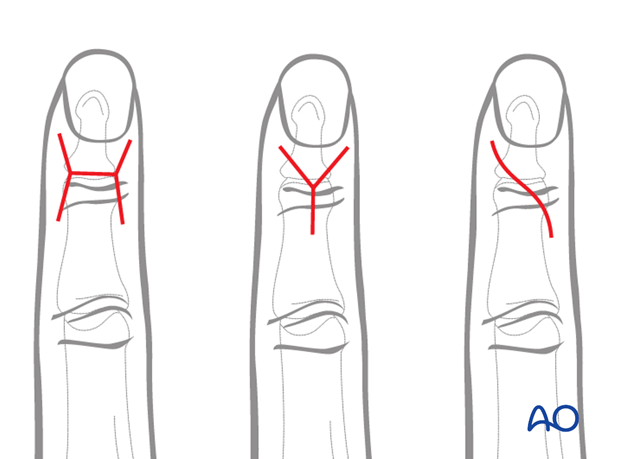
Spectrum of injury – partial disruption
These injuries may be complete disruptions or partial disruptions.
The nature of the disruption may be either a tear of the tendon insertion without fracture, or a bony avulsion of the tendon from the dorsum of the base of the distal phalanx, the bony fragment being of variable size.
In incomplete tendon injuries the resulting extension lag is no greater than 30 degrees. The patient retains a partial ability actively to extend the DIP joint.
In complete disruption of extensor mechanism, the patient is unable actively to extend the DIP joint.
The flexor digitorum profundus exerts a flexion deforming force onto the distal phalanx, partly counterbalanced by the intact oblique retinacular ligaments and the collateral ligaments.
A similar clinical picture is presented by bony avulsion of the extensor mechanism at its insertion. The dorsal avulsion fracture is of variable size.
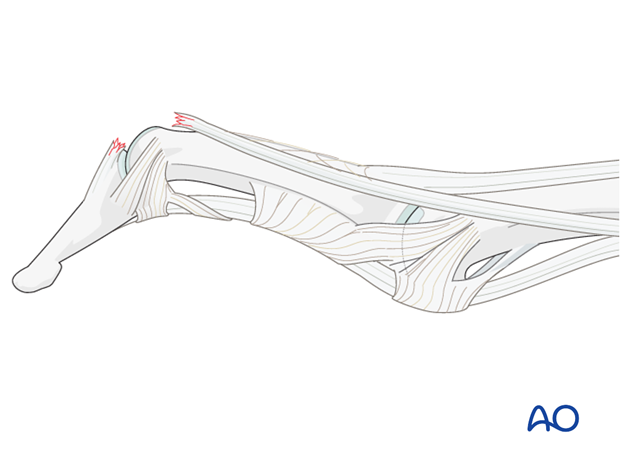
Swan-neck deformity
In some patients, elasticity of the ligaments and a lax PIP joint can result in swan-neck deformity, because after disruption of the extensor mechanism at the DIP joint, all extensor forces are concentrated on the PIP joint.
Nonoperative treatment (splinting)
Nonoperative treatment can produce excellent results, with near-normal range of motion, due to bone remodelling, even in the presence of persisting fragment displacement.
Nonoperative treatment is based on immobilization of the DIP joint in extension, leaving the PIP joint free.
Duration of immobilization
The DIP joint should be immobilized in extension for 8 weeks. It must be impressed on the patient that splintage should be uninterrupted during this period.
It must be kept in mind that the vascularity of this area is precarious, even in healthy patients, and healing is slow. Any shorter period of immobilization risks re-rupture. Joint stiffness is unusual after these injuries.
Result
Frequently, patients may complain of a dorsal prominence, and of loss of the last 10-20 degrees of extension of the DIP joint. Dorsal tenderness rarely persists for more than a month or so after removal of the splint.
