Bridge plate
1. Principles of bridge plating
Preliminary remark
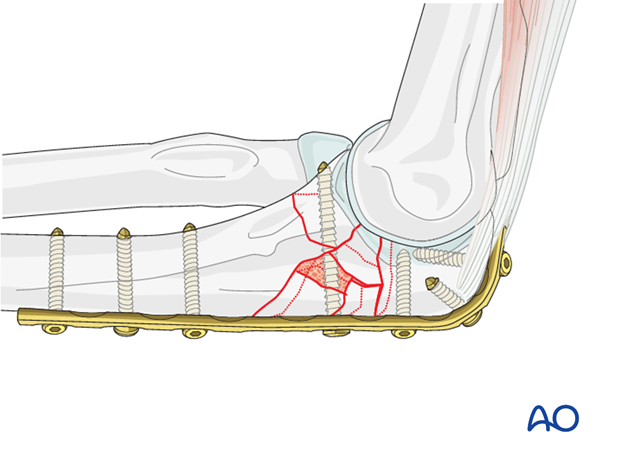
Absolute stability is desirable for articular fractures. However, this may not be possible in multifragmentary fractures of the proximal ulna. Every effort should still be directed at anatomical reduction and absolutely stable fixation of the major articular surface fragments, particularly the coronoid process. Compression will deform the articular surface, so it no longer fits the trochlea. In this situation, the fracture must be bridged without compression to preserve size and shape of the olecranon fossa. Small interfragmentary screws, K-wires, medial, or lateral miniplate may improve stability.
Bridge plating
A bridge plate is analogous to locked intramedullary nail fixation of a comminuted shaft fracture. In multifragmentary fractures of the olecranon, anatomical reconstruction of the articular surface itself is the primary goal. Intermediate, nonarticular fragments do not need to be reduced anatomically. Cancellous bone graft can be used to support the articular fragments and fill defects.
Directly manipulate only the articular fragments. Excessive manipulation of intermediate fragments risks disturbing their blood supply. If the soft tissue attachments are preserved, and the fragments are relatively well aligned, healing is predictable. Alignment of the main fragments can usually be achieved indirectly utilizing traction and soft tissue tension.
Mechanical stability, provided by the bridging plate, is adequate for indirect healing (callus formation).
2. Positioning and approach
Positioning
This procedure is normally performed with the patient either in a lateral position or in a supine position for posterior access.
Approach
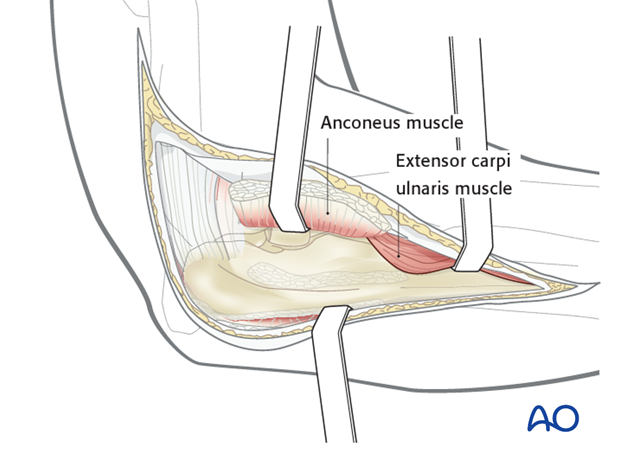
For this procedure a posterolateral approach is normally used.
