Lag screw and protection plate
1. General considerations
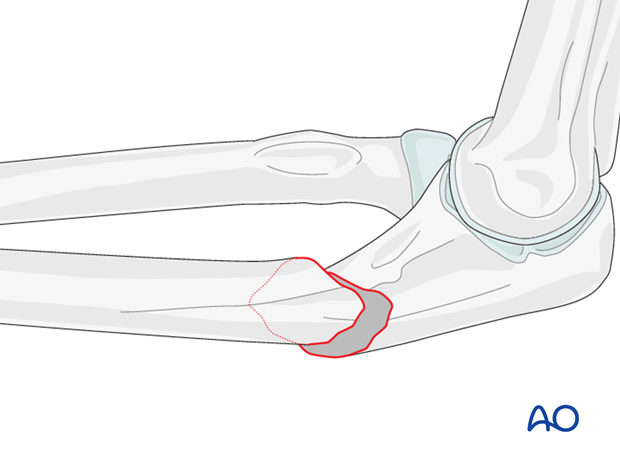
Compression with lag screw and protection (neutralization) plate
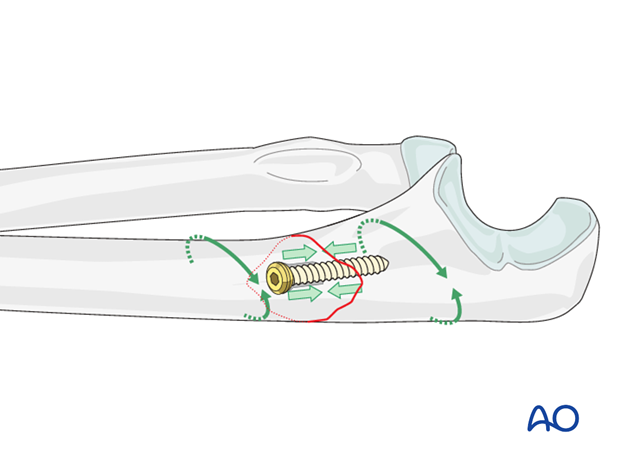
In an oblique fracture, interfragmentary compression is achieved with a lag screw.
The screw thread pulls the opposite bone fragment towards the head of the screw, compressing the fracture. On the near cortex, the thread of the screw turns freely, without purchase. Lag screws should be inserted as perpendicularly as possible to the fracture plane, to produce compression without displacement of the fracture.
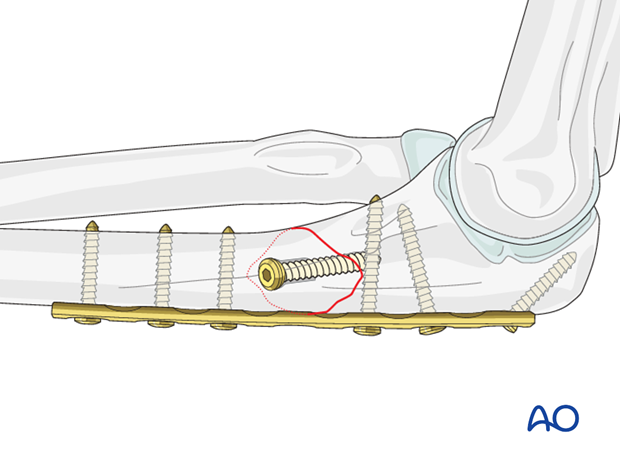
Lag screw osteosynthesis alone is not able to resist functional loading. Therefore, a neutralization plate must be added to allow early mobilization.
Note: Whenever possible (considering soft-tissue condition, fracture configuration, associated radial head fracture etc), position the plate so a lag screw can be inserted through it. This offers improved stability.