Nonoperative treatment (splinting)
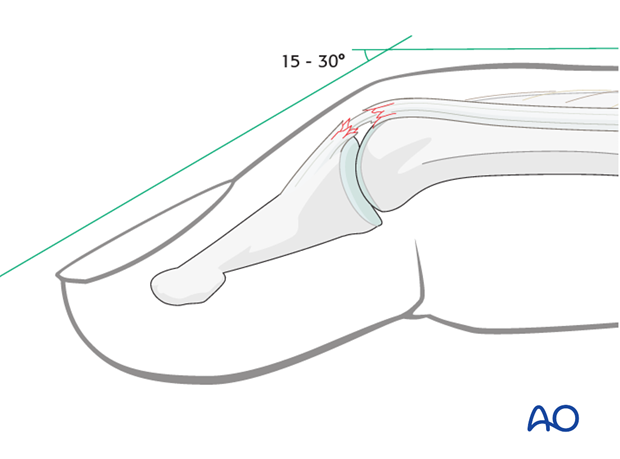
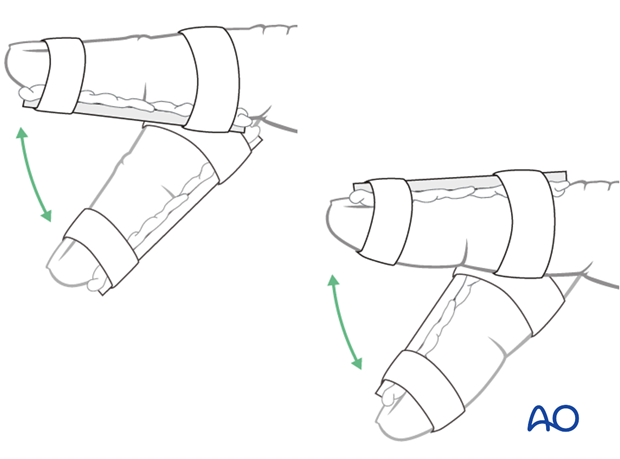
Dorsal splint vs palmar splint
Using a dorsal splint has the advantage of leaving the patient with the ability to pinch while the digit is immobilized.
However, proponents of palmar splintage argue that the palmar aspect is better cushioned than the dorsal and thereby can tolerate the splint better.

Contoured custom thermoplastic splint
The advantage of a custom thermoplastic splint is that it is better adapted to the shape of the finger, and easier to change.

Cleaning
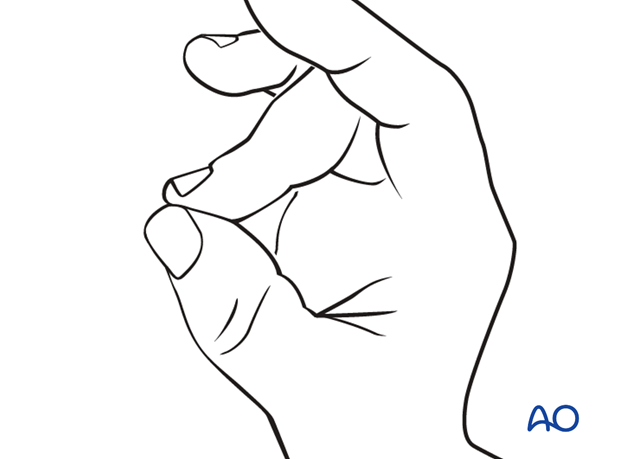
Instruct the patient to keep the finger in extension by pinching it with the thumb when the splint is taken off for cleaning.
Flexing the finger may delay the healing process.
