Compression plate
1. General considerations
Preliminary remarks
Simple fractures of the proximal ulna are often associated with proximal radial injuries. Usually, the ulnar fracture will be fixed first. Malreduction of the ulna will impede reduction of the radius.
Compression plate principles
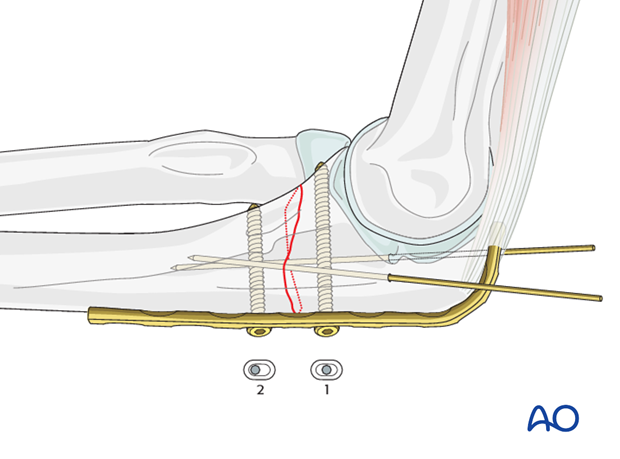
In transverse fractures, compression can only be achieved using a preloaded plate. Slight overbending of the plate is necessary to ensure compression of the far cortex. Sequence of screw insertion:
- The first screw should be inserted in neutral position.
- A second screw is inserted eccentrically into the opposite fragment.
2. Positioning and approach
Positioning
This procedure is normally performed with the patient either in a lateral position or in a supine position for posterior access.
Approach
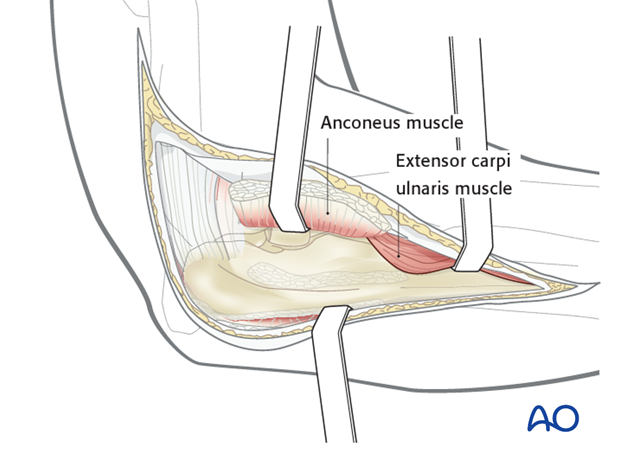
For this procedure a posterolateral approach is normally used.
3. Reduction and preliminary fixation
Prior to reduction, expose the fracture ends with minimal soft tissue dissection off the bone. Remove hematoma and irrigate.
Reduction can be achieved by direct or indirect reduction techniques.
Direct reduction
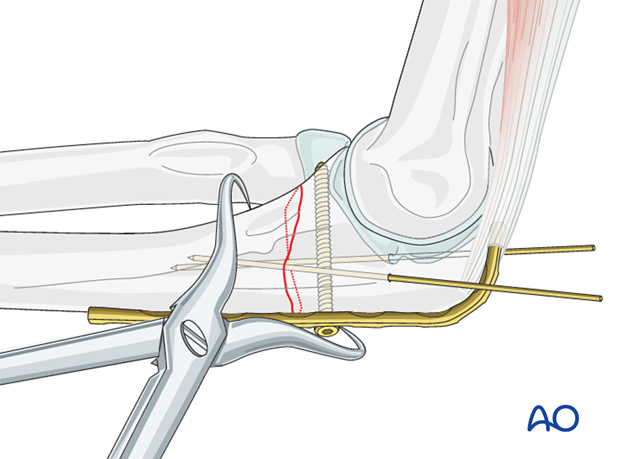
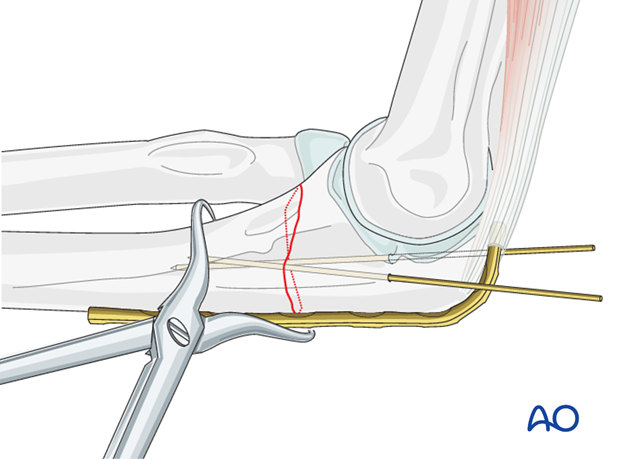
Reduce the fracture with the help of two small pointed reduction forceps ...
