Simple two-part pertrochanteric fractures
Definition
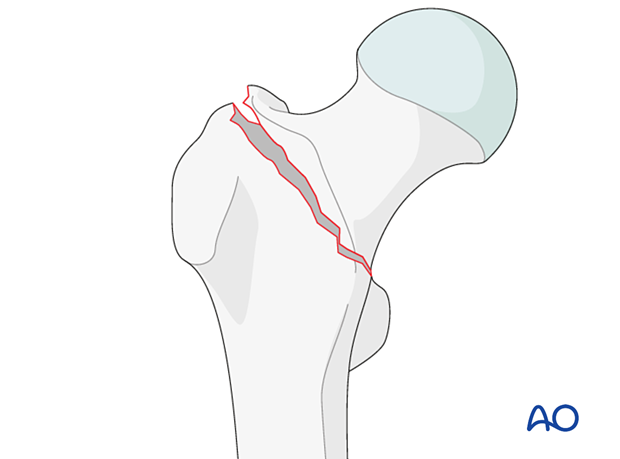
Simple two-part pertrochanteric fractures with an intact lateral wall are classified by AO/OTA as 31A1.2.
In these fractures, the fracture line can begin anywhere on the greater trochanter and end either above or below the lesser trochanter.
There are only two fragments, and the medial cortex is interrupted in only one place. An additional small coronal fragment may be present but will not change the fracture management.
The lesser trochanter, the so-called medial buttress, remains attached to one of the two fragments.
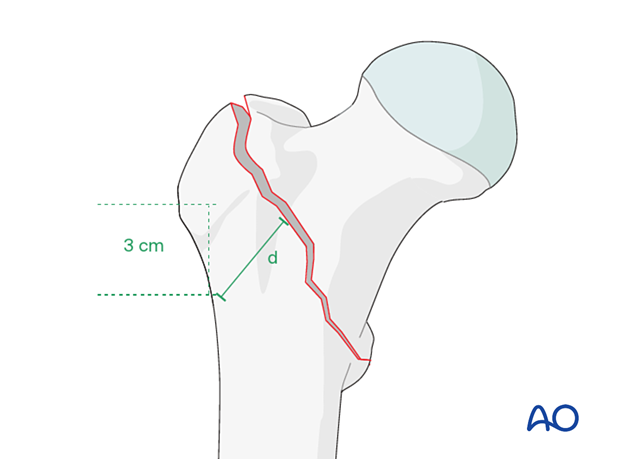
Lateral wall height of greater trochanter
The coding system separates the pertrochanteric fractures into two groups (A1 and A2) defined by the lateral wall height (d) of the greater trochanter.
Lateral wall height or thickness is defined as the distance in millimeters (mm) from a reference point 3 cm below the innominate tubercle of the greater trochanter angled 135° upward to the fracture line on the AP x-ray. The thickness (d) must be less than 20.5 mm for the fracture to be considered an A2 fracture (Hsu et al 2013). It is recommended that the measurement for the lateral wall be taken using the traction view with the leg in neutral rotation. This can be difficult to obtain preoperatively but should be assessed fluoroscopically following operative closed reduction but before implant selection. Alternatively, preoperative 3-D CT provides detailed mapping of fracture location and planes.
Further characteristics
These fractures are stable after reduction and fixation, largely because of the excellent contact of the fracture surfaces and no bone loss.
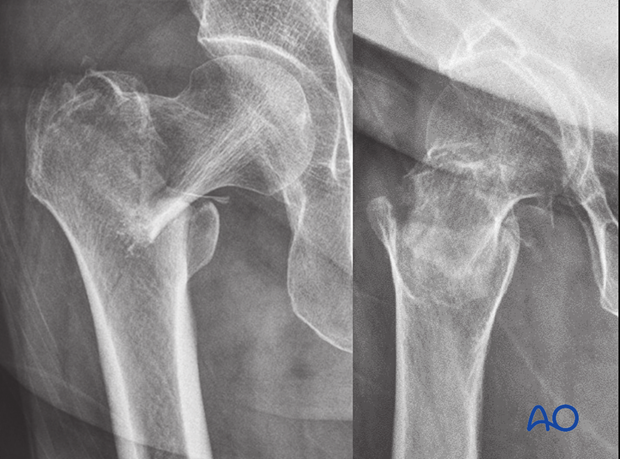
Case requiring percutaneous or open reduction
AP and lateral x-rays of a simple pertrochanteric two-part fracture. The anteromedial neck is displaced into the medullary canal.
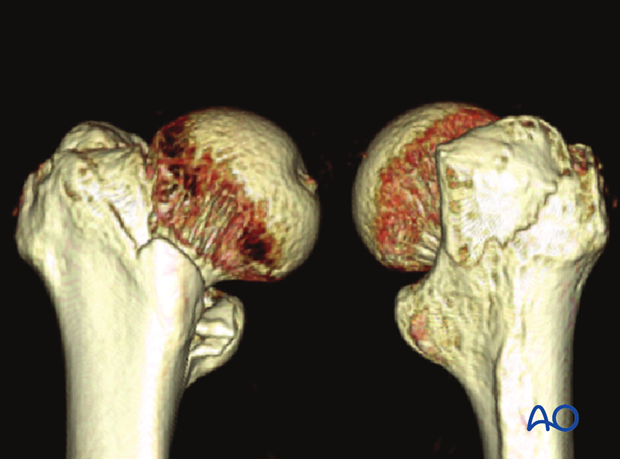
3-D CT views of the same case
Irreducible intertrochanteric fracture
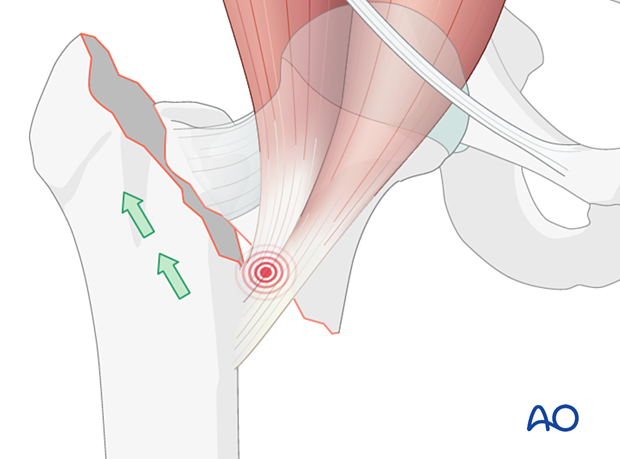
Superolateral displacement of the shaft after high-energy trauma is a sign of an irreducible intertrochanteric fracture.
If the lesser trochanter is attached to the proximal fragment, the pull of the iliopsoas muscle will flex and externally rotate the proximal fragment, and traction will not correct this displacement.
Occult hip fractures
An undisplaced fracture may also be referred to as occult fracture as it is often not visible and may not be diagnosed correctly.
If clinical assessment indicates a neck fracture, but the x-ray does not show clear signs of it, CT or MRI imaging is recommended.