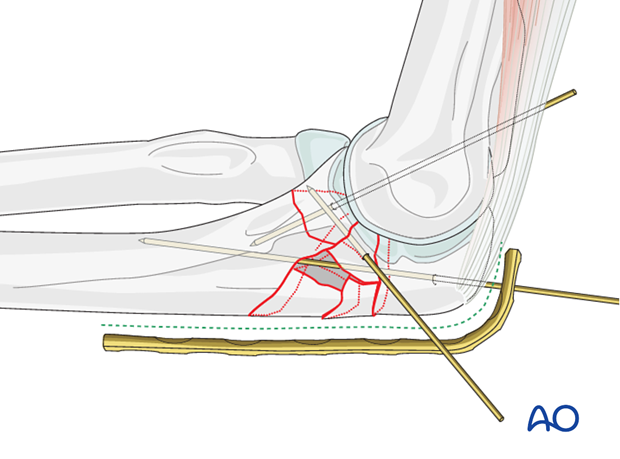
3. Reduction
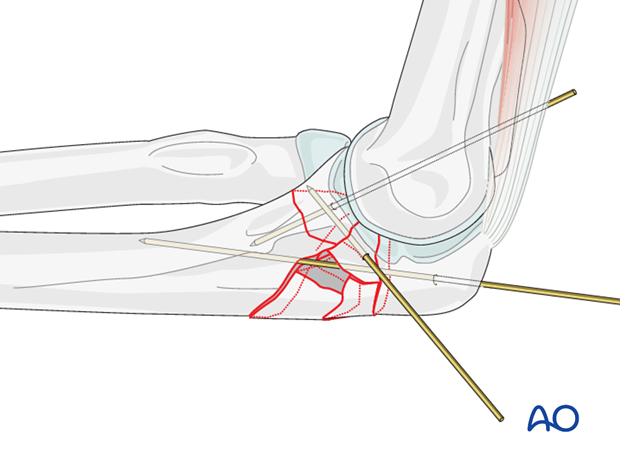
Through a posterior incision, release the joint capsule medially and laterally at the fracture site. With direct visualization, manipulate and anatomically reduce the articular fragments. Use the distal humerus as a template for reduction. Provisionally fix the fragments with 1.0 mm K-wires.
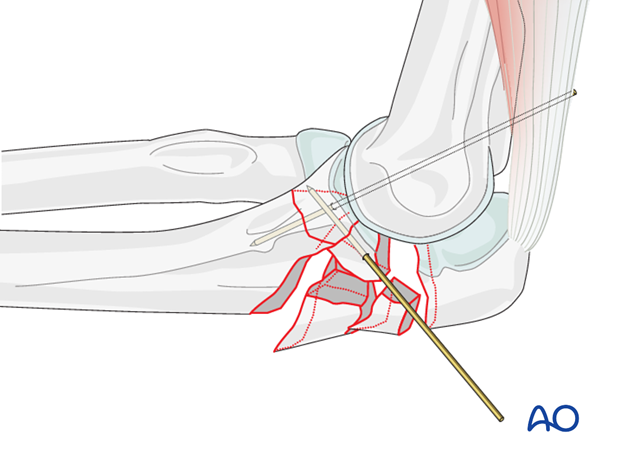
Reduce the proximal part of the olecranon with pointed reduction forceps and temporarily hold the reduction with one or two K-wires.
Insert all K-wires in a position where they do not interfere with the planned plate and screws.
Control reduction with direct visualization of the sigmoid notch and the posterior cortex of the olecranon, and confirm with C-arm fluoroscopic control.
4. Plate preparation
Implant choice
Use a 3.5 dynamic compression plate (DCP), reconstruction plate, limited contact dynamic compression plate (LC-DCP), or locking plate (LCP). The reconstruction plate is the least durable, and should be used cautiously as a bridged plate.
Choose the length of the plate so that at least three screws can be inserted in the most proximal fragment and three in the diaphysis.
If the fracture is very proximal or in osteoporotic bone, a preshaped olecranon LCP with locking head screws can be used to allow better fixation.
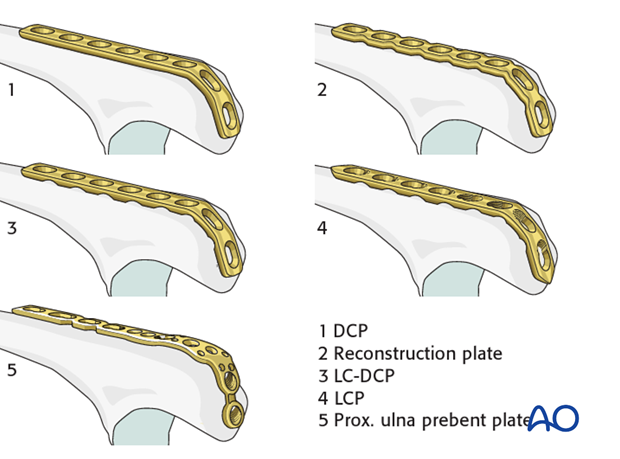
Plate contouring
If an anatomic plate is not used, contour the plate to fit the proximal ulna, bending around the tip of the olecranon. Make sure to follow the curvature of the olecranon.
Contouring is done with bending irons and bending press.