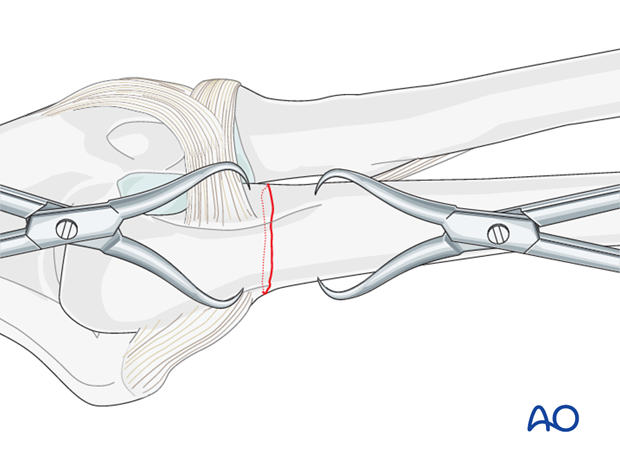
... and provisionally fix it with two K-wires or reduction clamps.
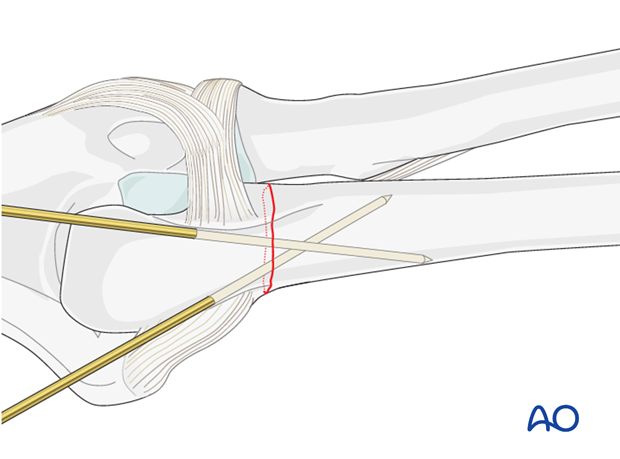
Reduction with a plate
Fix the contoured and pre-bent plate with one screw to the proximal fragment. Then reduce the distal fragment against plate and proximal fragment by manipulation of the distal ulna, possibly aided by a clamp outside the fracture site. Final adjustment of the screw may affect reduction and may be delayed until a screw is placed in the distal fragment.
4. Plate preparation
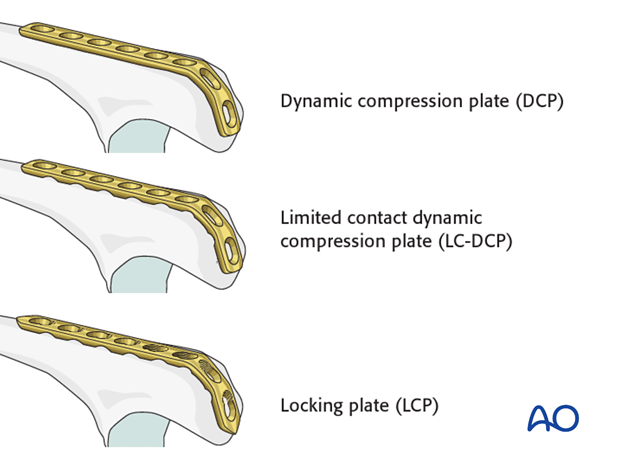
Implant choice
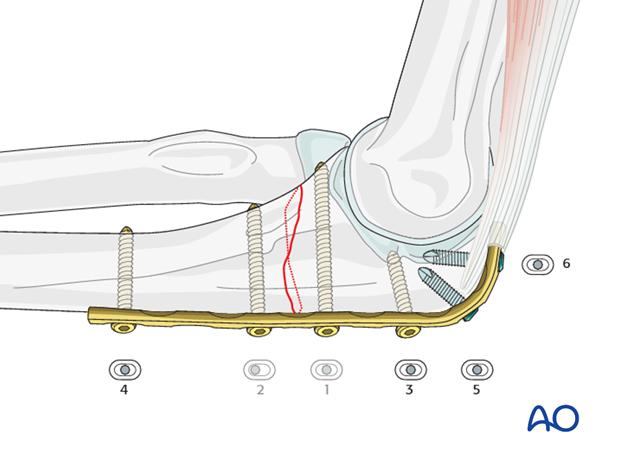
Plate length should be sufficient to place, usually, three screws in each fragment.