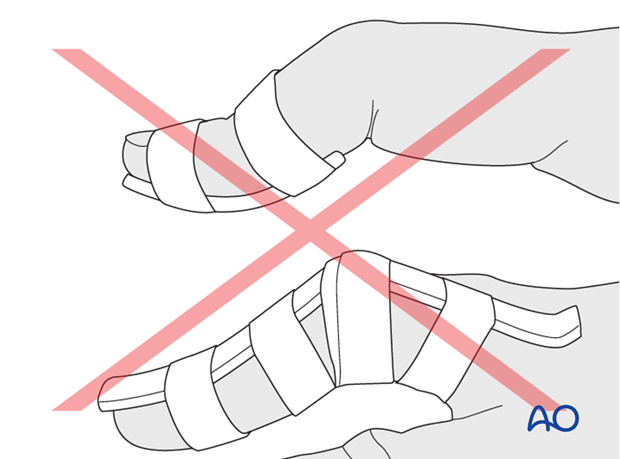
Pitfalls of nonoperative treatment
Hyperextension of the DIP joint
Do not attempt to immobilize the joint in hyperextension. This can compromise the precarious vascularization of the skin of the dorsal aspect of the joint and might provoke ischaemia and possible necrosis.
Immobilization of the PIP joint
Do not immobilize the PIP joint as this may result in flexion contraction of the joint.
2. Operative treatment: caveat
Inexperienced handling of this area may harm the germinative matrix of the nail and cause permanent deformity. Consider that nonoperative treatment is almost always a viable alternative in these fractures, often with comparable results. Operative treatment should only be attempted by experienced hand surgeons, in selected cases. Absolute indications for surgical intervention are:
- Open fractures
- Palmar subluxation of the DIP joint
It is wise always to use magnifying loupes in these surgical procedures.

