K-wire fixation
1. Principles
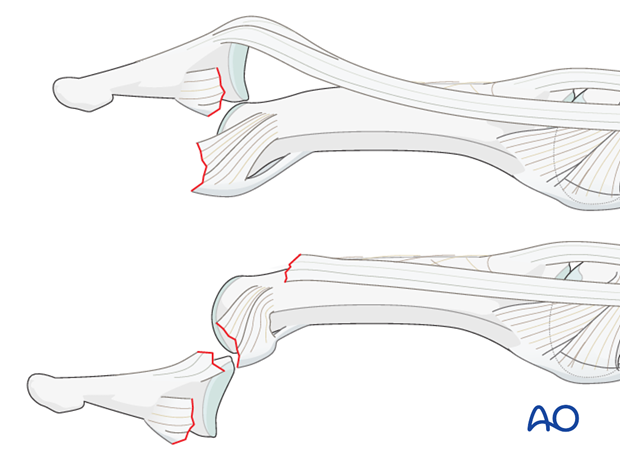
Mechanism of the injury
The majority of these uncommon injuries are caused by sporting accidents.
Typically, hyperextension of the finger causes dorsal, or, rarely, palmar dislocation.
In both cases, disruptions of the collateral ligament and the volar plate will be present.
In palmar dislocations, there will be an additional terminal extensor tendon disinsertion.
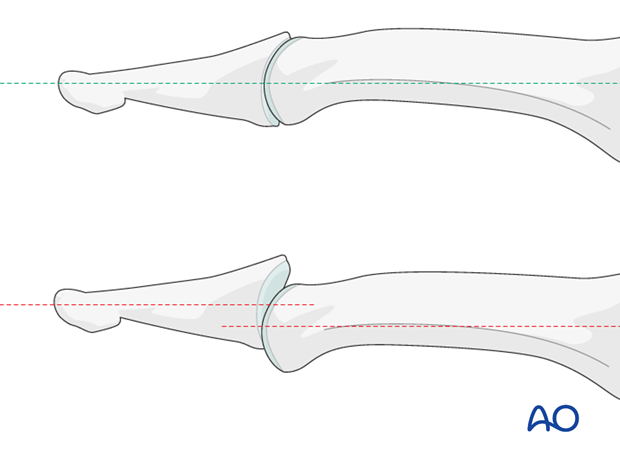
Recognizing subluxation
Diagnosis is based on
- the clinical history of the trauma and mechanism of the injury
- the clinical examination of the patient
- the x-rays
AP and lateral x-rays are necessary for diagnosis. Be careful to avoid interposition of other fingers in the x-rays.
In the lateral view, the middle and distal phalanges should be collinear. Any axial malalignment is a clear indication of subluxation.
2. Closed reduction
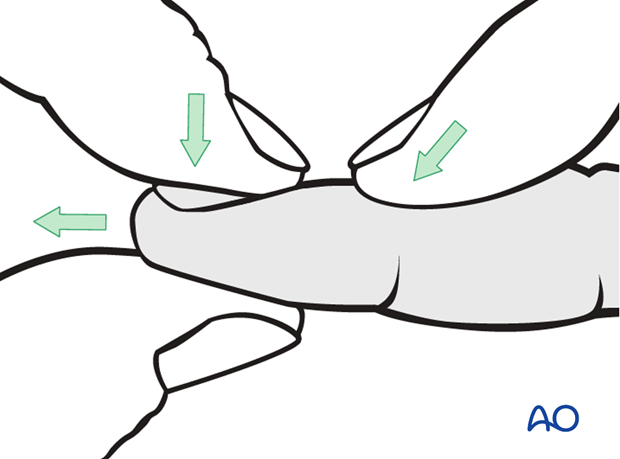
Dorsal subluxation
The majority of these dislocations can be reduced by applying traction, flexion and dorsal pressure on the base of the distal phalanx.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
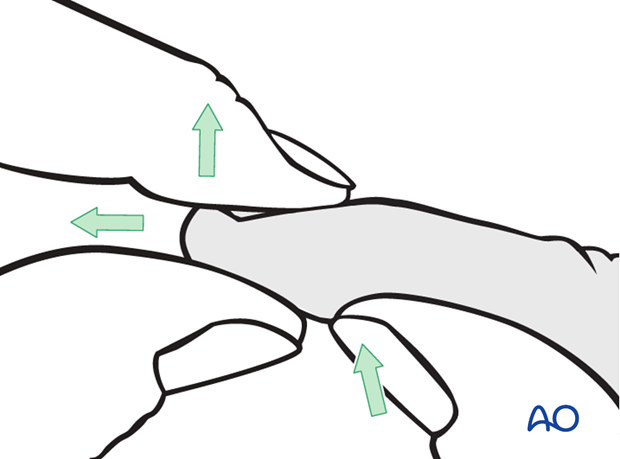
Palmar subluxation
In the case of palmar dislocation, apply traction and extension. Then apply pressure with the thumb on the palmar aspect of the base of the distal phalanx.