The plate may be a small fragment dynamic compression plate (3.5 DCP), or limited contact dynamic compression plate (LC-DCP), or locking plate (LCP) with conventional screws. More recently, use of 2.7 LCP has been reported.
Note: In osteoporotic bone, a LCP with locking head screws should be used, after insertion of a conventional lag screw through the plate.
Contouring the plate
Place a slight convex bend over the fracture to ensure compression of the opposite cortex.
Contour the plate with bending irons or bending press.
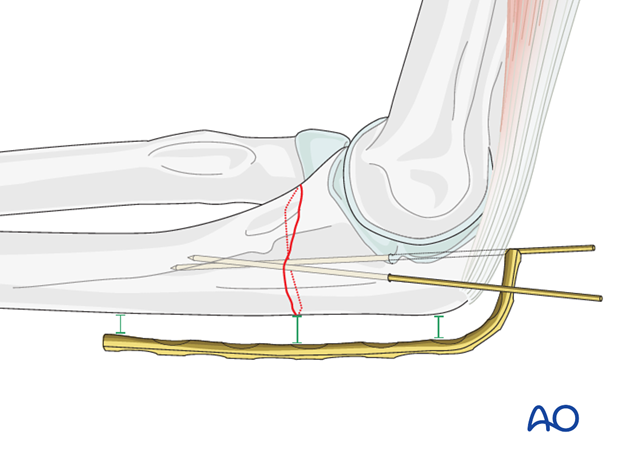
Plate application
Make a small cut in the triceps tendon to slide the plate under.
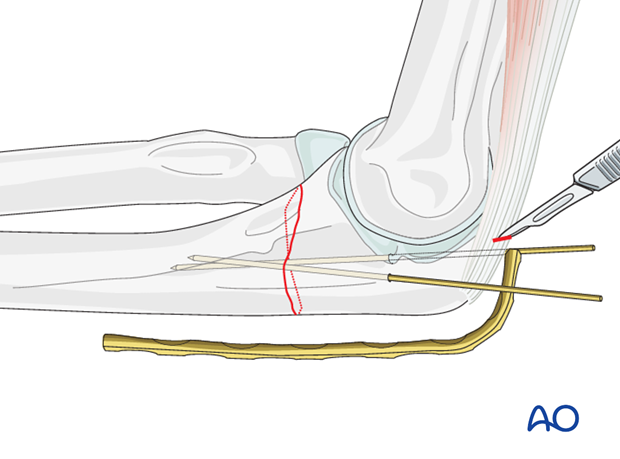
Apply plate and hold it against the bone with a bone clamp or one or two fingers.
