Complications and technical failures in trochanteric fracture management
1. General considerations
Factors influencing the outcome
Four main factors influence the outcome:
- Bone quality
- Fracture pattern
- Quality of reduction
- Implant positioning
The first two factors should be considered during decision making and selection of treatment.
The last two factors can be controlled during surgery. Therefore, it is important to achieve good anatomical reduction and apply the selected implant properly.
Augmentation in poor-quality bone
In severely osteoporotic bone, implant pull-out, cut-out, and cut-through, and collapse may result even if good reduction and fixation have been achieved. Consider augmentation with PMMA cement to improve the hold of screws and blades.
Types of technical failures
Technical failures in fixation of trochanteric fractures mainly include:
- Varus collapse
- Too much valgus reduction with a medial gap
- Lag screw/blade malposition
2. Pitfalls in fracture diagnosis
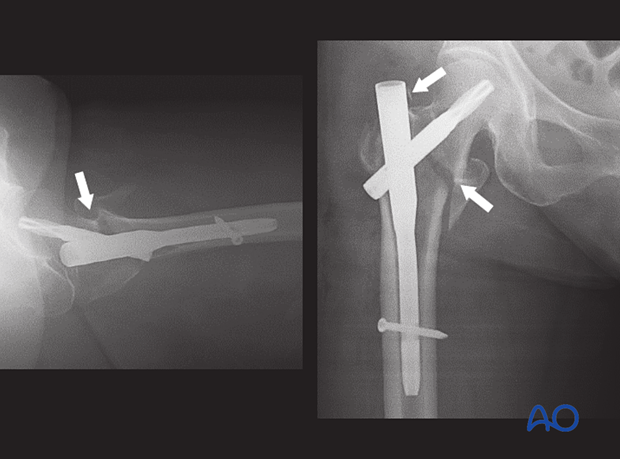
In this case of an elderly patient, the apparent trochanteric fracture has been treated with a short nail fixation. The postoperative x-ray shows failure (arrow).
The primary fracture line exits medially through the femoral neck and should have been treated as a femoral neck fracture.
In the AP x-ray, it is difficult to interpret the fracture pattern correctly as fragments overlap. A CT is strongly recommended in such a case.
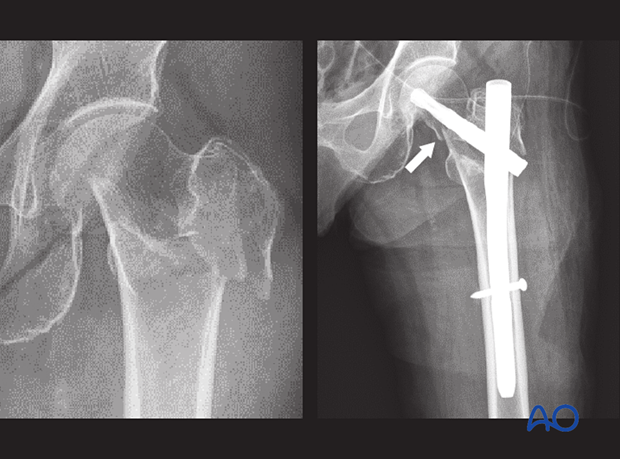
The one-year follow-up x-ray shows excessive collapse with penetration of the acetabulum.

3. Pitfalls in reduction and fixation
Irreducible intertrochanteric fracture
It is important to recognize an irreducible intertrochanteric fracture and treat it with open reduction and fixation.
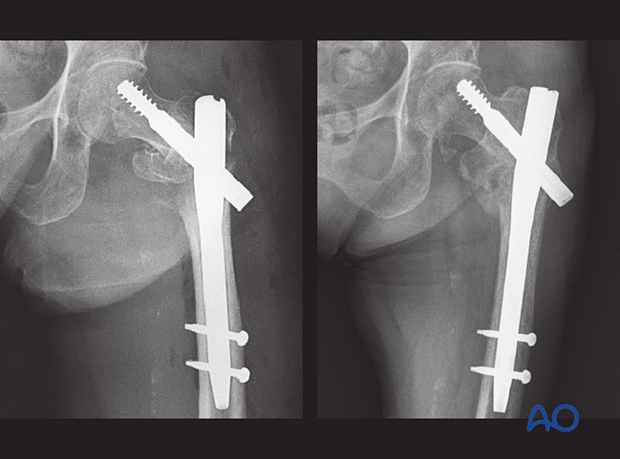
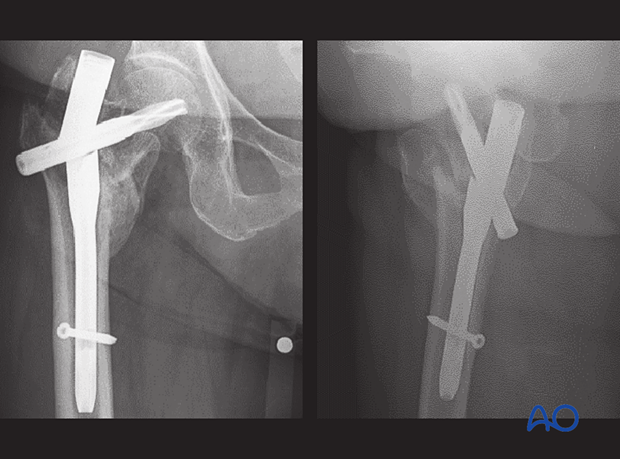
In this case, nail fixation has been chosen. In the postoperative x-ray, the remaining fracture displacement is visible. This led to severe collapse, seen in the follow-up x-ray.
