ORIF - Mini-fragment or headless screws
1. General considerations
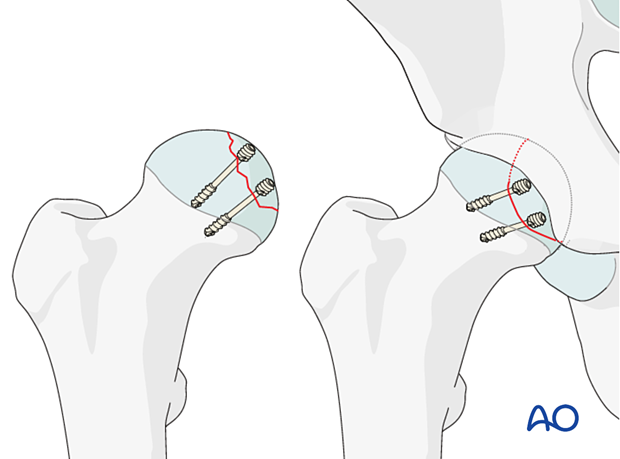
Principles of screw fixation
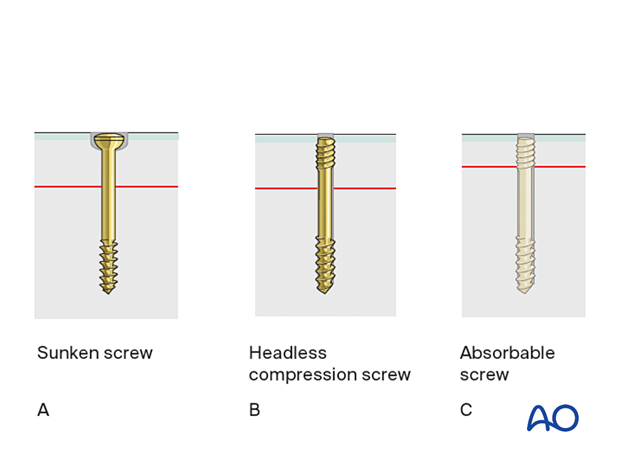
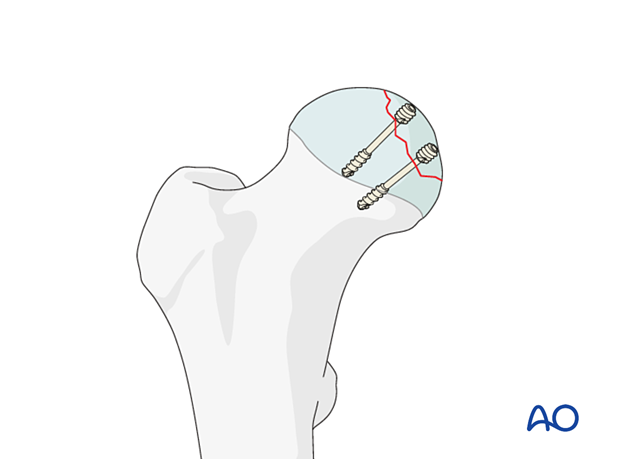
Articular fragments need to be reduced anatomically and may be stabilized with absorbable screws, recessed small cancellous lag screws, or headless compression screws.
For rotational stability, two screws should be used in each fragment if possible.
Prognosis of stabilized split fractures of the femoral head
The outcome of stabilized suprafoveal split fractures remains unpredictable even after anatomical joint restoration.
Treatment of hip dislocation
In general, fractures of the femoral head are associated with dislocation of the hip. In 90%, the dislocations are posterior and in 10% anterior.
An unreduced dislocation is an emergency because it threatens the blood supply to the head, and it may also be accompanied by pressure on a major nerve. Therefore, a reduction must be performed as an emergency.
If a closed reduction succeeds, one can investigate the patient further with a CT to develop an appropriate treatment rationale.
If a closed reduction fails, an emergency open reduction must be undertaken.