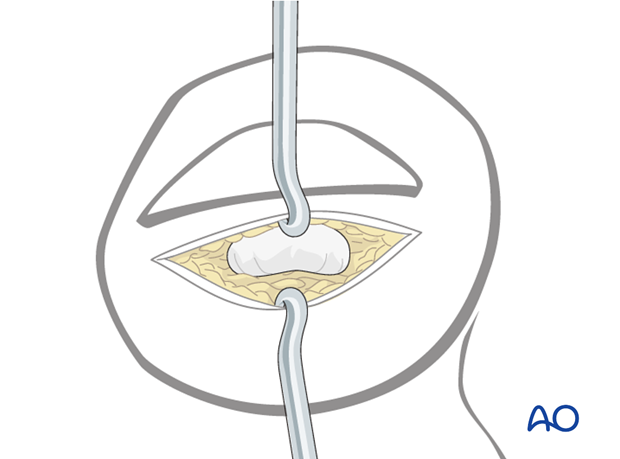
Rarely, the terminal extensor tendon, or the flexor digitorum profundus, may be interposed in the DIP joint. This is an indication for ORIF.
If the joint is stable after reduction, nonoperative treatment is usually indicated.
3. Preparation and approach
Indication
In high-demand patients, K-wire fixation enables immediate return to many activities.
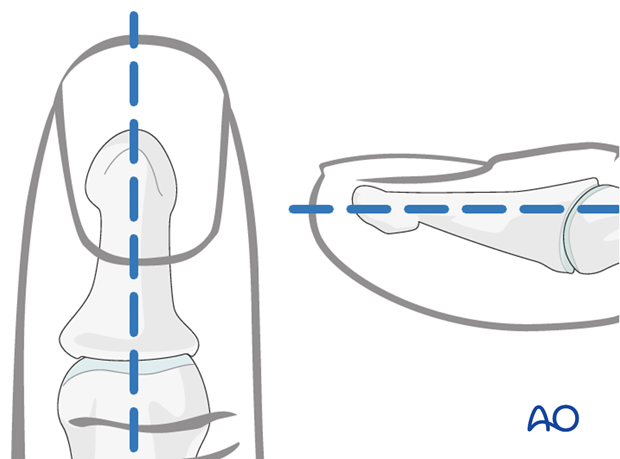
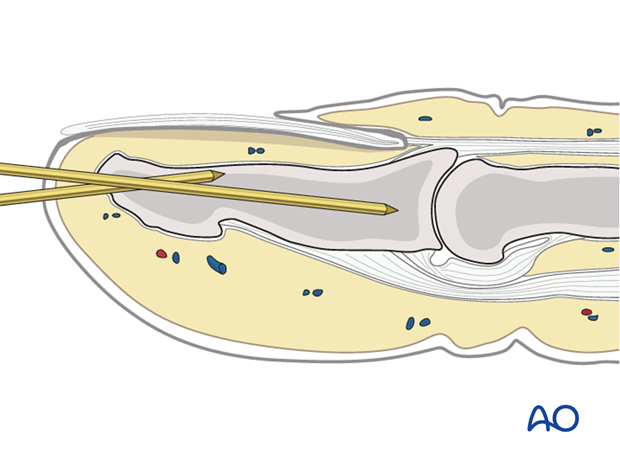
Marking K-wire track
In order to avoid unnecessary radiation from image intensification, mark the planned track of the K-wire with a skin marker (or methylene blue) on the distal phalanx, in both the AP and the lateral aspects.
