MIO - Screw fixation
1. Introduction
The displaced greater tuberosity must be reduced and fixed stably. The metaphyseal fracture may be left impacted, unless severe deformity must be corrected. This disimpacts the metaphyseal fracture, which then requires fixation.
2. Principles
In some cases it is beneficial to perform a closed reduction and closed osteosynthesis. This induces no further damage to the soft-tissue and does not disturb the fracture zone including the fracture hematoma. It also does not disturb the subacromial space and allows prolonged immobilization postoperatively in a shoulder immobilizer.
The overall stability of cannulated screws alone is limited and 2-3 weeks postoperative immobilization in a shoulder immobilizer is recommended.
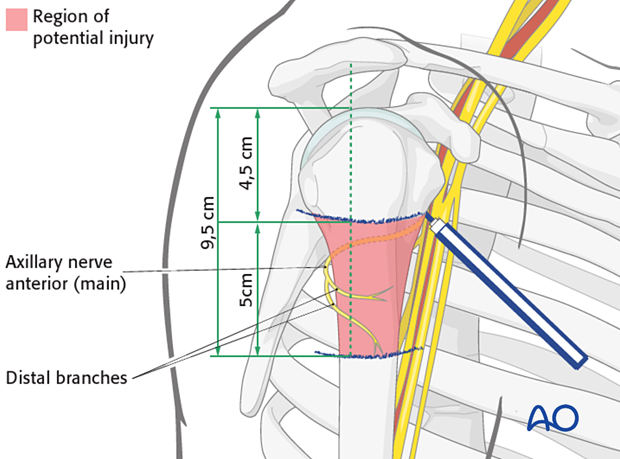
Risk of axillary nerve injury
The main structure at risk is the axillary nerve. The axillary nerve should be protected by limiting the incision to less than 5 cm distal to the acromial edge, by palpating the nerve, and by avoiding maneuvers that stretch the nerve during reduction and fixation. Remember the course of the nerve when placing K-wires.
3. Patient preparation and approach
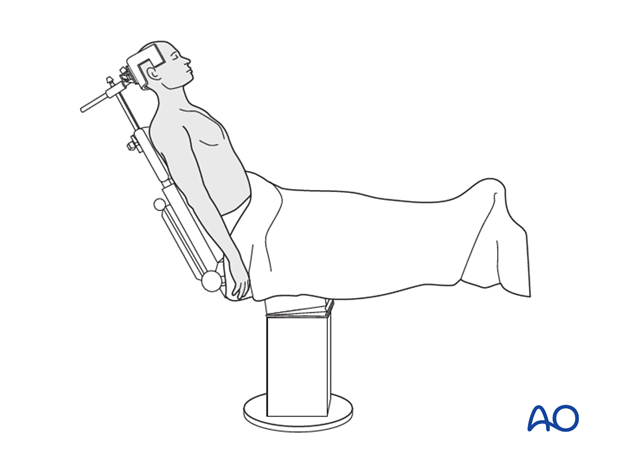
Patient preparation
This procedure is normally performed with the patient in a beach chair position.
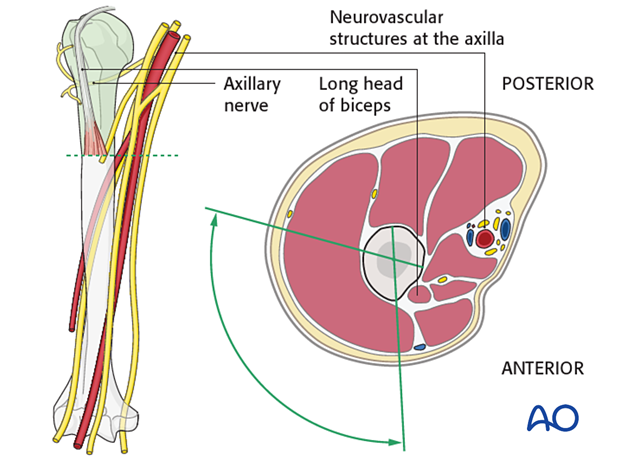
Safe zones for screw insertion
Inserting percutaneous instrumentation through the safe zones reduces the risk of damage to neurovascular structures.
4. Reduction and preliminary fixation
Reduction
Sequence of repair:
- Reduce and fix the greater tuberosity to the humeral head (thereby converting the 3-part fracture into a 2-part situation)
- Reduce the proximal humeral fragment to the shaft and fix it.