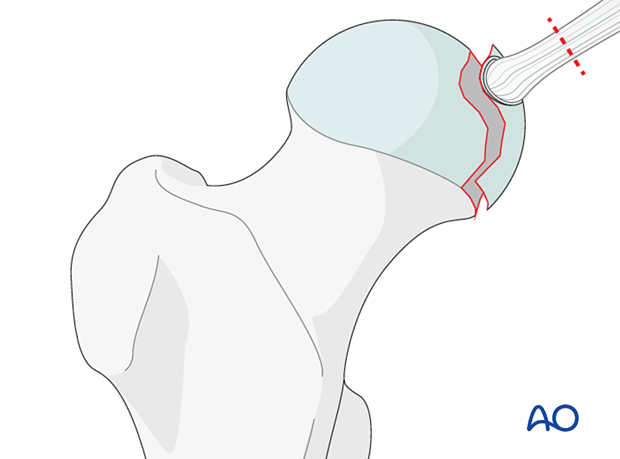
If a large medial fragment blocks an anatomical reduction of the hip, consider incising the ligamentum teres to which the fragment is often still attached; then fix the fragment through the articular surface.
Imaging after hip reduction
After a closed reduction of the hip, an x-ray evaluation of the reduction is necessary.
Osteochondral fragments, their location, and incongruence of the femoral head and joint after dislocation may be overlooked on conventional x-rays. CT scans are always recommended.
Implant selection
Absorbable screws do not need removing but may be relatively weak.
If metal screws are used, titanium is a better choice than steel, as it does not interfere with subsequent MRI imaging.
When inserted subchondrally, intraosseous headless compression screws cause less damage to the articular cartilage than conventional screws, and there is less risk of a prominent screw head causing secondary articular surface damage.
2. Patient preparation and approaches
Patient preparation
Position the patient either supine on a radiolucent table or in a lateral decubitus position.
Approaches for open reduction
For this procedure, the following approaches may be used for open reduction:
3. Open reduction
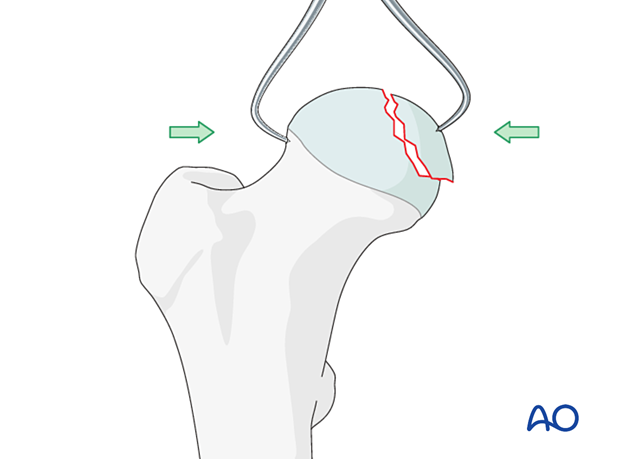
Reduce the fragment directly and maintain reduction with pointed forceps. This is most commonly done with the hip dislocated employing a trochanteric osteotomy.
4. Fixation
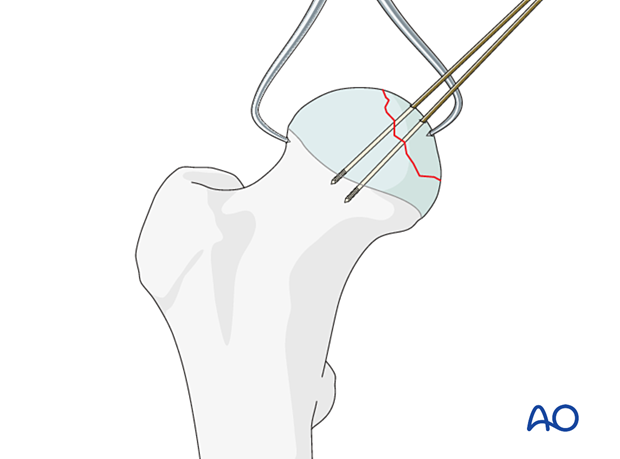
Preliminary fixation
Before definitive fixation with screws, secure the fragment with a minimum of two K-wires to avoid rotational redisplacement during screw insertion.