3. Approach
For this procedure a dorsal approach to the DIP joint is normally used.
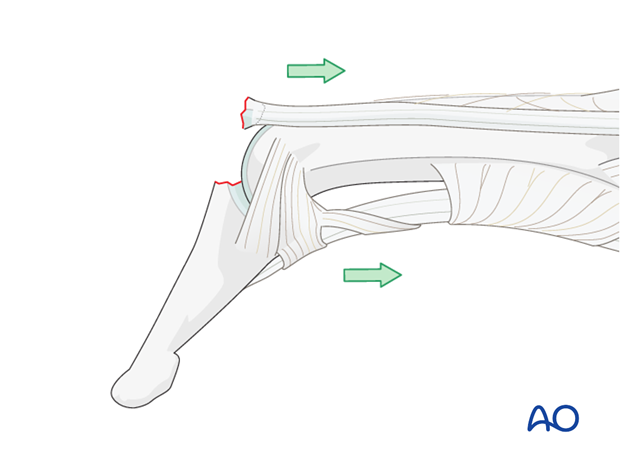
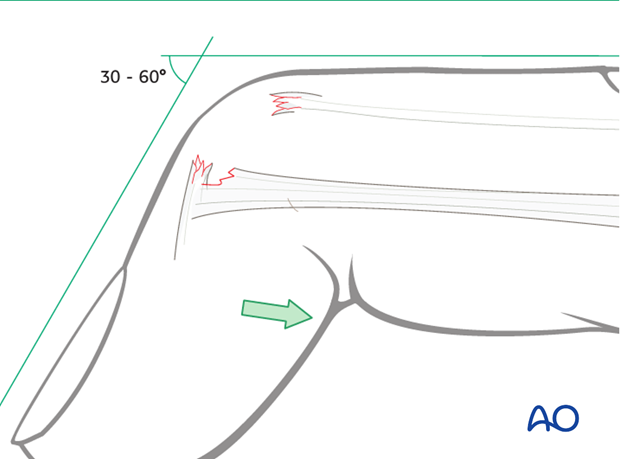
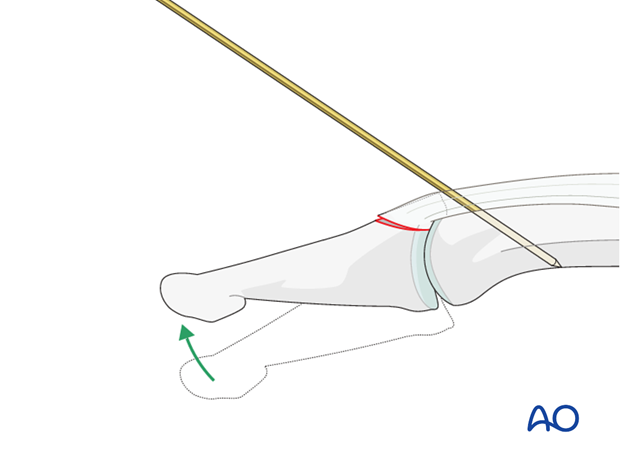
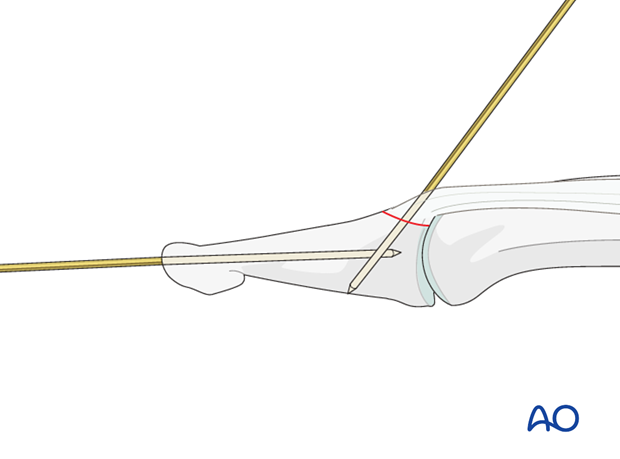
4. K-wire fixation: Extension block
Insert K-wire
Use image intensification to determine the precise location of the DIP joint. Make a small longitudinal incision over the DIP joint in order to avoid further tension of the skin against the K-wire, and subsequent irritation and possible infection. Use a drill guide or a 16 hypodermic needle to insert a 1.0 mm K-wire at an angle of approximately 45 degrees through the terminal extensor tendon into the head of the middle phalanx. Engage the far cortex.
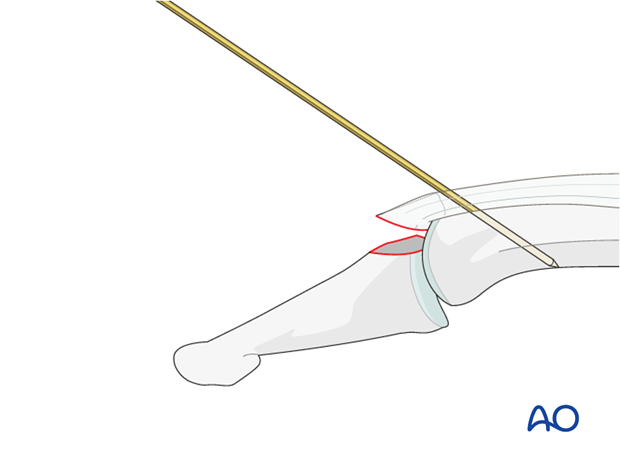
This K-wire serves as the extension block.
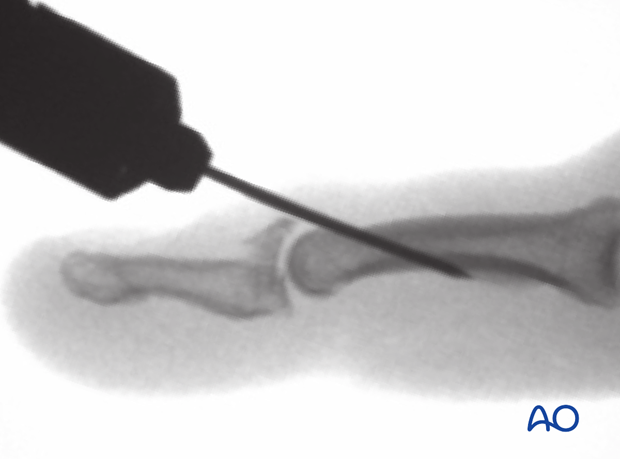
Extend the DIP joint
Carefully reduce the fracture by extending the DIP joint.