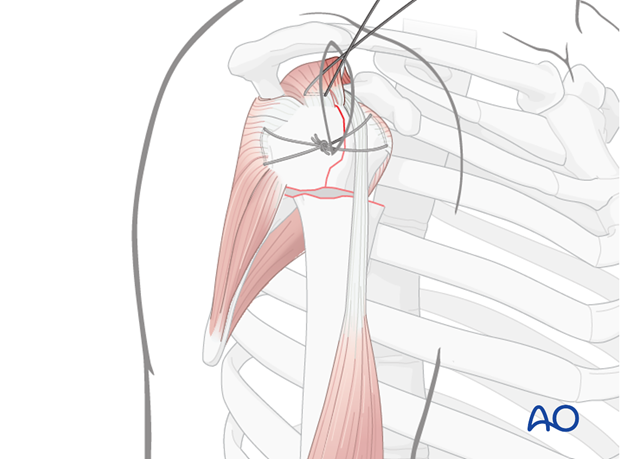
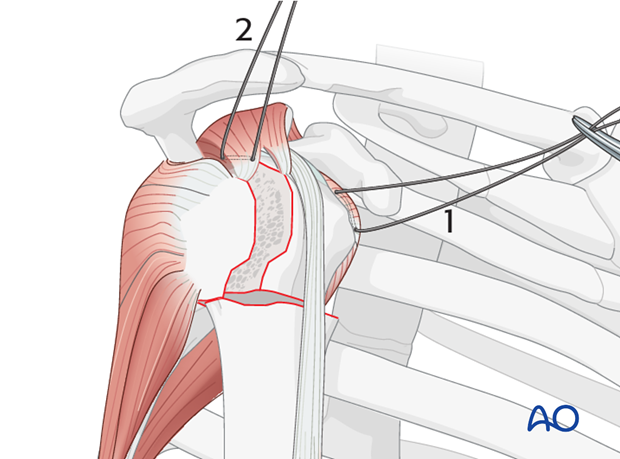
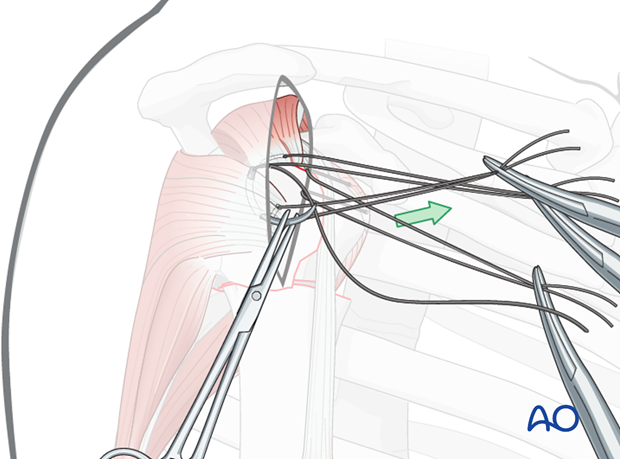
Place rotator cuff sutures
Subscapularis and supraspinatus tendon
Begin by inserting sutures into the subscapularis tendon (1) and the supraspinatus tendon (2). Place these sutures just superficial to the tendon’s bony insertions. These provide anchors for reduction, and temporary fixation of the greater and lesser tuberosities.
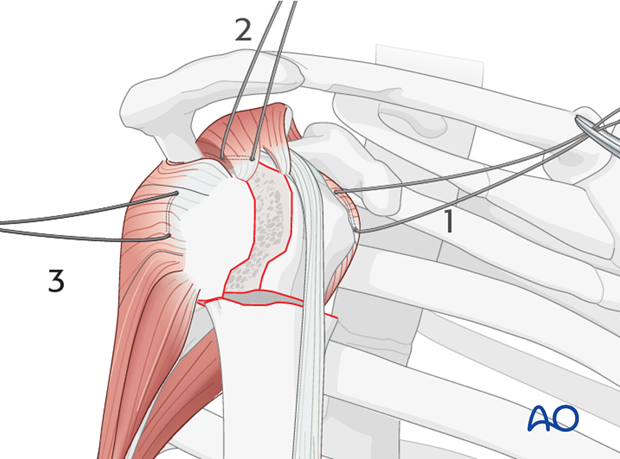
Infraspinatus tendon
Next, place a suture into the infraspinatus tendon insertion (3). This can be demanding, and may be easier with traction on the previously placed sutures, with properly placed retractors, and/or repositioning the arm.