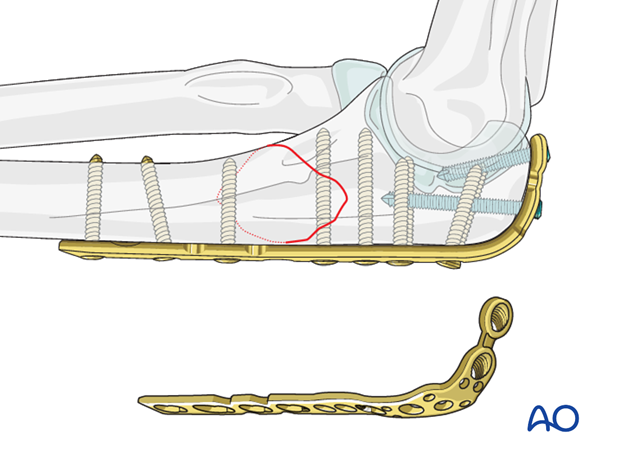
Choosing the right plate
Use a six or seven-hole plate, depending on the fracture configuration. Usually, three screws in each fragment provide sufficient stability.
These plates plate may be used:
- Small fragment dynamic compression plate (3.5 DCP),
- Limited contact dynamic compression plate (LC-DCP)
- Specific proximal ulna prebent plate
- Locking plate (LCP) may be used in osteoporotic bone.
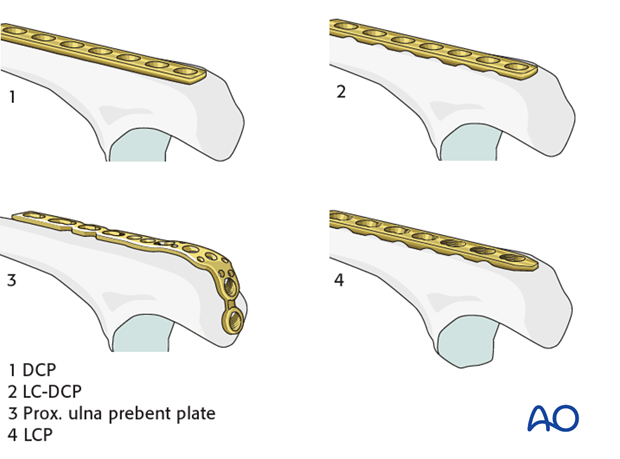
Prebending and contouring
Prebend the plate according to the surface anatomy of the ulna if needed.
Contouring of the plate is achieved with bending irons or a bending press.
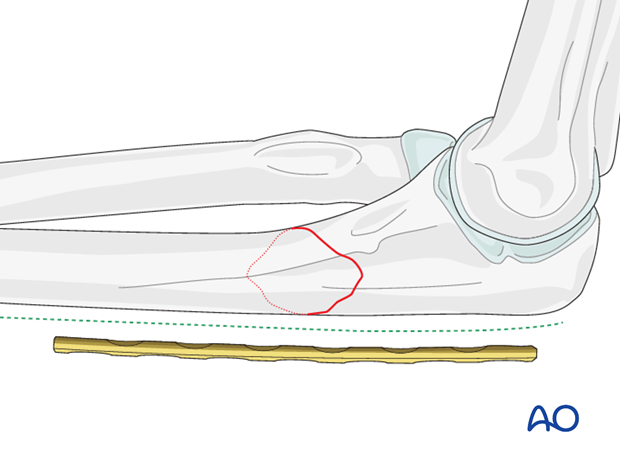
Plate position
The plate is placed on the posterior aspect of the ulna. This is the tension side of the bone and the plate will resist deforming forces best when placed here. Make sure that the proximal screws do not protrude into the joint.
Note: To improve proximal stability (short fragment and/or osteoporosis) a posterior plate can be curved around the olecranon and anchored with an axial screw.
2. Positioning and approach
Positioning
This procedure is normally performed with the patient either in a lateral position or in a supine position for posterior access.