Anatomical realignment, with open reduction if necessary, can help to avoid such an outcome.
Valgus deformity with a medial gap
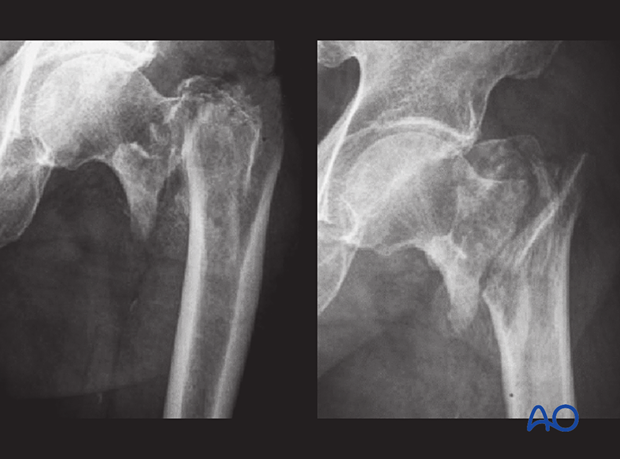
In this case, the valgus deformity with a medial gap has not been reduced anatomically before nail fixation.
The superolateral part of the proximal fragment prevented the fracture from sliding along the blade axis. The medial gap remained open and too big to be bridged with callus, which resulted in nonunion.
Although the nail has been inserted correctly, the lack of sliding and medial support led to metal failure of the nail.
Malreduction
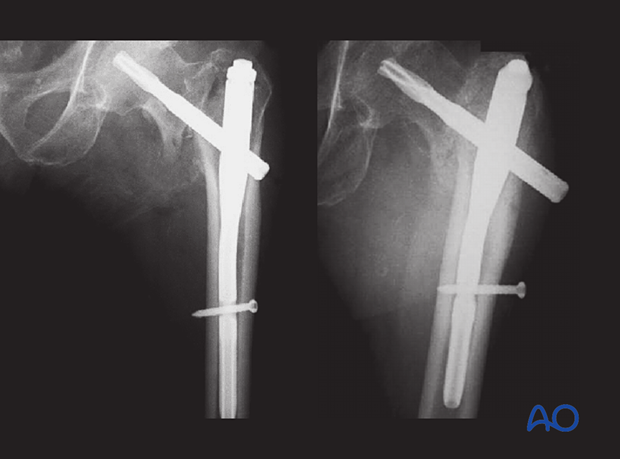
This case shows a trochanteric fracture with severe varus deformity.
The decision has been made to treat it with a short nail.
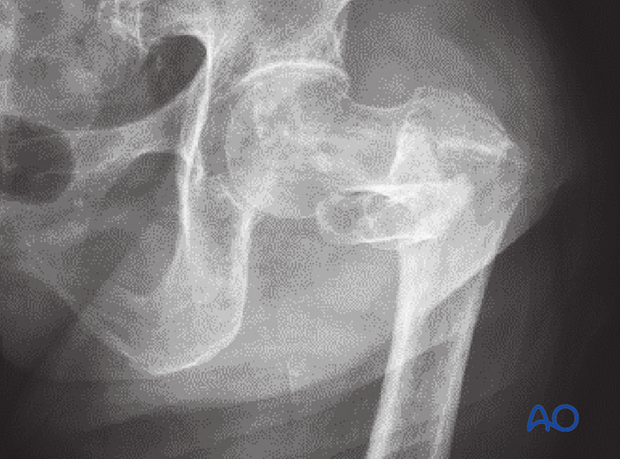
The postoperative x-ray shows insufficient correction of the varus deformity.
Consequently, the lag screw could not be inserted in line with the head-neck axis (mismatch of implant angle and bone in varus deformity).
Prevention: Although it is difficult to reduce severe varus deformities, anatomical fracture alignment is necessary for proper implant insertion.