Assessment of patients with a proximal femoral fracture
1. Clinical examination
Consider the history of the injury.
Check for swelling and bruise. This indicates an extracapsular, ie, trochanteric, injury.
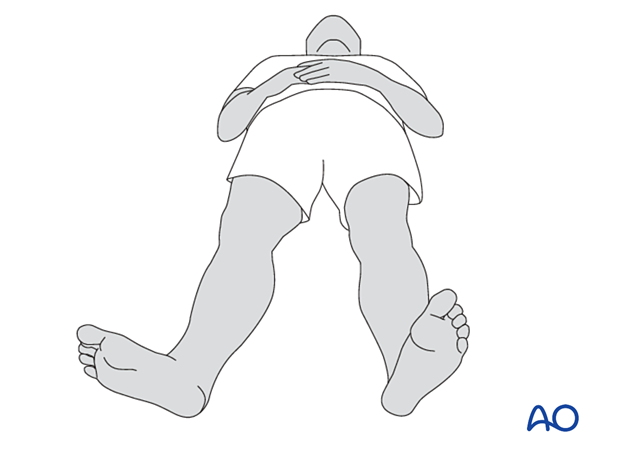
Check for the degree of external rotation of the leg and compare it to the contralateral leg.
A femoral neck fracture is intracapsular and will have less external rotation.
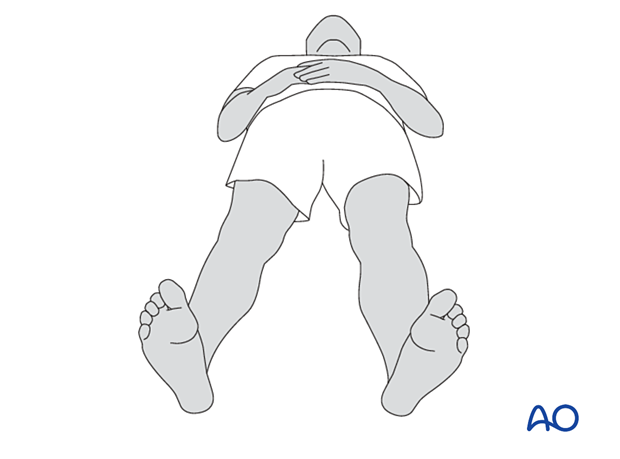
Trochanteric fractures allow greater external rotation.
Medial thigh pain without visible deformity suggests an impacted or undisplaced fracture.
2. Radiological examination
X-rays
For proper radiological evaluation, x-rays in two planes at 90° to one another are necessary.
In the presence of a fracture, the lateral radiograph may be obtained by taking a so-called cross-table view. Rotate the limb 15° internally to get a lateral view of the proximal femur. Direct the x-ray beam at a 45° angle to the straight leg through the center of the femoral head.
If this is of good quality, it will allow the surgeon to assess the degree of retroversion and the degree of fragmentation of the posterior cortex.

CT imaging
If the trauma plain films show a potentially unstable fracture but do not give enough detail about the fracture morphology, 3-D CT imaging is a powerful tool for better diagnosis and planning for surgery.
3. Trochanteric fractures
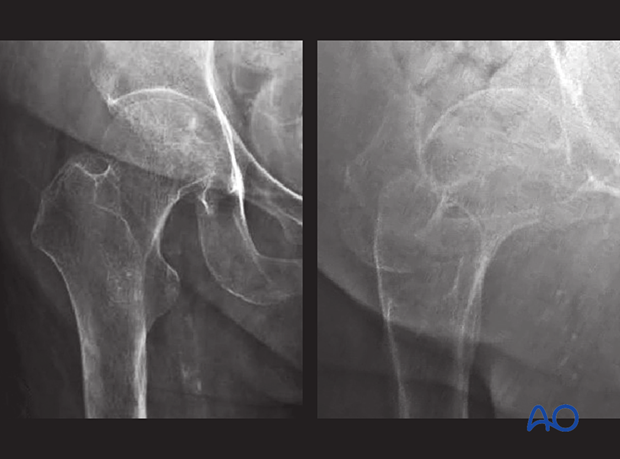
Plain x-ray imaging
Plain x-rays are often sufficient to diagnose simple trochanteric fractures.