Use of stay sutures
Anterior traction on the supraspinatus tendon helps expose the greater tuberosity and infraspinatus tendon.
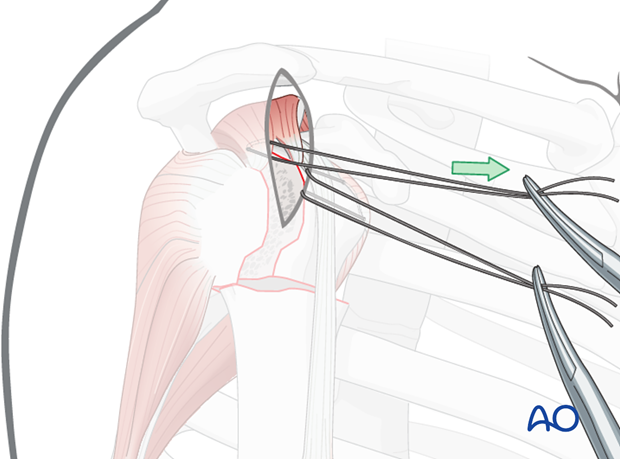
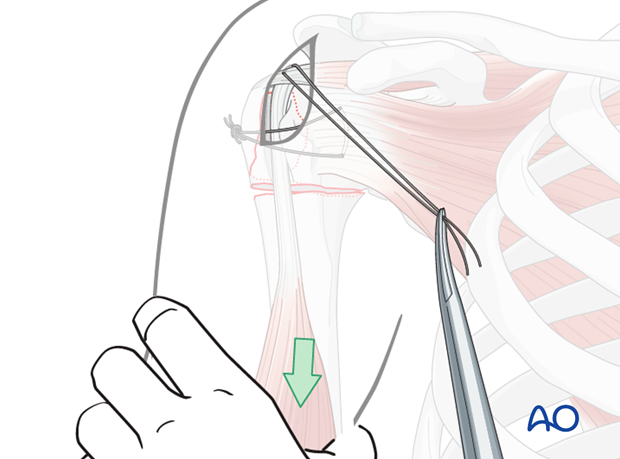
Insert a preliminary traction suture into the visible part of the posterior rotator cuff …
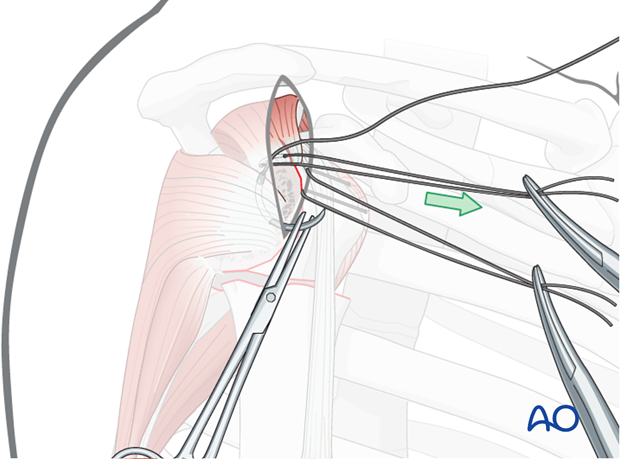
… and pull it anteriorly. This will expose the proper location for a suture in the infraspinatus tendon insertion. Then the initial traction suture is removed.
Pearl: larger needles
A stout sharp needle facilitates placing a suture through the tendon insertion.