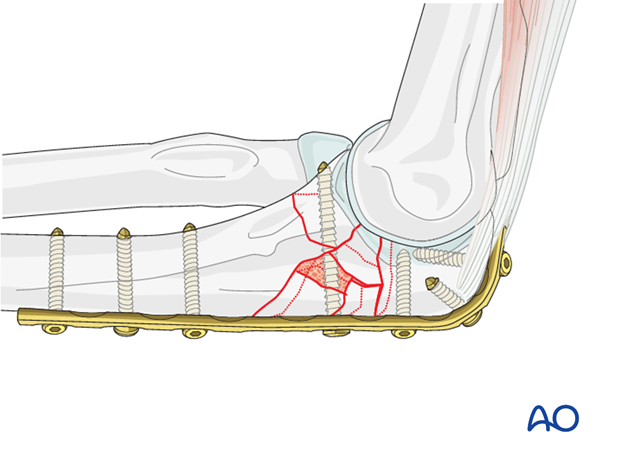
5. Proximal plate fixation
Split the triceps attachment
To achieve close bone plate contact, split the triceps attachment before positioning the plate.
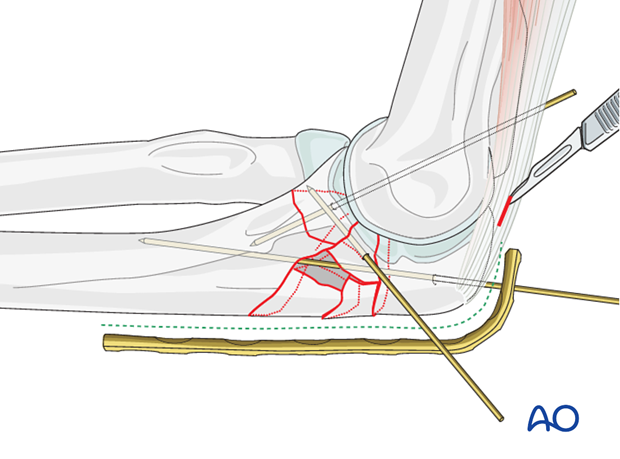
Proximal plate fixation
Anchor the plate with three screws to the proximal olecranon. Make sure that the screws do not protrude into the joint.
Whenever possible, insert the screws bicortically, aiming the drill to the lateral or to the medial cortex.
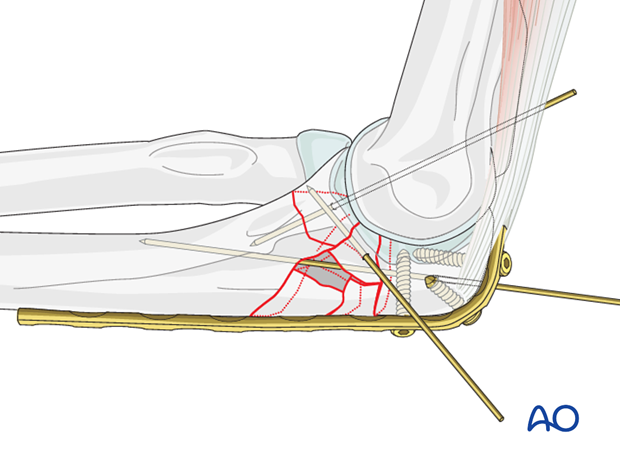
6. Distal plate fixation
Insert three bicortical screws in the distal fragment and in a divergent pattern.
Make sure to maintain contour and size of the olecranon’s articulation.
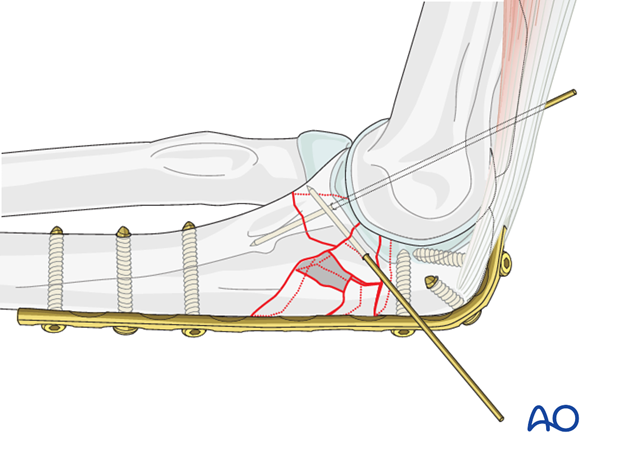
Bone graft
Large defects may be filled with bone graft.
K-wires are then removed.
