ORIF - Anterior SI fracture fixation
1. Introduction
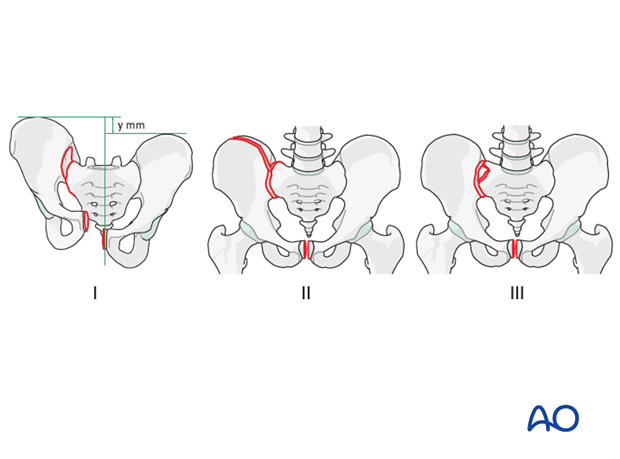
Types of sacroiliac joint instability
Sacroiliac joint instability may be produced by pure dislocations (I), or fracture dislocations involving either the ilium (II) or the sacrum (III)
Instability of the sacroiliac joint occurs most commonly with a pure disruption of the sacroiliac joint.
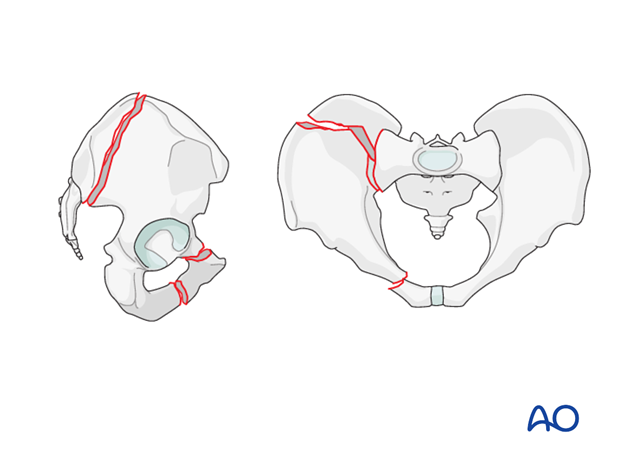
Crescent fracture-dislocation
A crescent fracture is a fracture dislocation of the SI joint.
This injury involves a ligamentous disruption of the inferior part of the SI joint, and a vertical fracture of the posterior ilium that extends from the SI joint and exits the iliac crest.
The posterior superior iliac spine remains firmly attached to the sacrum via the superior portion of the posterior ligamentous complex.
The remaining anterior fragment is more mobile to internal rotation but remains relatively stable to external rotation and vertical forces.
This fracture is always combined with an injury to the anterior pelvis, most often fractures of the pubic rami.
These fractures are unstable.
2. Patient preparation and approach
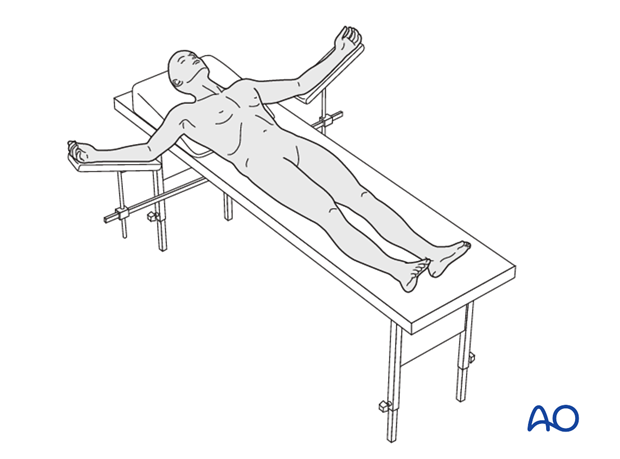
Patient preparation
This procedure is performed with the patient in a supine position.