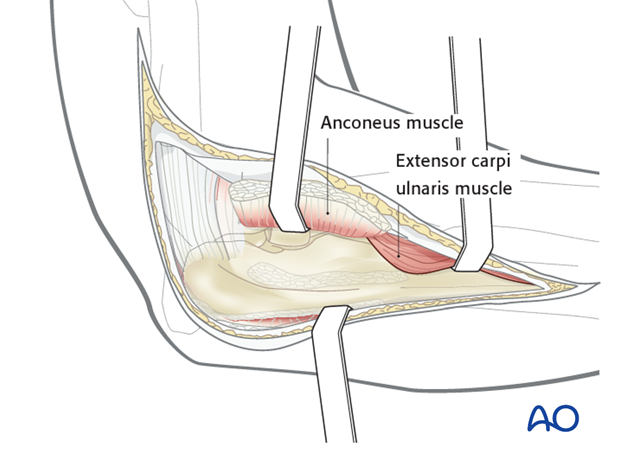
Approach
For this procedure a posterolateral approach is normally used.
3. Reduction and preliminary fixation
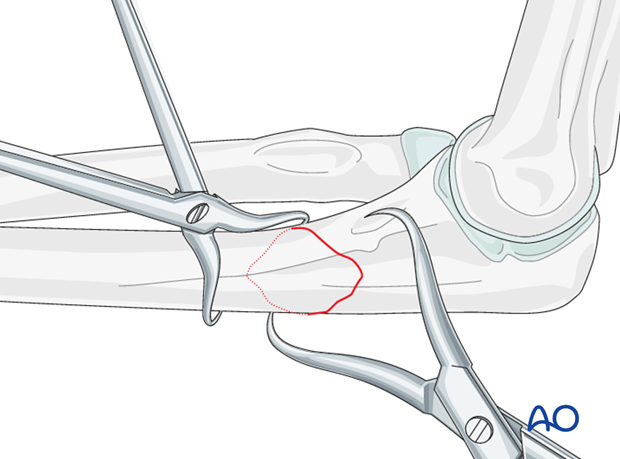
Cleaning of the fracture site
Expose the fracture ends with minimal soft tissue dissection off the bone.
Remove hematoma and irrigate.
Direct reduction
Reduce the fracture with the help of small pointed reduction forceps and provisionally fix with forceps or K-wires.
4. Lag screw insertion
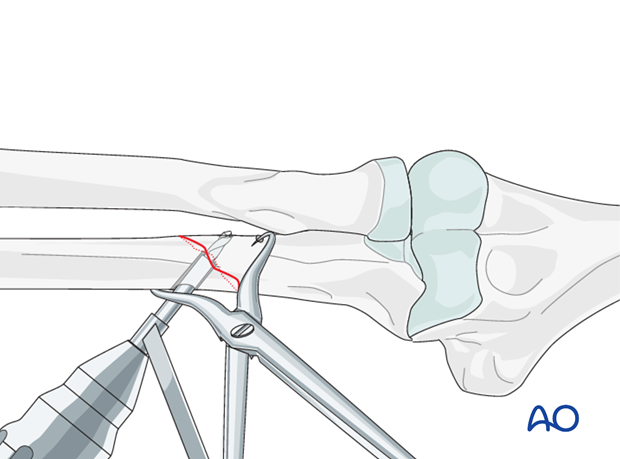
Drilling
Drill a 3.5 mm gliding hole for the lag screw into the posterior cortical bone of the distal fragment.
Insert the 2.5 mm drill sleeve into the gliding hole until it reaches the far cortical bone.
Now drill the far cortex with the 2.5 mm drill bit.
Countersink the cortex of the distal fragment in order to have more surface area to distribute the force caused by the head of the lag screw.
Measuring
Measure the depth of the hole with the hook of the depth gauge pointing proximally.