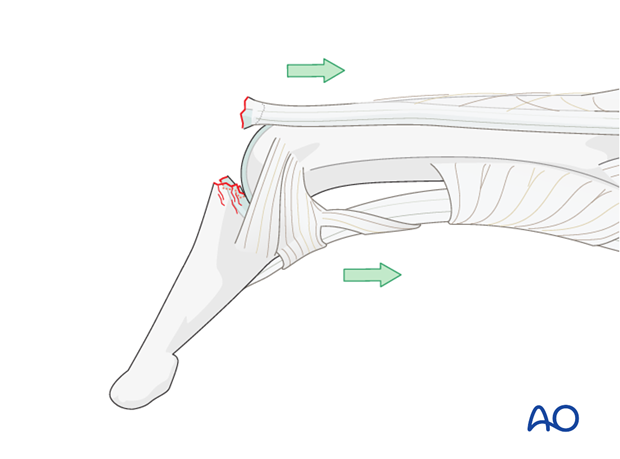
5. K-wire fracture fixation
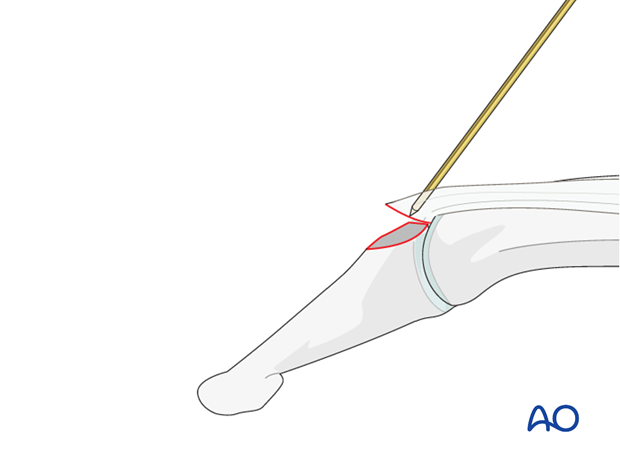
Insert fixation K-wire
Use image intensification to determine the precise location of the DIP joint and the avulsed fragment.
Make a small longitudinal incision over the DIP joint in order to avoid tension of the skin against the K-wire, subsequent irritation and possible infection.
Insert a 1.0 mm K-wire into the avulsed fragment.
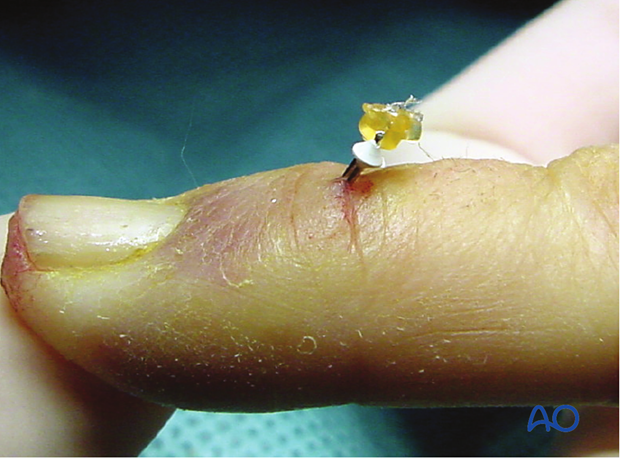
Insert axial K-wire
Using a drill guide or a hypodermic needle, insert an axial K-wire through a 1 cm horizontal incision in the finger tip, over the center of the distal phalanx and just beneath the nail.
Advance the K-wire into the base of the distal phalanx.