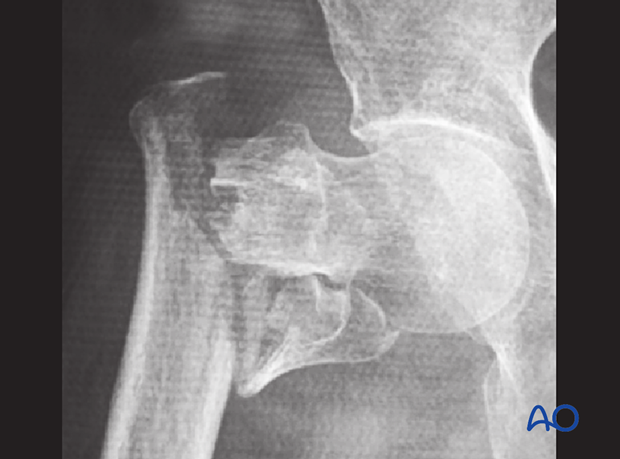
If the fracture is displaced, especially with rotation, the fracture morphology and type can often not be diagnosed properly.
Traction AP view may be considered to achieve better images for diagnosis. But this is usually painful to the patient.
CT imaging is the better option in this case.
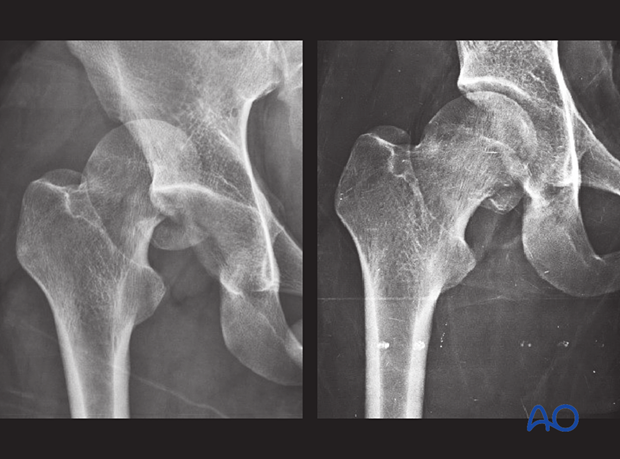
In this x-ray, the fracture is displaced with rotation and varus.
Indications for CT imaging
In the following cases, CT imaging is recommended:
- Difficulty identifying the primary fracture line
- Lateral wall broken
- Additional anterior cortical fragment
- Intertrochanteric fracture with comminution
For trochanteric fracture assessment with 3D CT imaging, see, eg, Cho et al (2017).
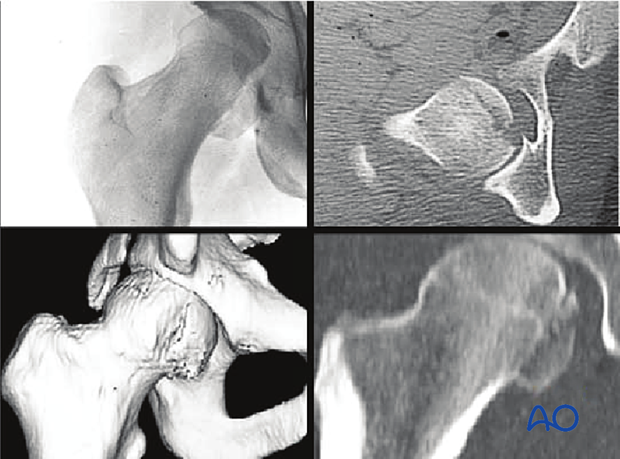
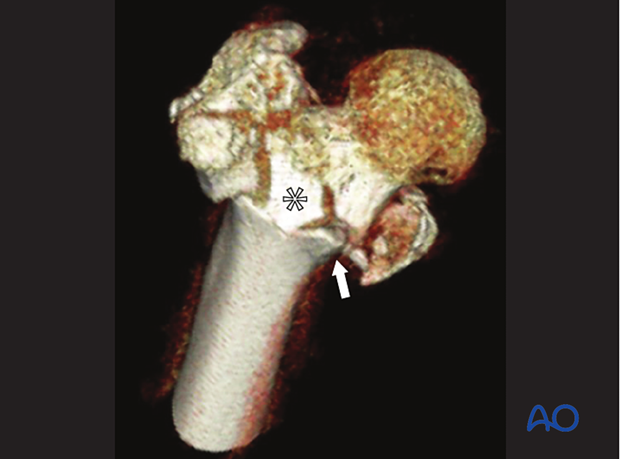
CT imaging
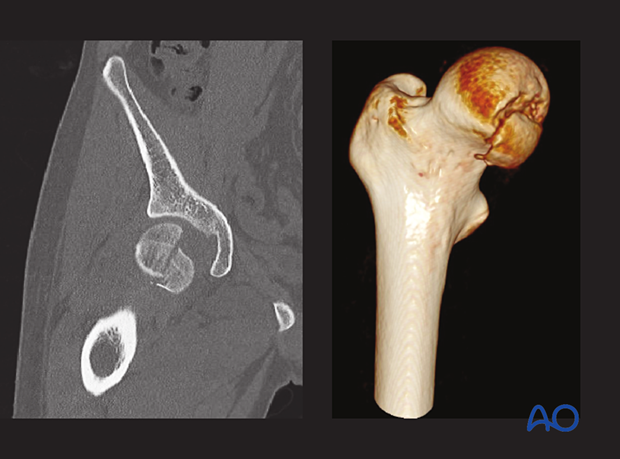