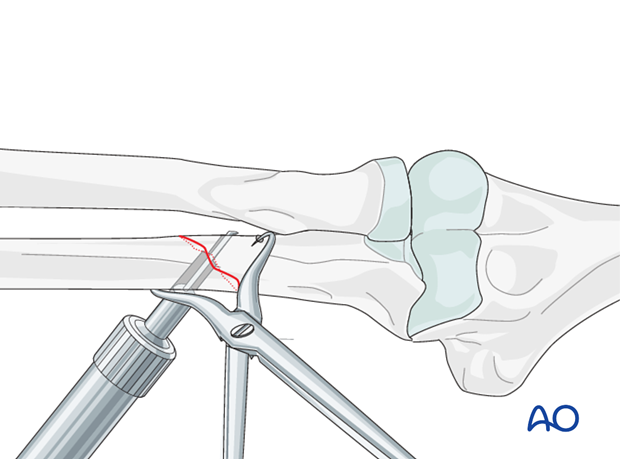
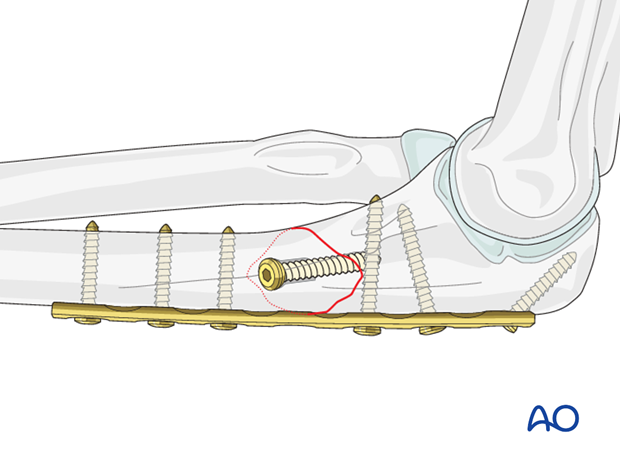
Lag screw insertion
Closely observe the compression effect on the fracture line while tightening the lag screw.
The reduction forceps should be removed just before the final tightening of the screw.
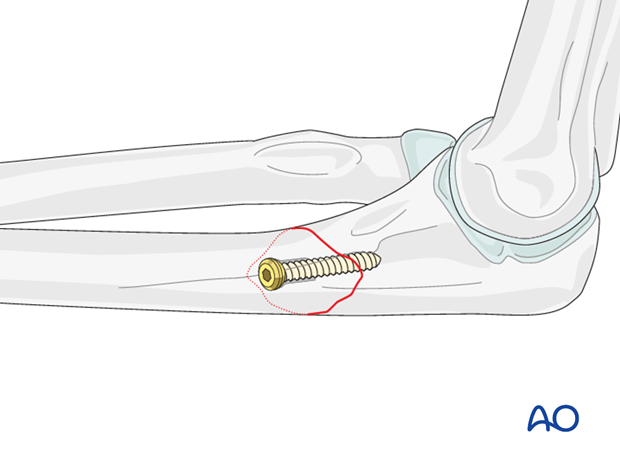
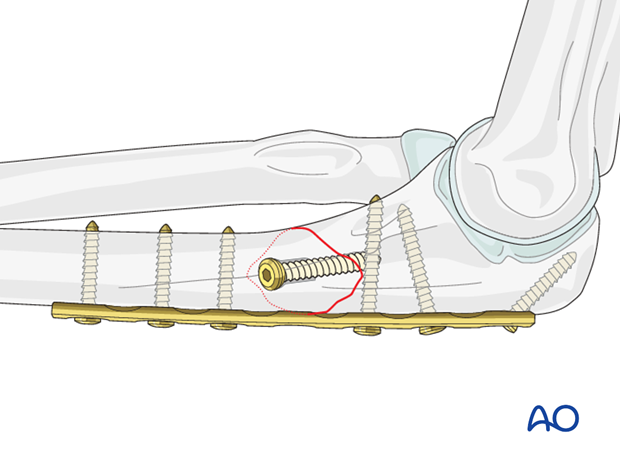
5. Protection plate
Plate fixation
Apply the contoured plate and fix it to the bone with three screws proximal and three screws distal to the fracture in neutral position to protect the lag screw.