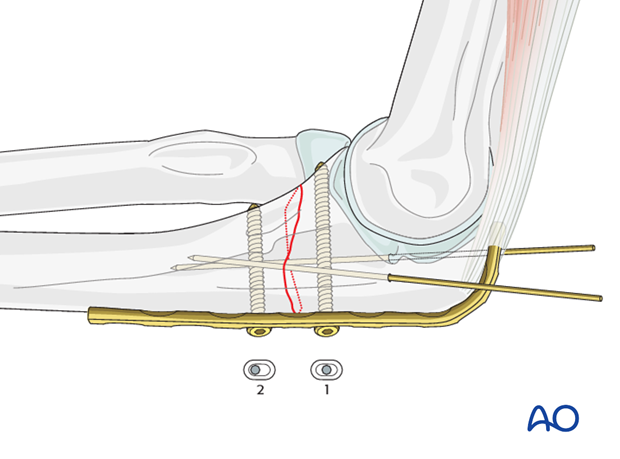
5. Creating compression
Apply a cortical screw in neutral position into the proximal fragment next to the fracture. The screw is inserted until it stabilizes the plate, but not fully tightened.
Insert a cortical screw in eccentric position into the distal fragment, next to the fracture, until it compresses the far cortex.
Both screws are then tightened completely.
6. Finish fixation
Insert the rest of the screws in neutral position and remove the K-wires.
7. Final assessment
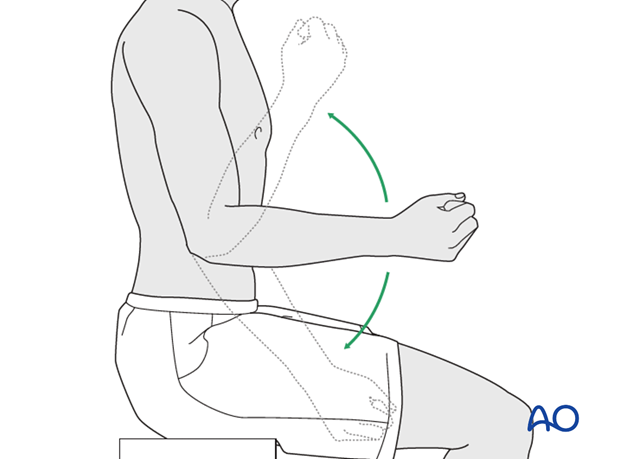
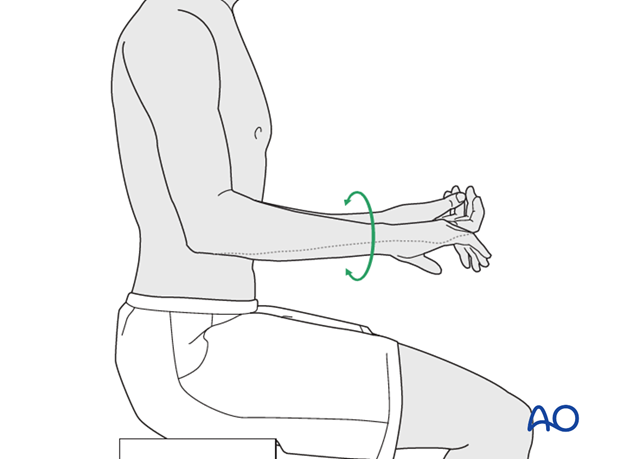
After fixation of the ulna, assess the range of motion in pronation, supination, flexion and extension. Fixation should be stable and crepitus or restricted motion should be absent. Radiocapitellar and ulnohumeral joints should remain located through a full range of motion.
Check results with image intensifier or x-ray.
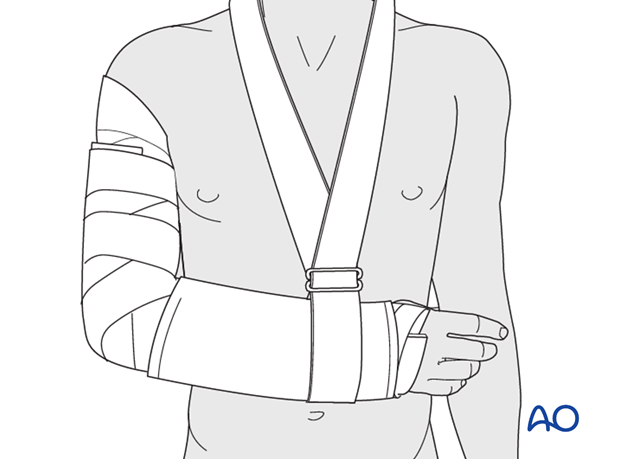
8. Postoperative treatment following ORIF
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
Mobilization
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