Approach
For this procedure a percutaneous approach through the finger tip is normally used.
4. Inserting the K-wire
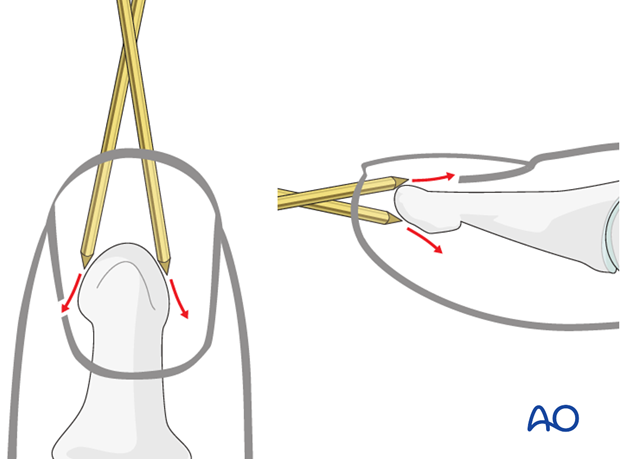
Pitfall: slipping K-wire
Due to the conical shape of the tip of the distal phalanx, there is a risk of skidding of the K-wire, either in the lateral, palmar, or dorsal directions.
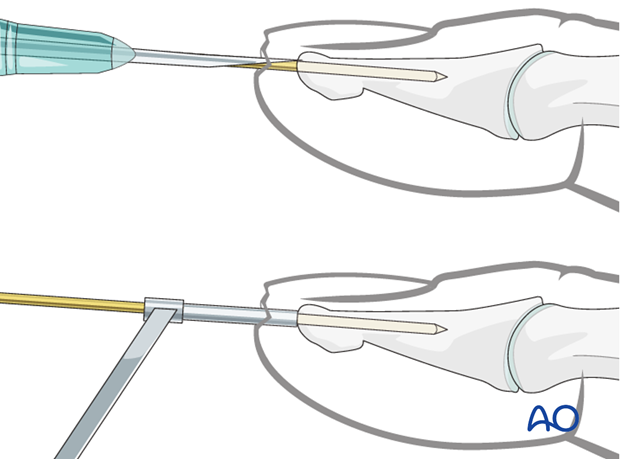
Pearl: preventing slippage
To prevent the K-wire from skidding while introducing it, either a 16 gauge hypodermic needle or a 1.0 mm drill guide can be used. Each finds good purchase on the tip of the distal phalanx and will ensure that the K-wire is inserted in the center and along the longitudinal axis of the phalanx.
Pitfall: K-wire in wrong plane
If a K-wire is mistakenly inserted at an angle to the axis of the phalanx, we recommend leaving it in until a second K-wire has been inserted in the correct orientation. This will prevent the wire from going unintentionally along the wrong track.
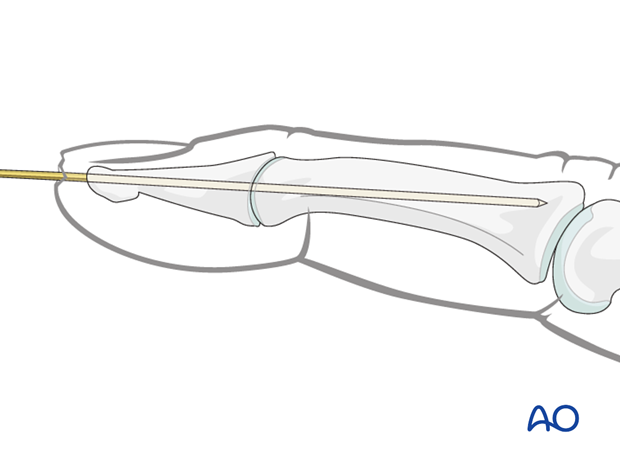
Fully insert the K-wire
The K-wire is now advanced across the DIP joint into the middle phalanx, as far as its base. Be careful not to penetrate the PIP joint.