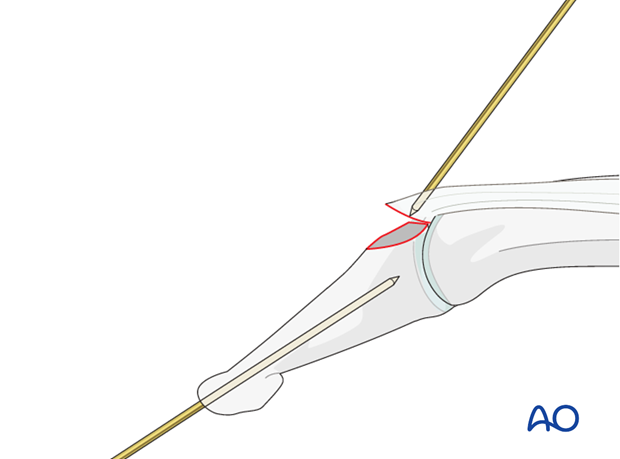
Reduce the fracture
Use the axial K-wire as a joystick to extend the DIP joint and to reduce the fracture.
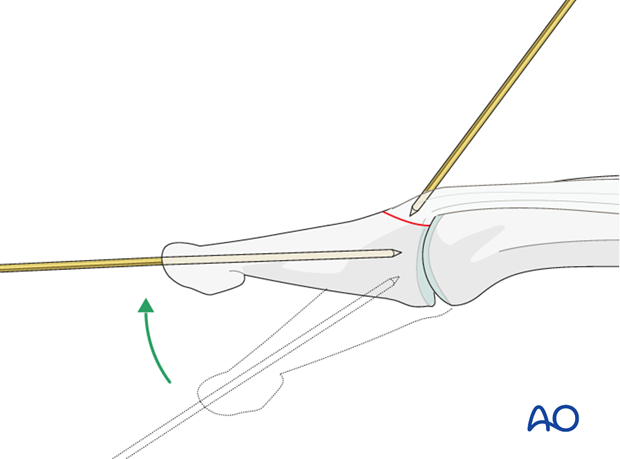
K-wire fixation
Advance the first K-wire into the main fragment, fixing the fracture. Engage the far cortex.
Then advance the axial K-wire across the DIP joint into the base of the middle phalanx.
Pearl: needle instead of K-wire
Instead of a K-wire, a 26 insulin needle can be used for fixing the fracture.
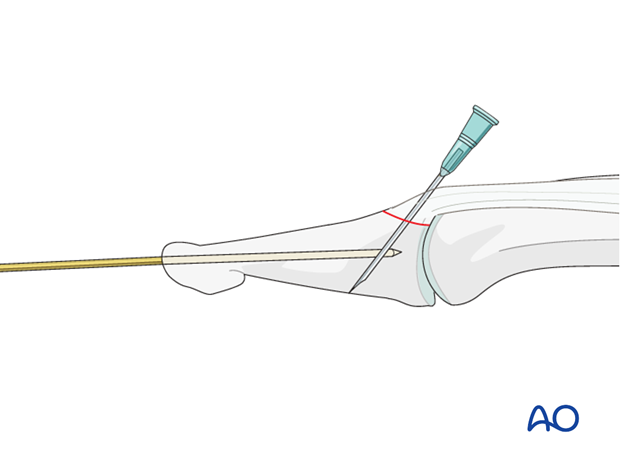
There are two advantages to this option:
- the needle is thinner than a K-wire,
- it is cheaper than a K-wire and easily available
6. Aftertreatment
Aftertreatment depends on the size of the fragment, the quality of the bone, and the stability gained by the fixation.
The DIP joint is immobilized in extension in a palmar splint, leaving the PIP joint free.
PIP joint movement is encouraged immediately to avoid extensor tendon adhesion.

Functional exercises
After 3 weeks, the splint is removed. Passive motion is only permitted after removal of the K-wires at 4 weeks.
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.
Mobilization of the PIP and MP joints are encouraged from the very beginning.