Reduction of the greater tuberosity
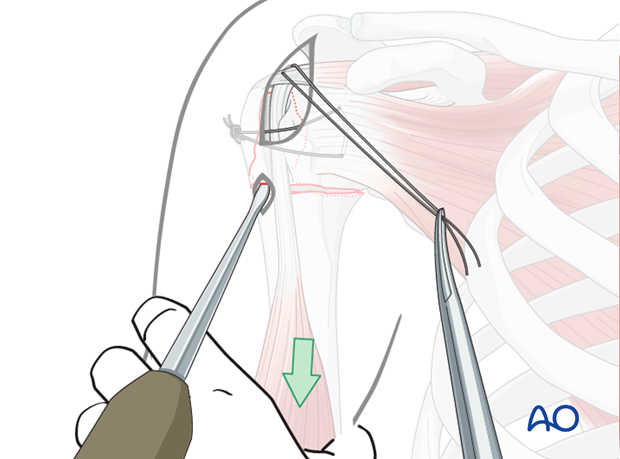
Direct reduction of the greater tuberosity fragment is performed by pulling the sutures or, …
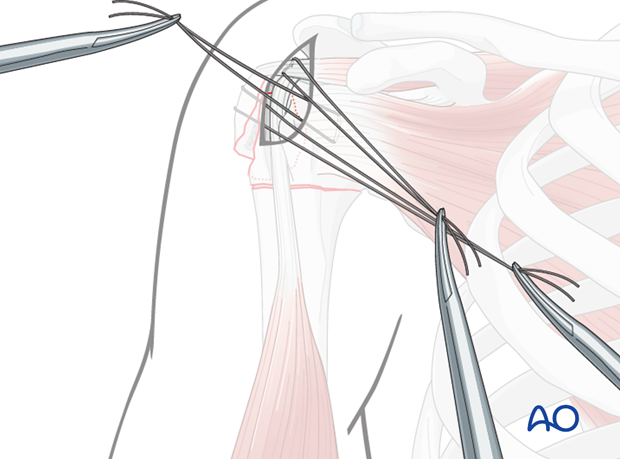
… with instruments (eg, elevator) applied either through the incision (as illustrated) or through a separate stab incision.
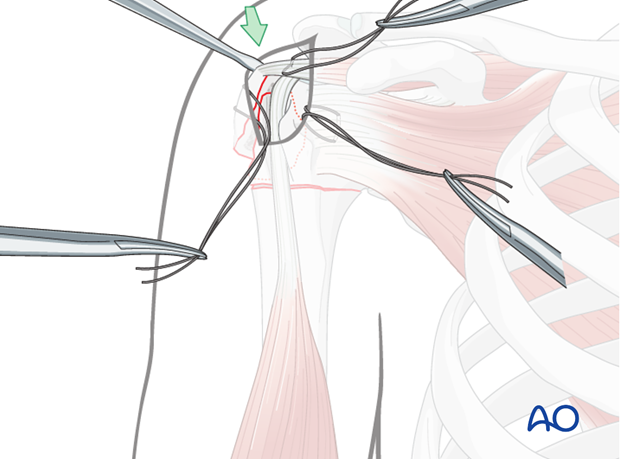
Preliminary fix the greater tuberosity
Tighten and tie the transverse sutures in order to preliminarily fix the greater tuberosity fragment. Thereby, the 3-part fracture is converted into a 2-part situation.
Reduction of the head fragment
Distal traction, perhaps augmented with increased angulation, will help to reduce the fracture.
Use of an elevator
Sometimes, the incision allows insertion of an elevator to disimpact the humeral head, or to help to correct inclination/torsion and to restore a normal relationship of the medial fracture surface. The proximal fragment should be reduced anatomically to the shaft.
The actual process of reduction is done with image intensifier control.
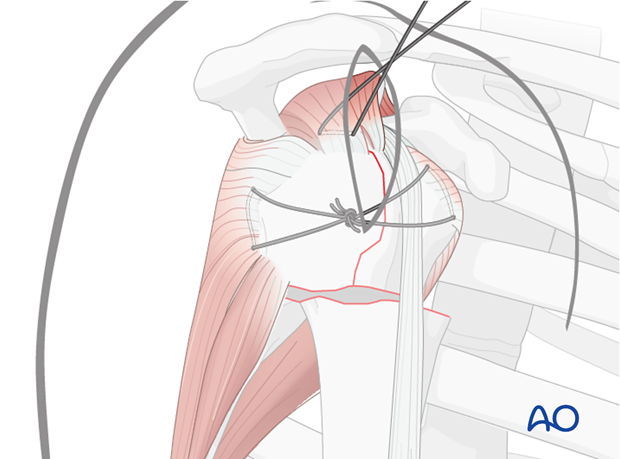
Preliminary fixation
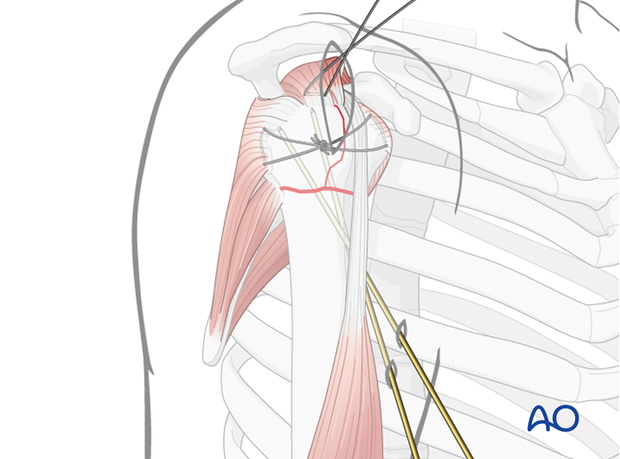
After the tuberosity and humeral head have been reduced and stabilized with sutures, there may be no need for additional preliminary fixation, but it might be advantageous to use additional K-wires to secure the position of the humeral head relative to the humeral shaft. This is illustrated with 2 retrograde K-wires. Other options are possible.