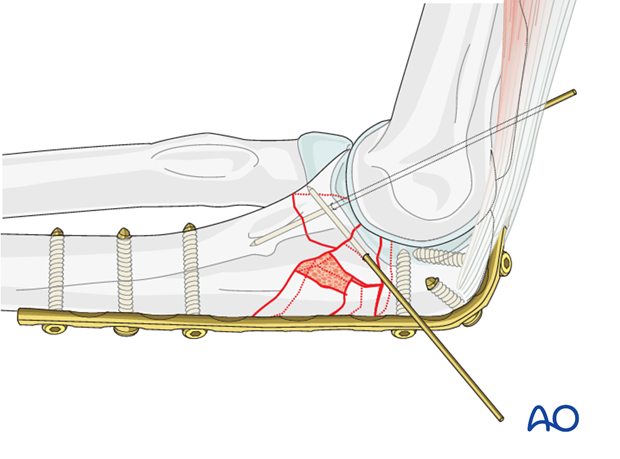
7. Possible fixation of a large coronoid fragment
Reduction of a large coronoid component of multifragmentary proximal ulna fractures can often be done through the fracture site. Provisional or definitive fixation can be placed at that time, but sometimes it helps to use a screw through a posterior plate for its fixation, as shown here. Insert this as a lag screw, as perpendicularly as possible to the fracture plane at the base of the coronoid. Smaller diameter screws may be better.
For further information on the fixation of coronoid fractures, see “Repair of coronoid fracture”.
8. Postoperative treatment following ORIF
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
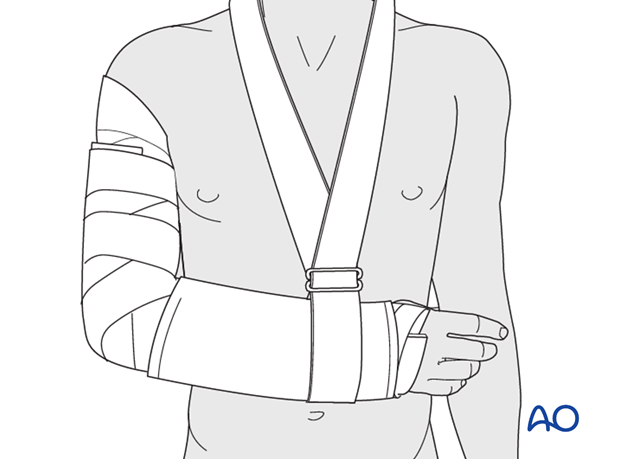
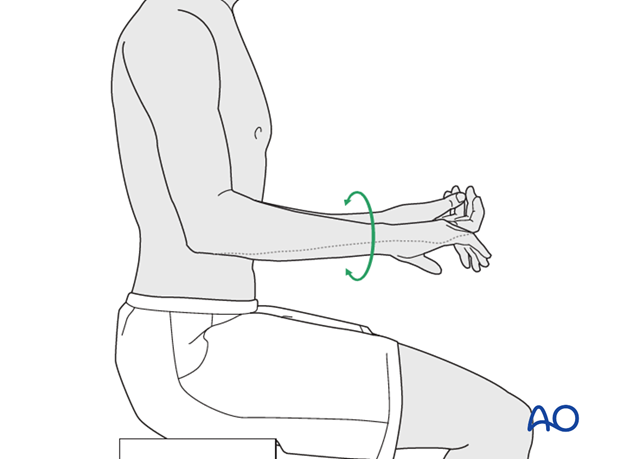
Mobilization
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
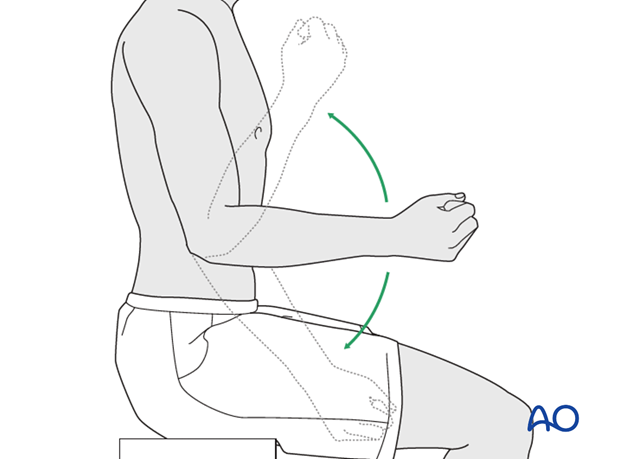
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