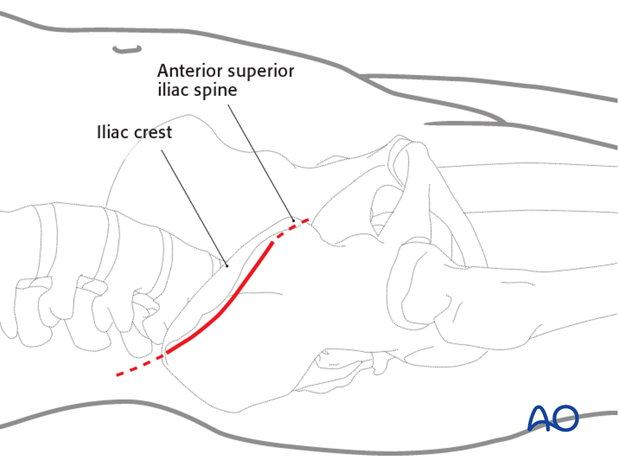
Approach
For this procedure an anterior approach to the iliac wing and SI joint is used.
3. Cleaning of the fracture site
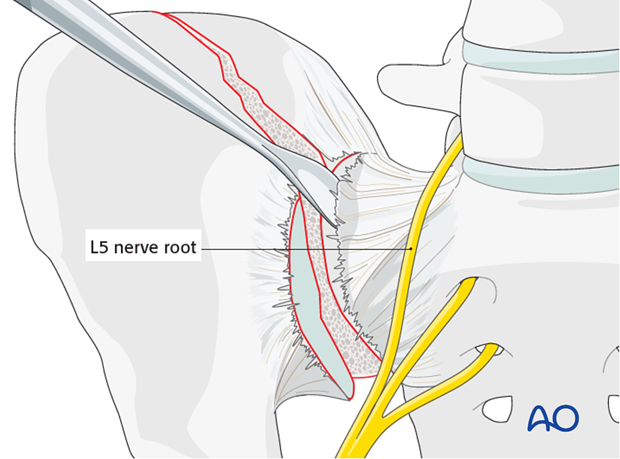
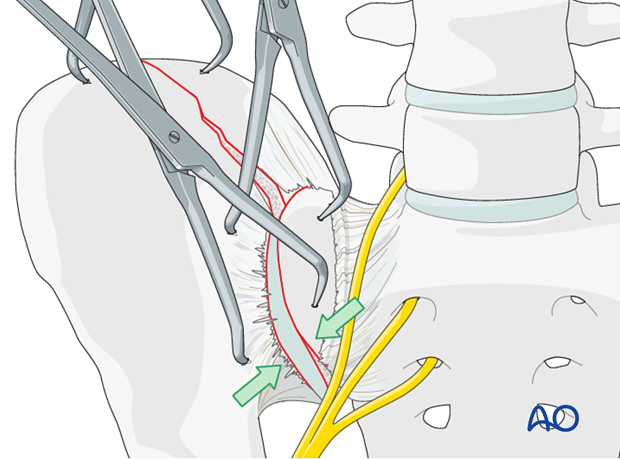
Elevation of the sacroiliac ligament
Use a Cobb elevator to elevate the anterior fibers of the sacroiliac ligament from the sacrum. Further medial dissection must respect the L5 nerve root but can be extended 1-2 cm and should be subperiosteal.
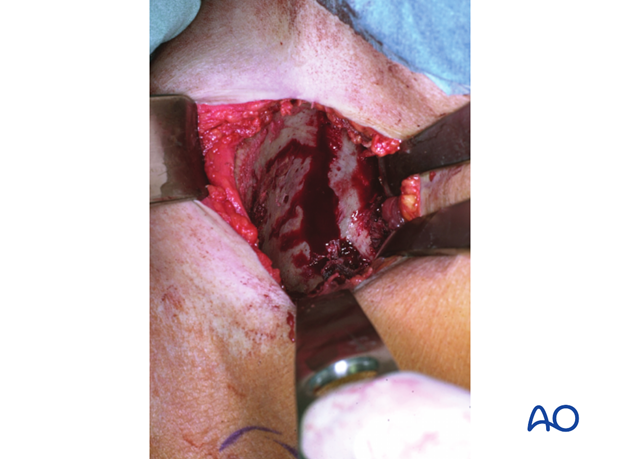
Intraoperative view
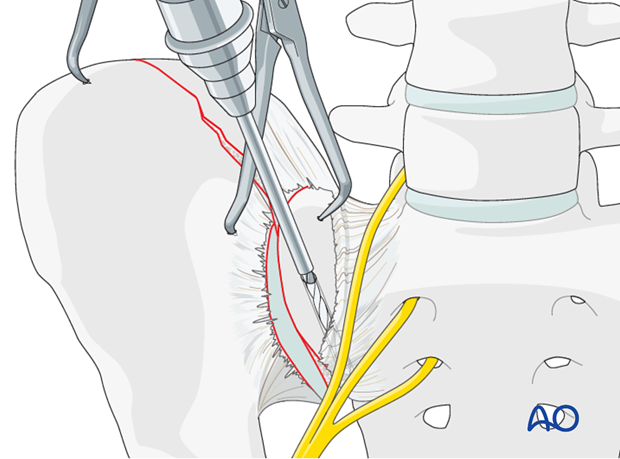
Prepare the sacral screw insertion
Insert sharp Hohmann retractors posteriorly and anteriorly into the sacrum to expose approximately 1-2 cm of the lateral section of the sacrum for later screw positioning.