If the greater tuberosity is multifragmentary it might become necessary to use additional small K-wires in order to fix separate fragments.
Confirmation of reduction
The correct reduction must be confirmed in both AP and lateral views using image intensifier control.
5. Definitive fixation
Fixation of the head fragment
Two or more percutaneously inserted screws linking the shaft fragment to the head fragment are inserted first.
Cannulated 3.5 mm lag screws (as illustrated), or non-cannulated small fragment lag screws are used according to the surgeon’s preference.
This illustration shows two screws inserted over guide wires.
Note: Washers may be advisable in poor bone stock. Generally, they are not preferable as they make the screw heads more prominent and may result in shoulder impingement.
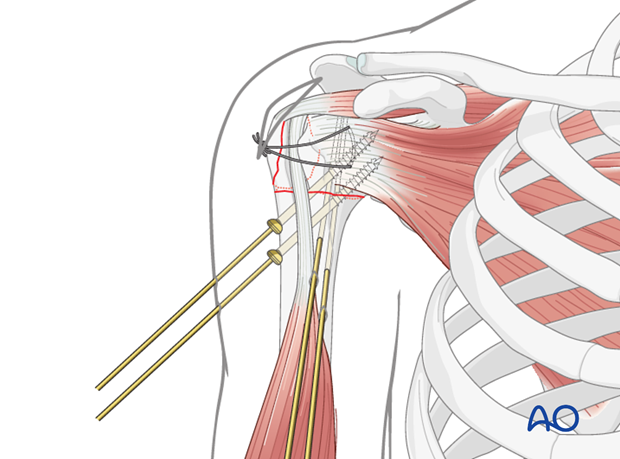
Fixation of the greater tuberosity
Remove K-wires and guides wires from the shaft.
Fixation of the head fragment is followed by insertion of a screw into the greater tuberosity.
Again, in this case, the screw is inserted over a guide wire.
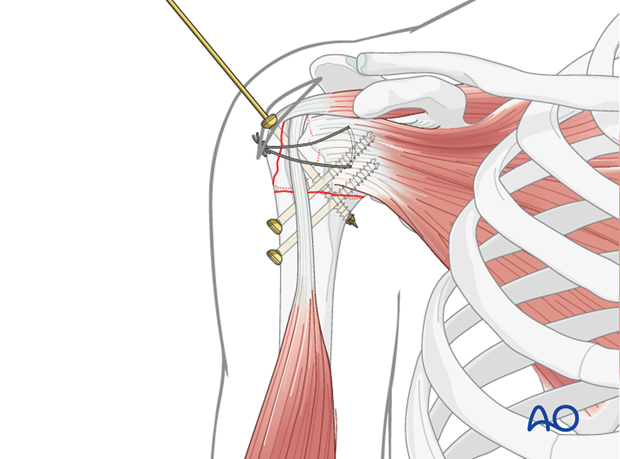
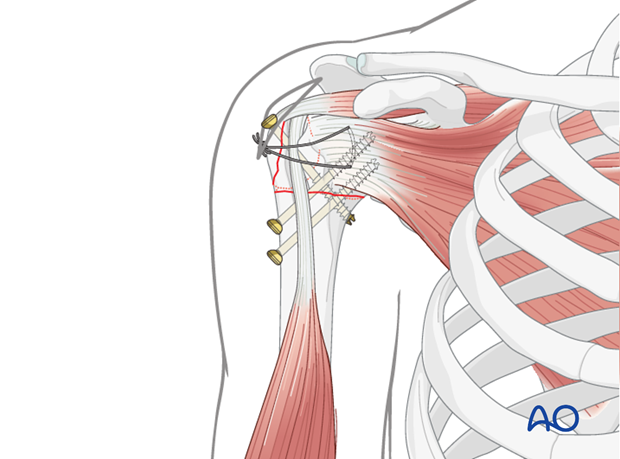
Completed osteosynthesis
The illustration shows the completed osteosynthesis.
