Floating shoulder - Sequence of repair
1. Introduction
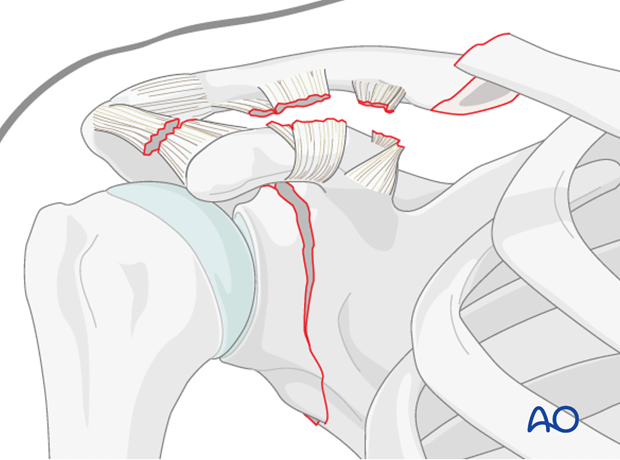
Management of floating shoulders (combined ipsilateral clavicular shaft and glenoid neck fractures) remain controversial. While some studies report reasonable function with nonoperative care, expanding indications for clavicle fracture fixation have led to an increased incidence of surgical fixation of these complex injuries.
2. Indications for surgery
Indications for surgery include standard indications for operative repair for either fracture (clavicular shaft or glenoid neck). Additionally, surgical repair can be extended to include patients who may have borderline indications of each individual fracture but who, in the surgeons opinion, would benefit from stabilization due to the multiple nature of the injuries.
3. 1: Reduction and fixation of clavicle
Introduction
In general, the clavicular shaft fracture is repaired initially, followed by reassessment of the alignment of the shoulder girdle in general and the glenoid neck fracture in particular.
Occasionally, re-establishing clavicular length and alignment may result in significant improvement in scapular and/or glenoid position such that further intervention is unnecessary. However, usually minimal change is seen and glenoid neck fixation is required.
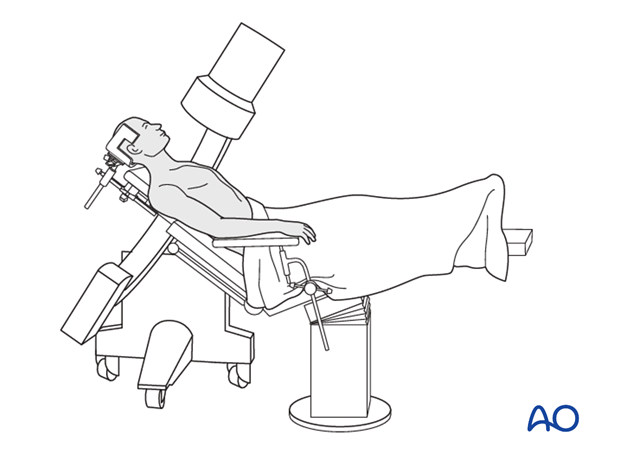
Positioning
The patient is positioned in the beach chair position.
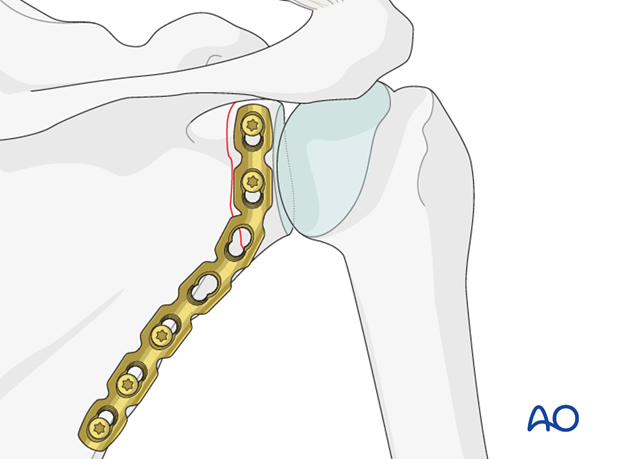
Fixation
Fixation of the clavicle proceeds as described in the clavicle module of the AO surgery reference.
Reassessment of the glenoid neck fracture
Following this, reassessment of the patient occurs with clinical examination and radiographic evaluation. If significant improvement in shoulder asymmetry and alignment of the glenoid neck fracture has occurred, then no further operative intervention is indicated.
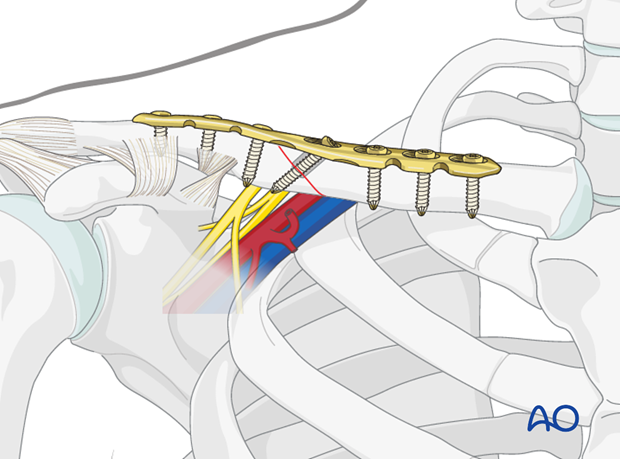
4. 2: Reduction and fixation of the glenoid neck
Introduction
If however, as is usually the case, specific indications for repair of the glenoid neck fracture remain, then the surgeon should proceed with reduction and fixation of the glenoid neck.
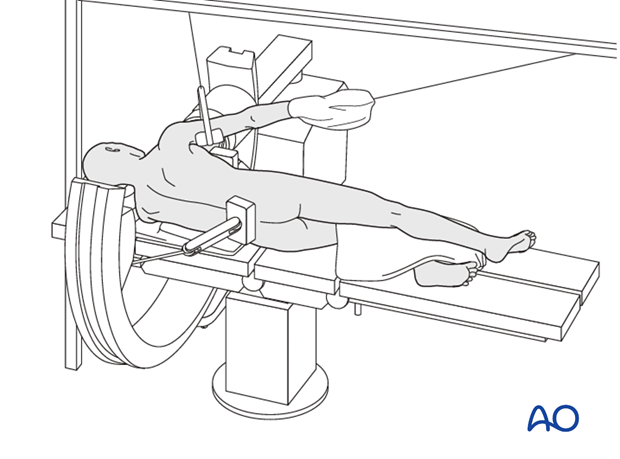
Positioning
At this point the patient is repositioned in a lateral decubitus position with the affected side up. The involved shoulder is prepared and draped as described elsewhere in this surgery reference.
Reduction and fixation
Glenoid neck fracture reduction and fixation is then performed.