Nonoperative
1. Introduction
The decision for operative or nonoperative treatment of pelvic ring injuries is based on:
- Fracture stability, displacement, and pattern
- Patient factors
- Surgical skill and availability of equipment
Pelvic ring stability is assessed by the type and location of fractures and joint injuries involving the pelvic ring.
2. Fractures of the innominate bone
These fractures are stable fractures and typically do not require operative treatment.
The exceptions are:
- selected apophyseal avulsions
- widely displaced extra articular fracture of the iliac crest.
In these cases reduction and internal fixation is performed.
Goal of treatment
The goals of nonoperative treatment are:
- Satisfactory fracture healing
- Recovery of function
- Patient comfort
- In an appropriate time frame
Mobilization
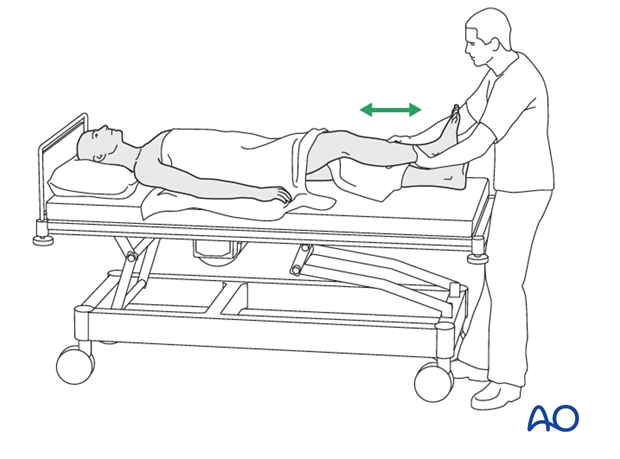
Mobilization can often begin early but should be individualized. Even in a bed bound patient, exercises to avoid stiffness and promote muscle function are advisable.
As soon as the patient is mobile enough, and comfortable enough, discharge from hospital should be possible and encouraged (depending upon other injuries).
Weight bearing
Weight bearing must be individualized but initial protection, using crutches or a walker, is advocated. This can be gradually decreased as comfort and healing permit.
Most of these pelvic fractures become increasingly stable by 6 weeks, and most are securely healed by 3 months. A helpful approach is to accept permissive weight bearing, permitting the patient to bear weight according to tolerance.

Rehabilitation
Outpatient rehabilitation should maintain and increase mobility and muscle strength. Contractures should be avoided.
Patients should be seen at 2 weeks, 6 weeks, and 3 months after injury. Follow up X-rays are obtained at these visits to assess fracture healing.
Large iliac wing fractures may develop progressive displacement and require ORIF.
Persistent pain
Patients with persistent pain (especially low back pain), require special attention to exclude undiagnosed unstable fracture patterns, and/or nonunions. If pain has not resolved by 3 months or more, CT scans or other advanced imaging may be advisable.
3. Sacral fractures
Local pain and tenderness can be significant and interfere with sitting. Walking and standing as well as bed bound activities will soon become tolerable.
Coccygeal fractures and dislocations
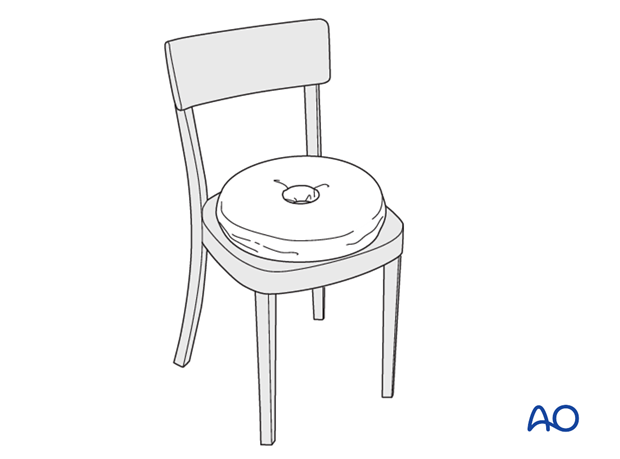
Coccygeal fractures and dislocations usually have little deformity. If there is significant angulation, closed reduction with local anaesthesia and digital intra-anal manipulation may be considered. The use of a donut cushion (central hollow area) or other pillow for sitting is usually helpful.
Undisplaced lower sacral fractures
Undisplaced lower sacral fractures will not require reduction but a donut cushion will relieve pain during sitting.
Displaced lower sacral fractures
Displaced lower sacral fractures may compromise sacral plexus neurologic function which should be assessed to exclude the need for surgery. If the patient is neurologically normal and deformity is acceptable, activities can be allowed as tolerated with cushions for sitting.