6. Final check of osteosynthesis
Using image intensification, carefully check for correct reduction and fixation (including proper implant position and length) at various arm positions. Ensure that screw tips are not intraarticular.
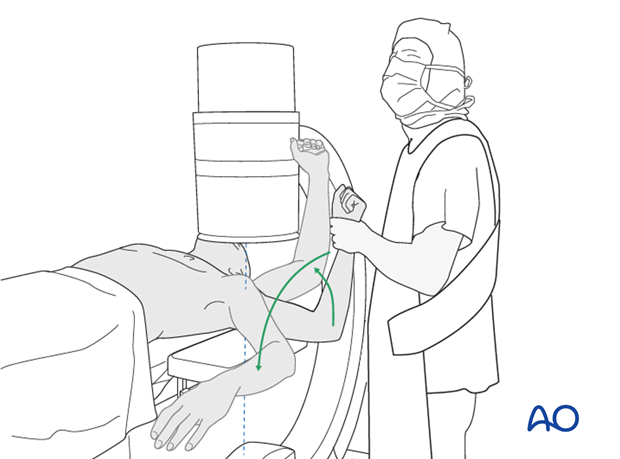
Also obtain an axial view.
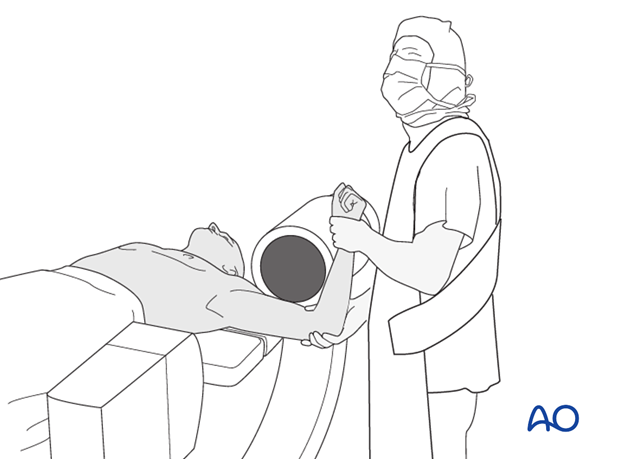
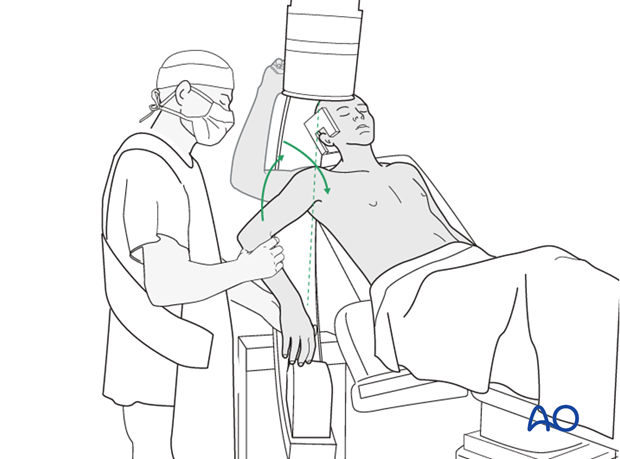
In the beach chair position, the C-arm must be directed appropriately for orthogonal views. Position arm as necessary to confirm that reduction is satisfactory, fixation is stable, and no screw is in the joint.
7. Overview of rehabilitation
The shoulder is perhaps the most challenging joint to rehabilitate both postoperatively and after conservative treatment. Early passive motion according to pain tolerance can usually be started after the first postoperative day - even following major reconstruction or prosthetic replacement. The program of rehabilitation has to be adjusted to the ability and expectations of the patient and the quality and stability of the repair. Poor purchase of screws in osteoporotic bone, concern about soft-tissue healing (eg tendons or ligaments) or other special conditions (eg percutaneous cannulated screw fixation without tension-absorbing sutures) may enforce delay in beginning passive motion, often performed by a physiotherapist.
The full exercise program progresses to protected active and then self-assisted exercises. The stretching and strengthening phases follow. The ultimate goal is to regain strength and full function.