The pointed tips of these retractors may be gently impacted into the bone of the sacral ala.
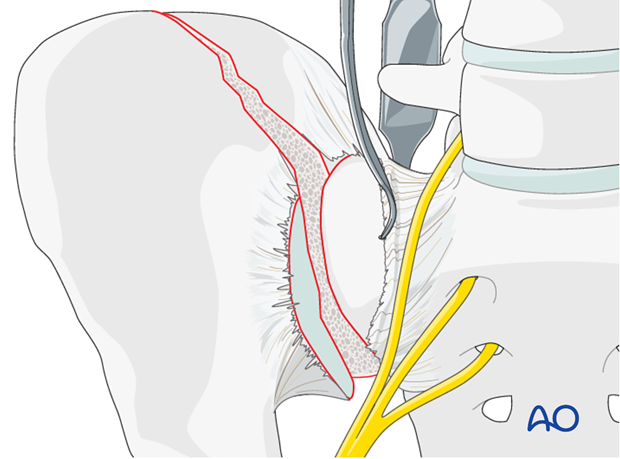
The SI joint is distracted using a laminar spreader. The joint is inspected, irrigated, and small fragments are removed.
4. Reduction
Reduction techniques
Reduction is performed using the following techniques:
- Applying manual lateral compression
- Use of longitudinal traction
- Use of pointed reduction forceps applied on the iliac crest.
- Use of pointed reduction forceps applied on the sacrum
- Use of a Jungbluth or Farabeuf clamp applied across the sacroiliac joint.

Additional pointed reduction forceps may be applied when necessary to reduce the joint.
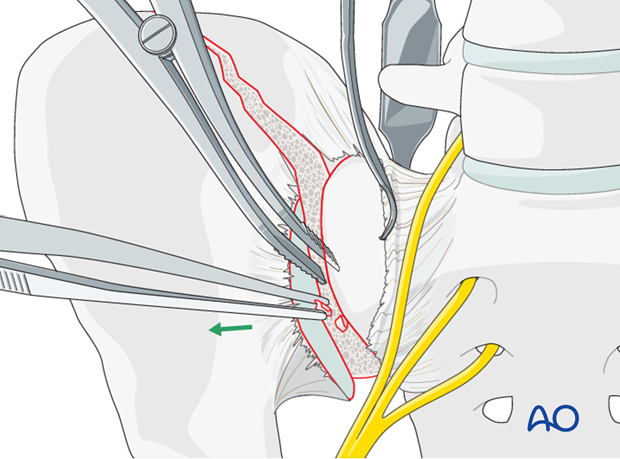
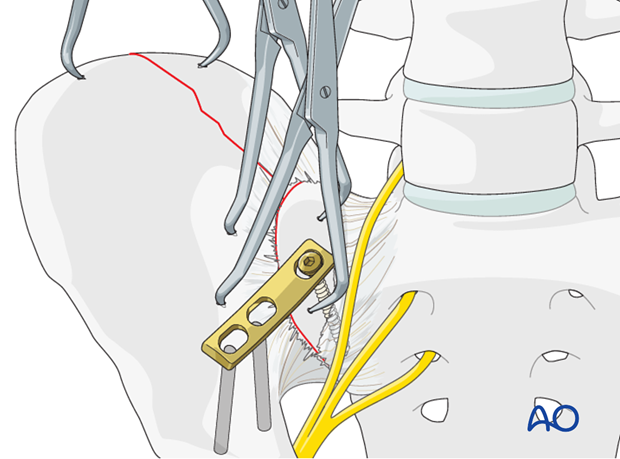
Reduction using a Farabeuf or Jungbluth clamp
In order to apply the Farabeuf or Jungbluth clamp a screw is placed into the sacral ala. First, the drill hole is made. The drill is placed parallel to the SI joint under direct vision.