Definitive fixation of the fragment
Fix the fragment with either recessed small cancellous lag screws or headless compression screws.
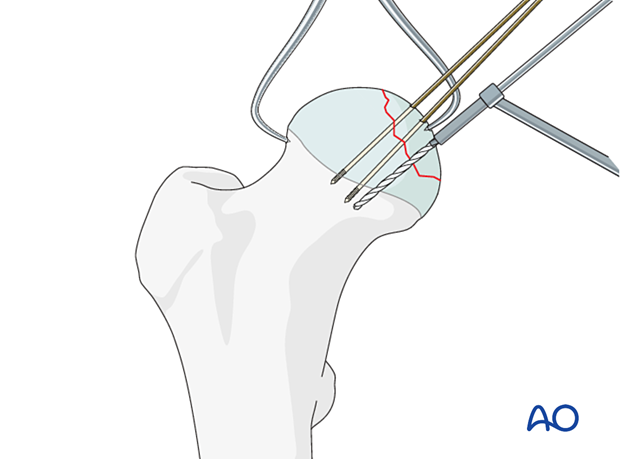
Number and size of screws
Choose screws long enough so that the thread is beyond the fracture line.
A single screw does not provide rotational stability. If the size of the fragment allows, use at least two screws.
5. Aftercare
Dislocation precautions
Since most femoral head fractures are associated with a hip dislocation, precautions against redislocation should be taken for the first 6 weeks after injury.
Low seats and toilets, flexing the hip when arising, sitting with legs crossed, as well as squatting and kneeling may also be avoided initially, as should pivoting on the affected leg. The patient and caregivers may be encouraged to use additional support when rising from a sitting position.
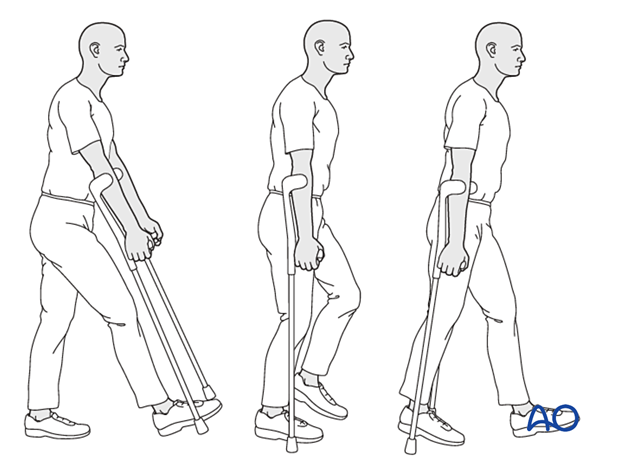
Postoperative mobilization
Since the fractures are articular, weight-of-the-leg weight bearing is advised up to 8 weeks and then advanced.
Range-of-motion exercises should start cautiously in the immediate postoperative period to prevent stiffness while avoiding dislocation.
Pain control
To facilitate rehabilitation and prevent delirium, it is important to control the postoperative pain properly, eg, with a specific nerve block.
VTE prophylaxis
Patients with lower extremity fractures requiring treatment require deep vein prophylaxis.
The type and duration depend on VTE risk stratification.
Follow-up
Follow-up assessment for wound healing, neurologic status, function, and patient education should occur within 10–14 days.
Check the condition of the injury with appropriate x-rays at six weeks.
Longer follow-up, at 6 months and 1 year, is indicated to assess the development of posttraumatic arthritis and/or avascular necrosis.