Postoperative physiotherapy must be carefully supervised. Some surgeons choose to manage their patient’s rehabilitation without a separate therapist, but still recognize the importance of carefully instructing and monitoring their patient’s recovery.
Activities of daily living can generally be resumed while avoiding certain stresses on the shoulder. Mild pain and some restriction of movement should not interfere with this. The more severe the initial displacement of a fracture, and the older the patient, the greater will be the likelihood of some residual loss of motion.
Progress of physiotherapy and callus formation should be monitored regularly. If weakness is greater than expected or fails to improve, the possibility of a nerve injury or a rotator cuff tear must be considered.
With regard to loss of motion, closed manipulation of the joint under anesthesia, may be indicated, once healing is sufficiently advanced. However, the danger of fixation loosening, or of a new fracture, especially in elderly patients, should be kept in mind. Arthroscopic lysis of adhesions or even open release and manipulation may be considered under certain circumstances, especially in younger individuals.
Progressive exercises
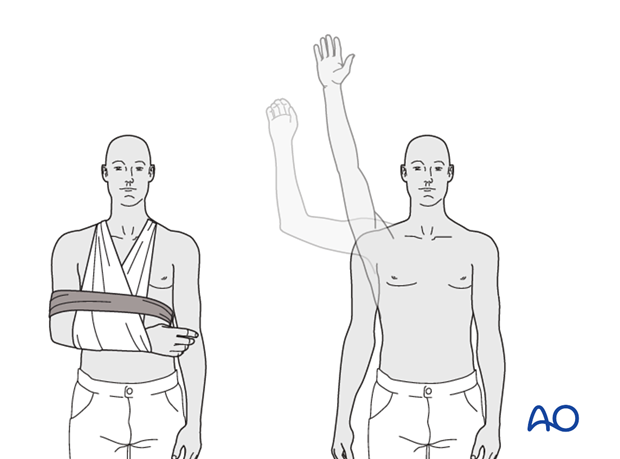
Mechanical support should be provided until the patient is sufficiently comfortable to begin shoulder use, and/or the fracture is sufficiently consolidated that displacement is unlikely.
Once these goals have been achieved, rehabilitative exercises can begin to restore range of motion, strength, and function.
The three phases of nonoperative treatment are thus:
- Immobilization
- Passive/assisted range of motion
- Progressive resistance exercises
Immobilization should be maintained as short as possible and as long as necessary. Usually, immobilization is recommended for 2-3 weeks, followed by gentle range of motion exercises. Resistance exercises can generally be started at 6 weeks. Isometric exercises may begin earlier, depending upon the injury and its repair. If greater or lesser tuberosity fractures have been repaired, it is important not to stress the rotator cuff muscles until the tendon insertions are securely healed.
Special considerations
Glenohumeral dislocation: Use of a sling or sling-and-swath device, at least intermittently, is more comfortable for patients who have had an associated glenohumeral dislocation. Particularly during sleep, this may help avoid a redislocation.
Weight bearing: Neither weight bearing nor heavy lifting are recommended for the injured limb until healing is secure.
Implant removal: Implant removal is generally not necessary unless loosening or impingement occurs. Implant removal can be combined with a shoulder arthrolysis, if necessary.
Shoulder rehabilitation protocol
Generally, shoulder rehabilitation protocols can be divided into three phases. Gentle range of motion can often begin early without stressing fixation or soft-tissue repair. Gentle assisted motion can frequently begin within a few weeks, the exact time and restriction depends on the injury and the patient. Resistance exercises to build strength and endurance should be delayed until bone and soft-tissue healing is secure. The schedule may need to be adjusted for each patient.
Phase 1 (approximately first 3 weeks)
- Immobilization and/or support for 2-3 weeks
- Pendulum exercises
- Gently assisted motion
- Avoid external rotation for first 6 weeks
Phase 2 (approximately weeks 3-9)
If there is clinical evidence of healing and fragments move as a unit, and no displacement is visible on the x-ray, then:
- Active-assisted forward flexion and abduction
- Gentle functional use week 3-6 (no abduction against resistance)
- Gradually reduce assistance during motion from week 6 on
Phase 3 (approximately after week 9)
- Add isotonic, concentric, and eccentric strengthening exercises
- If there is bone healing but joint stiffness, then add passive stretching by physiotherapist