These screws are usually 50-60 mm in length.
There is a limited area (approximately 1-2 cm medial to the SI joint) that allows for safe placement of screws in the sacral ala, due to the proximity of the L5 nerve root.
Insert a screw into the sacral ala using the previously drilled hole. A second hole is drilled in the ilium just lateral to the sacroiliac joint. Insert a second screw into this hole.
These screws should be placed in the central portion of the sacroiliac joint (from anterior to posterior) in order to leave room for plate(s) anteriorly and in some cases posteriorly to the reduction screws.
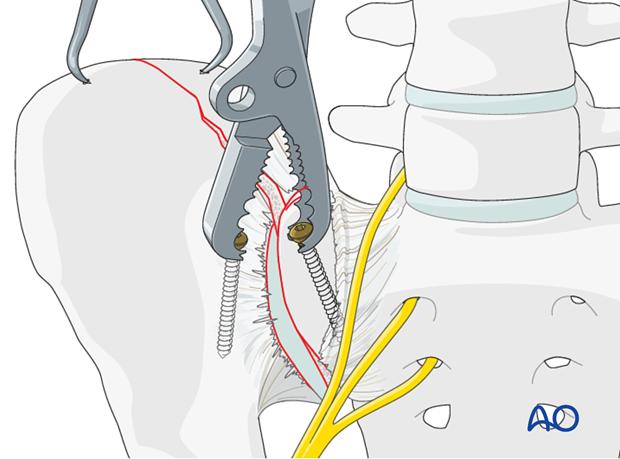
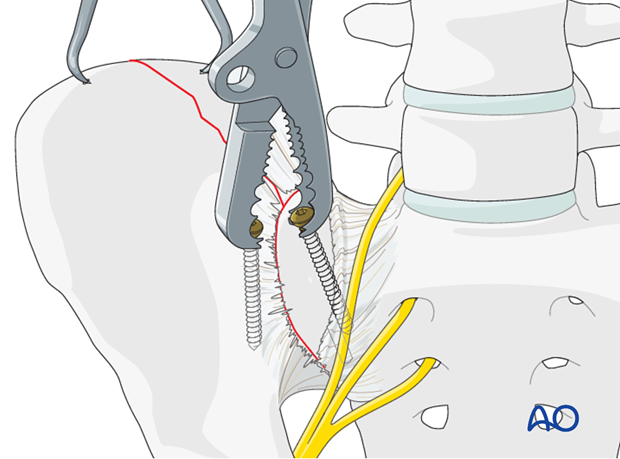
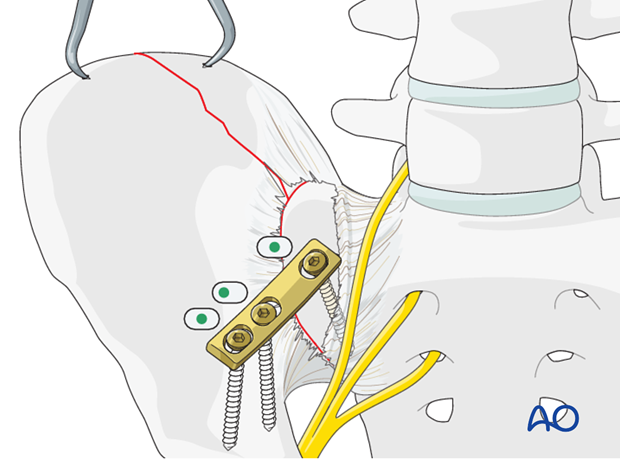
Next, apply a Farabeuf or Jungbluth clamp to these screws. The clamp can then be used to reduce the sacroiliac joint. The clamp allows for reduction in multiple planes.
