Excision
1. General considerations
Open capsulotomy vs arthroscopy
In most cases, as determined by a CT scan, osteochondral fragments are removed through a capsulotomy or arthroscopically.
The indication for arthroscopic removal depends on the surgeon’s skill with hip arthroscopy.
The advantages of hip arthroscopy are:
- Minimally invasive capsulotomy
- Enhanced visualization of the joint
- Visualization of the osteochondral defect in the head
The limitation of an arthroscopic approach is the ability to take out larger fragments.
The arthroscopic approach will need joint distraction (freehand or fracture table).

Treatment of hip dislocation
In general, fractures of the femoral head are associated with dislocation of the hip. In 90%, the dislocations are posterior and in 10% anterior.
An unreduced dislocation is an emergency because it threatens the blood supply to the head, and it may also be accompanied by pressure on a major nerve. Therefore, a reduction must be performed as an emergency.
If a closed reduction succeeds, one can investigate the patient further with a CT to develop an appropriate treatment rationale.
If a closed reduction fails, an emergency open reduction must be undertaken.
Imaging after hip reduction
After a closed reduction of the hip, an x-ray evaluation of the reduction is necessary.
Osteochondral fragments, their location, and incongruence of the femoral head and joint after dislocation may be overlooked on conventional x-rays. CT scans are always recommended.
2. Patient preparation and approaches
Approaches
For open procedures, the following approaches may be used:
3. Removal of fragments through open capsulotomy
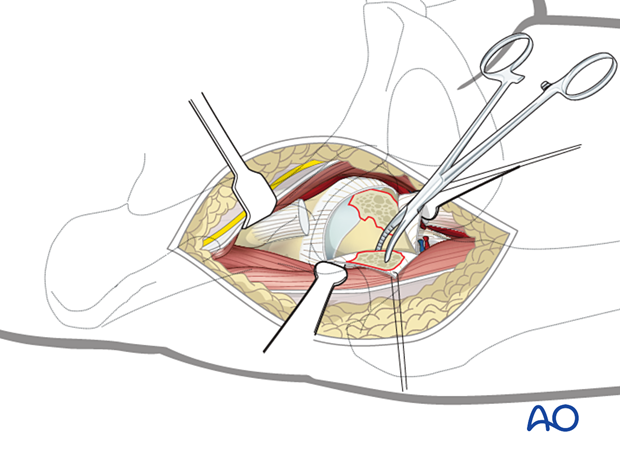
After the capsulotomy, irrigate the joint. Then remove large fragments using forceps, pituitary rongeurs, etc.
All fragments identified on the preoperative CT should be accounted for.
Subluxation by traction, with internal and external rotation, is useful for visualization of the joint and access to any trapped fragments.
Irrigation of the subluxed joint will often flush out smaller hidden fragments.
Confirm concentric reduction with image intensification.
4. Aftercare
Dislocation precautions
Since most femoral head fractures are associated with a hip dislocation, precautions against redislocation should be taken for the first 6 weeks after injury.
Low seats and toilets, flexing the hip when arising, sitting with legs crossed, as well as squatting and kneeling may also be avoided initially, as should pivoting on the affected leg. The patient and caregivers may be encouraged to use additional support when rising from a sitting position.
Postoperative mobilization
After excision, if the pain is tolerable, the patient starts with weight bearing as tolerated with walking aids.
Range-of-motion exercises should start cautiously in the immediate postoperative period to prevent stiffness while avoiding dislocation.

Pain control
To facilitate rehabilitation and prevent delirium, it is important to control the postoperative pain properly, eg, with a specific nerve block.
VTE prophylaxis
Patients with lower extremity fractures requiring treatment require deep vein prophylaxis.
The type and duration depend on VTE risk stratification.
Follow-up
Follow-up assessment for wound healing, neurologic status, function, and patient education should occur within 10–14 days.
Check the condition of the injury with appropriate x-rays at six weeks.
Longer follow-up, at 6 months and 1 year, is indicated to assess the development of posttraumatic arthritis and/or avascular necrosis.
Prognosis of proximal femoral fractures in elderly patients
For prognosis in elderly patients, see the corresponding additional material.