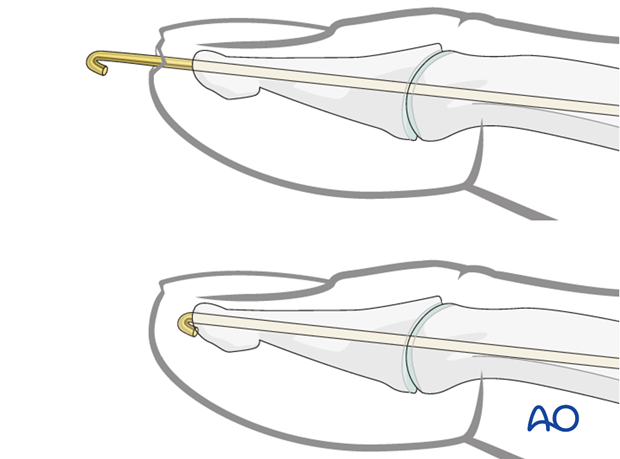
Cut the K-wire
There are two methods for completing K-wire fixation. Each method has its advantages and disadvantages.
K-wire beneath the skin
Cut the K-wire just distal of the tip of the distal phalanx. Retract it by about 5 mm (be careful not to pull the tip of the wire back through the fracture plane), bend it through 180 degrees and then bury it in the bone to avoid soft-tissue irritation.
This method has the advantage that the patient may speedily regain full use of the finger.
However, removal of the K-wire requires another minor surgical procedure under local anesthesia.
K-wire protrusion through the skin
Cut the K-wire so that it protrudes through the skin, about 1 cm from the tip of the finger. Bend its end to form a tight U-configuration to prevent catching on clothing, etc.
Leaving the K-wire to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and risk of pin-track infection.
5. Aftertreatment
Postoperatively
After K-wire fixation, the DIP joint has to be immobilized in extension, leaving the PIP joint free. Either a malleable aluminium splint, or a custom-made thermoplastic splint can be used.

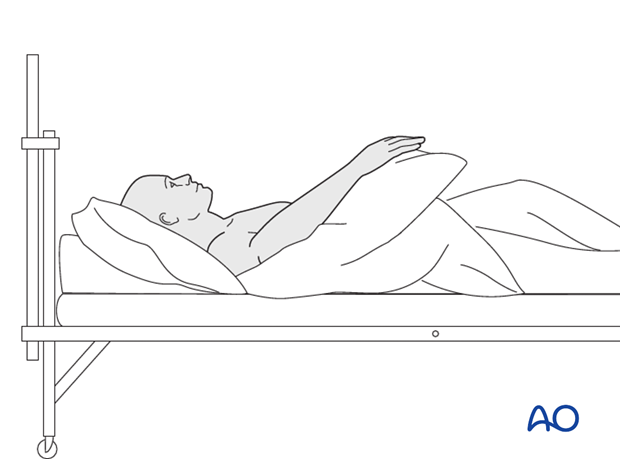
While the patient is in bed, use pillows to keep the hand elevated above the level of the heart to reduce swelling.
Mobilization
For ambulant patients, put the arm in a sling and elevate to heart level.
Instruct the patient to lift the hand regularly overhead, in order to mobilize the shoulder and elbow joints.

Follow-up
See the patient 5 days and 10 days after surgery.
Implant removal
After dorsal dislocation
After dorsal dislocation, the splint and K-wire can be removed after 3 weeks.
After palmar dislocation
After palmar dislocation, the DIP joint remains immobilized for 8-9 weeks before the splint and K-wire are removed.