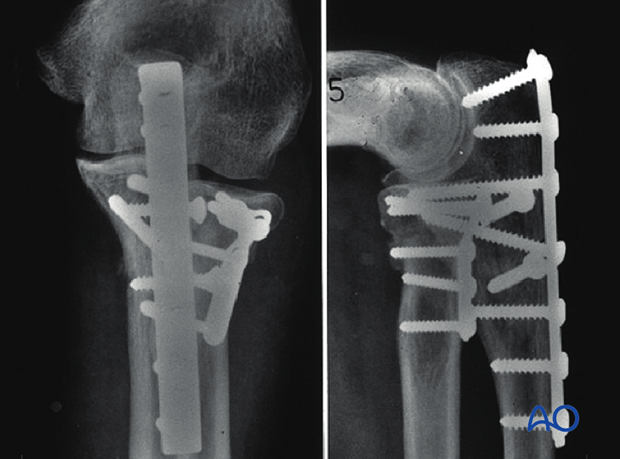
Final assessment
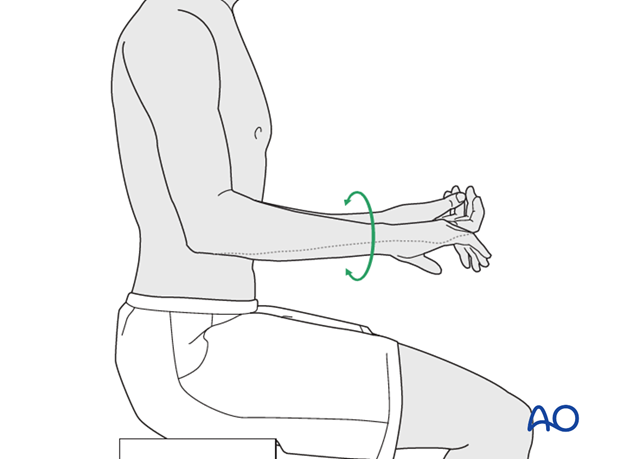
Finally, assess the range of motion in pronation, supination, flexion and extension.
Check results with image intensifier or x-ray.
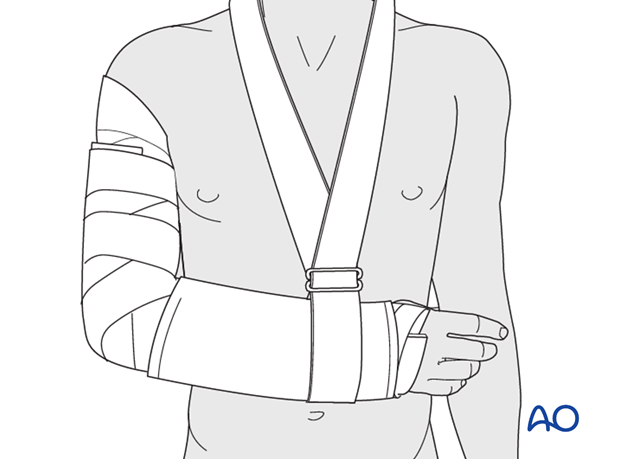
6. Postoperative treatment following ORIF
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
Mobilization
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
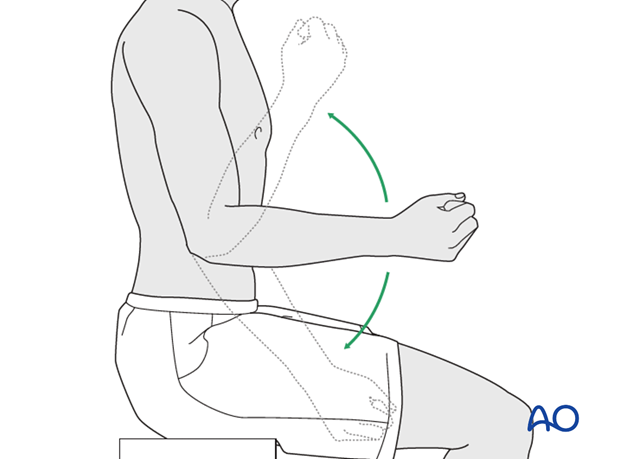
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