With 2-D images, it is often difficult to recognize the 3-D fracture morphology of trochanteric fractures.
In the 3-D CT, the fragmentation pattern becomes more readable and helps understanding the fracture personality, decision making, and preoperative planning.
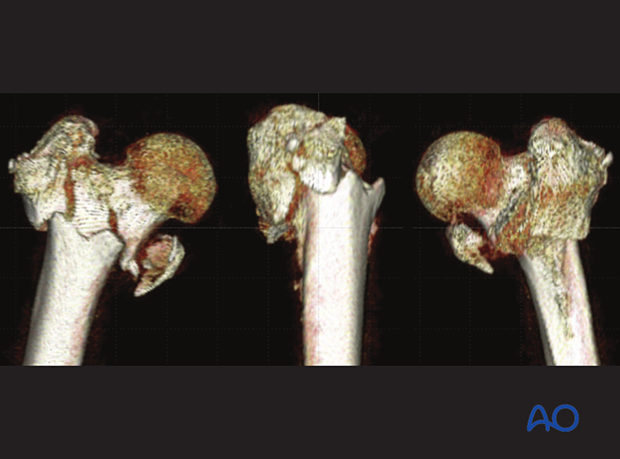
In this case, the anterior cortex contact is very limited (arrow) due to an additional anterior fragment (asterisk).
4. Imaging after hip reduction
After closed reduction of the hip, x-ray evaluation of the reduction is necessary.
Osteochondral fragments, ie, incongruency of the femoral head after dislocation, may be overlooked on conventional x-rays. CT scans are recommended, especially if nonoperative treatment is planned.
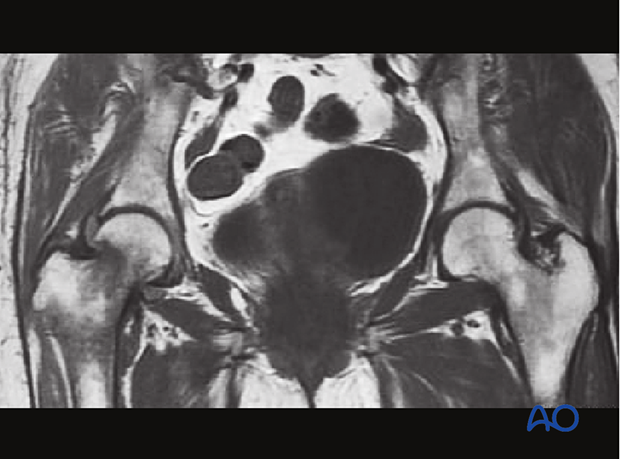
5. Occult hip fractures
An undisplaced fracture may also be referred to as occult fracture as it is not well visible in an x-ray and may not be diagnosed correctly.