Anatomic reduction should be confirmed by direct visualization and verified by image intensification.
5. Fixation
Drilling of the sacral screw
Drill a hole in the lateral part of the sacrum (close to the linea terminalis) directly parallel to the SI-joint using a 3.2 mm drill bit.
Alternatively small fragment plates may be considered.
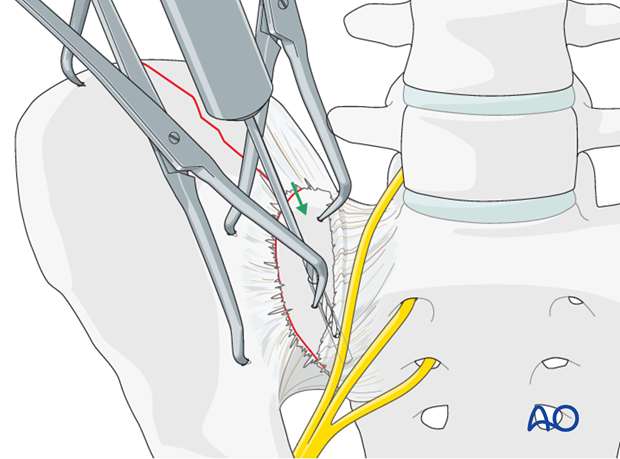
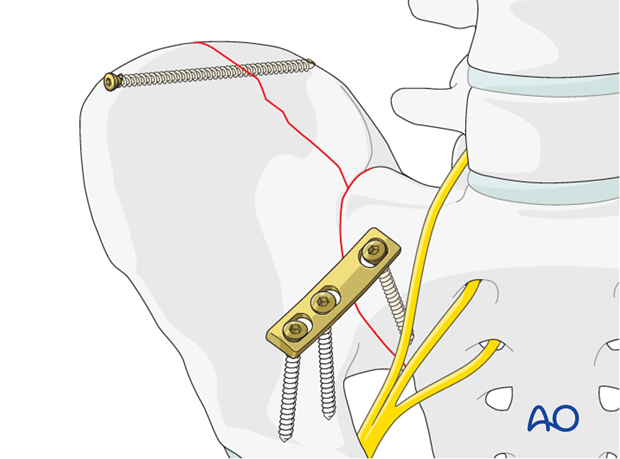
Plate application
Apply a 4.5 mm 3-hole DC-plate for dynamic compression.
The plates are contoured using a table top bending press. The plates are contoured to fit across the SI joint with one screw in the sacrum and two in the ilium.

Precontour the plate in the direction of the pelvic brim (linea terminalis) and apply the cortical, sacral screw.
The sacral screw hole is drilled carefully, to avoid injury to the lumbosacral nerve trunk but not enter the sloping SI joint. This screw is inserted and tightened in the neutral position.
The medial iliac screw is inserted in compression. Then the lateral screw is inserted in neutral.
Screw fixation of the iliac crest
The fracture of the ilium is stabilized with a 3.5 mm intramedullary screw
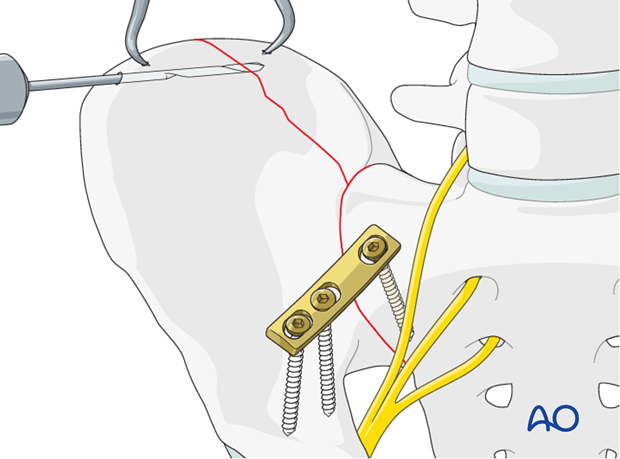
Repeat this procedure for insertion of a second screw, if needed.
X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.

6. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