If clinical assessment indicates a neck fracture, but the x-ray does not show clear signs of it, CT or MRI imaging is recommended (Davidson et al 2020).
6. Femoral neck fractures
Displaced femoral neck fractures show disruption of the medial and lateral cortical line in the AP x-ray.
In the lateral view, abnormal anteversion or retroversion should be recognized.
3-D CT imaging is highly recommended to understand the morphology of the fracture and comminution.
7. Femoral head fractures
CT is standard imaging as it provides the most accurate information of the fracture.
If CT is not available, AP and lateral views of the hip and Judet views of the pelvis are needed after closed reduction of the hip. The diagnosis is often missed in case of small fractures, but even larger fractures are not always apparent on a standard pelvic x-ray.
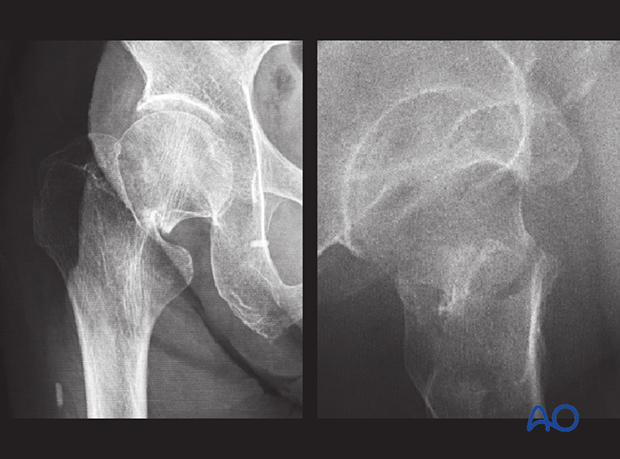
This case shows a femoral head split fracture. On the left x-ray, the dislocation is visible. On the right one, the hip is reduced, with the split fragment still displaced.
8. Combined fractures
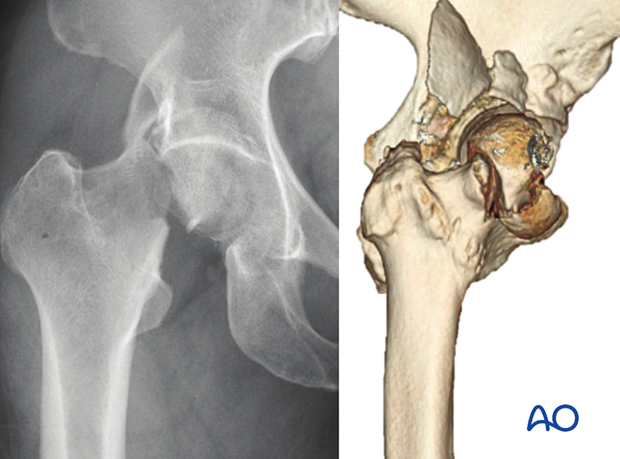
In combined fractures of the greater trochanter, the femoral head and neck, and/or the posterior wall of the acetabulum, CT imaging is necessary for recognizing the fracture pattern, decision making, and preoperative planning.
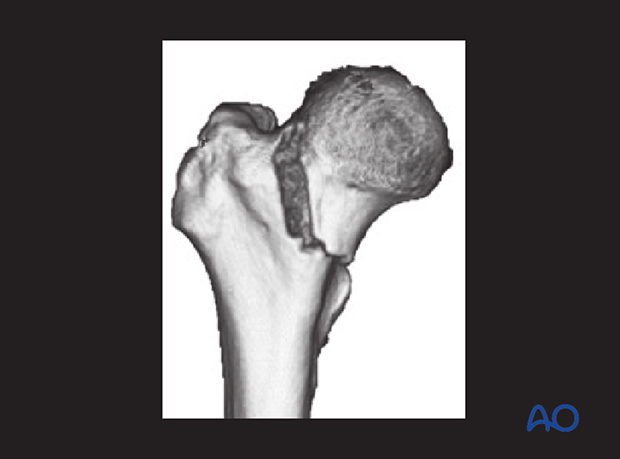
This case shows a femoral neck and head fracture combined with a posterior wall fracture and hip dislocation.
This case shows a femoral head and posterior wall fracture.